J Periodontal Implant Sci.
2019 Aug;49(4):258-267. 10.5051/jpis.2019.49.4.258.
Assessment of stem cell viability in the initial healing period in rabbits with a cranial bone defect according to the type and form of scaffold
- Affiliations
-
- 1Department of Dental Implantology, The Catholic University of Korea Graduate School of Clinical Dental Science, Seoul, Korea. omskim@catholic.ac.kr
- 2Department of Periodontics, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 3Department of Oral and Maxillofacial Surgery, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 4Institute of Foreign Language Studies, Korea University, Seoul, Korea.
- 5The Faculty of Liberal Arts, Eulji University, Seongnam, Korea.
- KMID: 2455803
- DOI: http://doi.org/10.5051/jpis.2019.49.4.258
Abstract
- PURPOSE
Increased bone regeneration has been achieved through the use of stem cells in combination with graft material. However, the survival of transplanted stem cells remains a major concern. The purpose of this study was to evaluate the viability of transplanted mesenchymal stem cells (MSCs) at an early time point (24 hours) based on the type and form of the scaffold used, including type I collagen membrane and synthetic bone.
METHODS
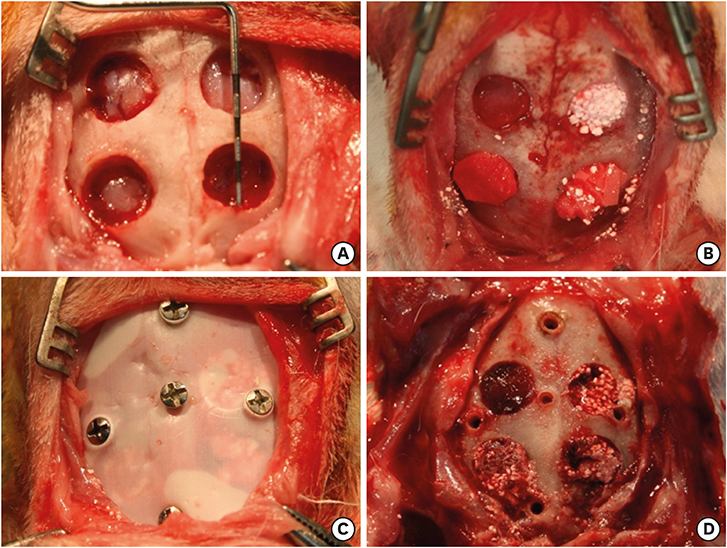
The stem cells were obtained from the periosteum of the otherwise healthy dental patients. Four symmetrical circular defects measuring 6 mm in diameter were made in New Zealand white rabbits using a trephine drill. The defects were grafted with 1) synthetic bone (β-tricalcium phosphate/hydroxyapatite [β-TCP/HA]) and 1×105 MSCs, 2) collagen membrane and 1×105 MSCs, 3) β-TCP/HA+collagen membrane and 1×105 MSCs, or 4) β-TCP/HA, a chipped collagen membrane and 1×105 MSCs. Cellular viability and the cell migration rate were analyzed.
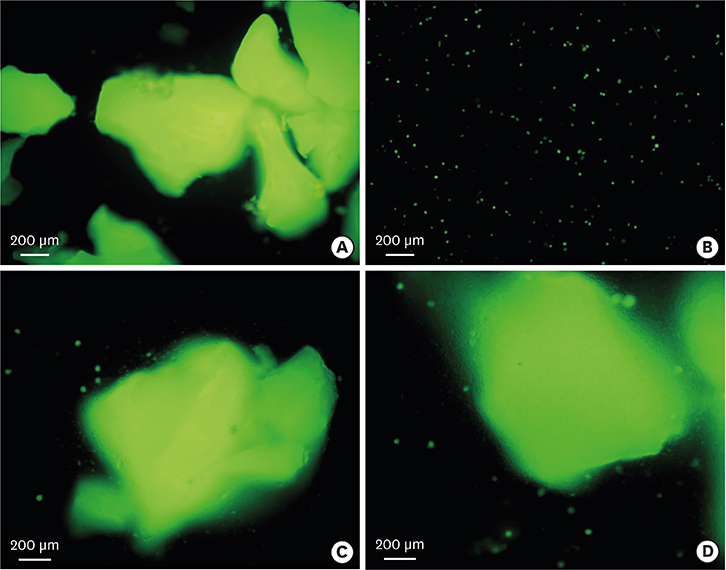
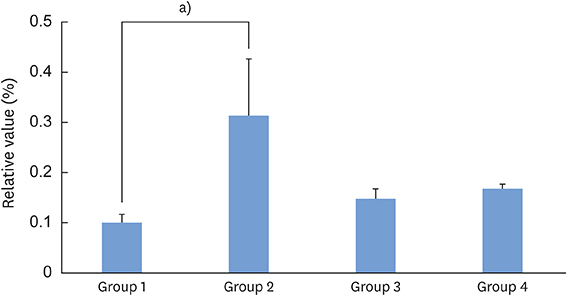
RESULTS
Cells were easily separated from the collagen membrane, but not from synthetic bone. The number of stem cells attached to synthetic bone in groups 1, 3, and 4 seemed to be similar. Cellular viability in group 2 was significantly higher than in the other groups (P<0.05). The cell migration rate was highest in group 2, but this difference was not statistically significant (P>0.05).
