J Korean Ophthalmol Soc.
2019 Sep;60(9):896-900. 10.3341/jkos.2019.60.9.896.
Fulminant Toxoplasmic Chorioretinitis Following Intravitreal Dexamethasone Implantation
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. msagong@ynu.ac.kr
- KMID: 2459136
- DOI: http://doi.org/10.3341/jkos.2019.60.9.896
Abstract
- PURPOSE
To report a case of fulminant toxoplasmic chorioretinitis following intravitreal dexamethasone implantation monotherapy in a stabilized toxoplasmic chorioretinitis patient with initial treatment.
CASE SUMMARY
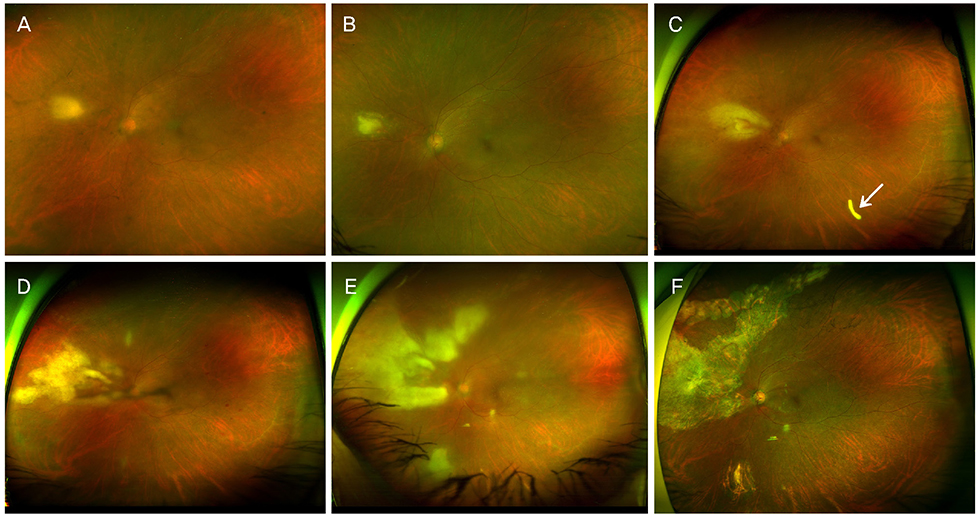
A 60-year-old healthy female presented with decreased visual acuity in the left eye. On fundus examination, focal chorioretinitis and yellow-white infiltration were observed. Laboratory work-up, including blood chemistry, complete blood count, and serum serology, was negative; however, toxoplasmic chorioretinitis could not be ruled out. The primary lesion improved with antibiotics and prednisolone treatment. However, the patient did not come in for her follow-up visit, as she had already received an intravitreal dexamethasone implant for recurrent vitreous inflammation elsewhere. On her return, she presented with necrotic retinitis with extensive infiltration. She underwent diagnostic vitrectomy and implant removal. A diagnosis of toxoplasma antigen was confirmed by polymerase chain reaction analysis; the lesions stabilized after anti-toxoplasmic therapy.
CONCLUSIONS
Intravitreal dexamethasone implant monotherapy with stabilized toxoplasmic chorioretinitis without systemic antibiotics can lead to fulminant toxoplasmic chorioretinitis and should be used with caution.
Keyword
MeSH Terms
Figure
Reference
-
1. Cunningham ET Jr, Belfort R Jr, Muccioli C, et al. Ocular toxoplasmosis. Ocul Immunol Inflamm. 2015; 23:191–193.
Article2. Park YH, Han JH, Nam HW. Clinical features of ocular toxoplasmosis in Korean patients. Korean J Parasitol. 2011; 49:167–171.
Article3. Rothova A, Meenken C, Buitenhuis HJ, et al. Therapy for ocular toxoplasmosis. Am J Ophthalmol. 1993; 115:517–523.
Article4. Park YH, Nam HW. Clinical features and treatment of ocular toxoplasmosis. Korean J Parasitol. 2013; 51:393–399.
Article5. Holland G, Lewis K. An update on current practices in the management of ocular toxoplasmosis. Am J Ophthalmol. 2002; 134:102–114.6. Oray M, Ozdal PC, Cebeci Z, et al. Fulminant ocular toxoplasmosis: the hazards of corticosteroid monotherapy. Ocul Immunol Inflamm. 2016; 24:637–646.
Article7. Papadia M, Aldigeri R, Herbort CP. The role of serology in active ocular toxoplasmosis. Int Ophthalmol. 2011; 31:461–465.
Article8. Suresh S, Nor-Masniwati S, Nor-Idahriani MN, et al. Serological IgG avidity test for ocular toxoplasmosis. Clin Ophthalmol. 2012; 6:147–150.9. De Groot-Mijnes JD, Rothova A, Van Loon AM, et al. Polymerase chain reaction and Goldmann-Witmer coefficient analysis are complimentary for the diagnosis of infectious uveitis. Am J Ophthalmol. 2006; 141:313–318.
Article10. Sugita S, Ogawa M, Inoue S, et al. Diagnosis of ocular toxoplasmosis by two polymerase chain reaction (PCR) examinations: qualitative multiplex and quantitative real-time. Jpn J Ophthalmol. 2011; 55:495–501.
Article11. Takakura A, Tessler HH, Goldstein DA, et al. Viral retinitis following intraocular or periocular corticosteroid administration: a case series and comprehensive review of the literature. Ocul Immunol Inflamm. 2014; 22:175–182.
Article12. Backhouse O, Bhan K, Bishop F. Intravitreal triamcinolone acetonide as an adjunct in the treatment of severe ocular toxoplasmosis. Eye (Lond). 2008; 22:1201–1202.
Article13. Zamora YF, Arantes T, Reis FA, et al. Local treatment of toxoplasmic retinochoroiditis with intravitreal clindamycin and dexamethasone. Arq Bras Oftalmol. 2015; 78:216–219.
Article14. O'Connor GR, Frenkel JK. Editorial: dangers of steroid treatment in toxoplasmosis. periocular injections and systemic therapy. Arch Ophthalmol. 1976; 94:213.15. Rush R, Sheth S. Fulminant toxoplasmic retino-choroiditis following intravitreal triamcinolone administration. Indian J Ophthalmol. 2012; 60:141–143.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraocular Pressure Elevation after 0.7 mg Intravitreal Dexamethasone (Ozurdex(R)) Implantation: A One Year Follow-Up
- A Case of Repeated Intravitreal Dexamethasone Implantation for Treatment of Macular Edema after Scleral Fixation of Intraocular Lens
- A Case of Retinal Hemorrhage Following a Dexamethasone Intravitreal Implant
- The Effect of Prophylactic IOP-Lowering Medication after Intravitreal Dexamethasone Implantation
- A Case of Intravitreal Dexamethasone Implantation in a Patient with Vogt-Koyanagi-Harada Disease