CONCLUSIONS
This study showed that stem cells can be applied when a membrane is used as a scaffold under no or minimal pressure. When space maintenance is needed, stem cells can be loaded onto synthetic bone with a chipped membrane to enhance the survival rate.
MeSH Terms
Figure
Reference
-
1. Wang W, Yeung KW. Bone grafts and biomaterials substitutes for bone defect repair: a review. Bioact Mater. 2017; 2:224–247.
Article2. Kubota T, Hasuike A, Ozawa Y, Yamamoto T, Tsunori K, Yamada Y, et al. Regenerative capacity of augmented bone in rat calvarial guided bone augmentation model. J Periodontal Implant Sci. 2017; 47:77–85.
Article3. Fernández-Domínguez M, Ortega-Asensio V, Fuentes-Numancia E, Aragoneses JM, Barbu HM, Ramírez-Fernández MP, et al. Can the macrogeometry of dental implants influence guided bone regeneration in buccal bone defects? Histomorphometric and biomechanical analysis in beagle dogs. J Clin Med. 2019; 8:8.
Article4. Ohta K, Tada M, Ninomiya Y, Kato H, Ishida F, Abekura H, et al. Application of interconnected porous hydroxyapatite ceramic block for onlay block bone grafting in implant treatment: a case report. Exp Ther Med. 2017; 14:5564–5568.5. Bertolai R, Catelani C, Aversa A, Rossi A, Giannini D, Bani D. Bone graft and mesenchimal stem cells: clinical observations and histological analysis. Clin Cases Miner Bone Metab. 2015; 12:183–187.
Article6. Park JB, Cho SH, Kim I, Lee W, Kang SH, Kim H. Evaluation of the bisphosphonate effect on stem cells derived from jaw bone and long bone rabbit models: a pilot study. Arch Oral Biol. 2018; 85:178–182.
Article7. Tae JY, Lee H, Lee H, Ko Y, Park JB. Osteogenic potential of cell spheroids composed of varying ratios of gingiva-derived and bone marrow stem cells using concave microwells. Exp Ther Med. 2018; 16:2287–2294.
Article8. Namli H, Erdogan Ö, Gönlüşen G, Kahraman OE, Aydin HM, Karabag S, et al. Vertical bone augmentation using bone marrow-derived stem cells: an in vivo study in the rabbit calvaria. Implant Dent. 2016; 25:54–62.9. Khadka A, Li J, Li Y, Gao Y, Zuo Y, Ma Y. Evaluation of hybrid porous biomimetic nano-hydroxyapatite/polyamide 6 and bone marrow-derived stem cell construct in repair of calvarial critical size defect. J Craniofac Surg. 2011; 22:1852–1858.
Article10. Daei-Farshbaf N, Ardeshirylajimi A, Seyedjafari E, Piryaei A, Fadaei Fathabady F, Hedayati M, et al. Bioceramic-collagen scaffolds loaded with human adipose-tissue derived stem cells for bone tissue engineering. Mol Biol Rep. 2014; 41:741–749.
Article11. Yang P, Huang X, Wang C, Dang X, Wang K. Repair of bone defects using a new biomimetic construction fabricated by adipose-derived stem cells, collagen I, and porous beta-tricalcium phosphate scaffolds. Exp Biol Med (Maywood). 2013; 238:1331–1343.
Article12. Sándor GK, Tuovinen VJ, Wolff J, Patrikoski M, Jokinen J, Nieminen E, et al. Adipose stem cell tissue-engineered construct used to treat large anterior mandibular defect: a case report and review of the clinical application of good manufacturing practice-level adipose stem cells for bone regeneration. J Oral Maxillofac Surg. 2013; 71:938–950.
Article13. Zamiri B, Shahidi S, Eslaminejad MB, Khoshzaban A, Gholami M, Bahramnejad E, et al. Reconstruction of human mandibular continuity defects with allogenic scaffold and autologous marrow mesenchymal stem cells. J Craniofac Surg. 2013; 24:1292–1297.
Article14. Kim SJ, Kim MR, Oh JS, Han I, Shin SW. Effects of polycaprolactone-tricalcium phosphate, recombinant human bone morphogenetic protein-2 and dog mesenchymal stem cells on bone formation: pilot study in dogs. Yonsei Med J. 2009; 50:825–831.
Article15. Wu H, Liu GH, Wu Q, Yu B. Repairing rabbit radial defects by combining bone marrow stroma stem cells with bone scaffold material comprising a core-cladding structure. Genet Mol Res. 2015; 14:11933–11943.
Article16. Yang DJ, Jeon JH, Lee SY, An HW, Park KO, Park KB, et al. Effects of collagen grafting on cell behaviors in BCP scaffold with interconnected pore structure. Biomater Res. 2016; 20:3.
Article17. Villa MM, Wang L, Rowe DW, Wei M. Effects of cell-attachment and extracellular matrix on bone formation in vivo in collagen-hydroxyapatite scaffolds. PLoS One. 2014; 9:e109568.18. Koury MJ, Bondurant MC. Maintenance by erythropoietin of viability and maturation of murine erythroid precursor cells. J Cell Physiol. 1988; 137:65–74.
Article19. Piltti KM, Avakian SN, Funes GM, Hu A, Uchida N, Anderson AJ, et al. Transplantation dose alters the dynamics of human neural stem cell engraftment, proliferation and migration after spinal cord injury. Stem Cell Res (Amst). 2015; 15:341–353.
Article20. Zhang H, Chen H, Wang W, Wei Y, Hu S. Cell survival and redistribution after transplantation into damaged myocardium. J Cell Mol Med. 2010; 14:1078–1082.
Article21. Alfotawei R, Naudi KB, Lappin D, Barbenel J, Di Silvio L, Hunter K, et al. The use of TriCalcium Phosphate (TCP) and stem cells for the regeneration of osteoperiosteal critical-size mandibular bony defects, an in vitro and preclinical study. J Craniomaxillofac Surg. 2014; 42:863–869.
Article22. Wu G, Pan M, Wang X, Wen J, Cao S, Li Z, et al. Osteogenesis of peripheral blood mesenchymal stem cells in self assembling peptide nanofiber for healing critical size calvarial bony defect. Sci Rep. 2015; 5:16681.
Article23. Jäger M, Degistirici O, Knipper A, Fischer J, Sager M, Krauspe R. Bone healing and migration of cord blood-derived stem cells into a critical size femoral defect after xenotransplantation. J Bone Miner Res. 2007; 22:1224–1233.
Article24. Berardinelli P, Valbonetti L, Muttini A, Martelli A, Peli R, Zizzari V, et al. Role of amniotic fluid mesenchymal cells engineered on MgHA/collagen-based scaffold allotransplanted on an experimental animal study of sinus augmentation. Clin Oral Investig. 2013; 17:1661–1675.
Article25. Robey TE, Saiget MK, Reinecke H, Murry CE. Systems approaches to preventing transplanted cell death in cardiac repair. J Mol Cell Cardiol. 2008; 45:567–581.
Article26. Amini AR, Laurencin CT, Nukavarapu SP. Bone tissue engineering: recent advances and challenges. Crit Rev Biomed Eng. 2012; 40:363–408.
Article27. Somaiah C, Kumar A, Mawrie D, Sharma A, Patil SD, Bhattacharyya J, et al. Collagen promotes higher adhesion, survival and proliferation of mesenchymal stem cells. PLoS One. 2015; 10:e0145068.
Article28. Neuss S, Stainforth R, Salber J, Schenck P, Bovi M, Knüchel R, et al. Long-term survival and bipotent terminal differentiation of human mesenchymal stem cells (hMSC) in combination with a commercially available three-dimensional collagen scaffold. Cell Transplant. 2008; 17:977–986.
Article29. Tiwari S, Patil R, Bahadur P. Polysaccharide based scaffolds for soft tissue engineering applications. Polymers (Basel). 2018; 11:11.
Article30. Linero I, Chaparro O. Paracrine effect of mesenchymal stem cells derived from human adipose tissue in bone regeneration. PLoS One. 2014; 9:e107001.
Article31. Deb A. How stem cells turn into bone and fat. N Engl J Med. 2019; 380:2268–2270.
Article32. Robey PG. Cell sources for bone regeneration: the good, the bad, and the ugly (but promising). Tissue Eng Part B Rev. 2011; 17:423–430.
Article33. Lawrence LM, Cottrill A, Valluri A, Marenzi G, Denning KL, Valluri J, et al. Minimally manipulative method for the expansion of human bone marrow mesenchymal stem cells to treat osseous defects. Int J Mol Sci. 2019; 20:20.
Article34. Dow J, Simkhovich BZ, Kedes L, Kloner RA. Washout of transplanted cells from the heart: a potential new hurdle for cell transplantation therapy. Cardiovasc Res. 2005; 67:301–307.
Article35. Murphy KC, Hughbanks ML, Binder BY, Vissers CB, Leach JK. Engineered fibrin gels for parallel stimulation of mesenchymal stem cell proangiogenic and osteogenic potential. Ann Biomed Eng. 2015; 43:2010–2021.
Article36. Moshaverinia A, Chen C, Xu X, Akiyama K, Ansari S, Zadeh HH, et al. Bone regeneration potential of stem cells derived from periodontal ligament or gingival tissue sources encapsulated in RGD-modified alginate scaffold. Tissue Eng Part A. 2014; 20:611–621.
Article37. Murphy KC, Fang SY, Leach JK. Human mesenchymal stem cell spheroids in fibrin hydrogels exhibit improved cell survival and potential for bone healing. Cell Tissue Res. 2014; 357:91–99.
Article38. Scarfì S. Use of bone morphogenetic proteins in mesenchymal stem cell stimulation of cartilage and bone repair. World J Stem Cells. 2016; 8:1–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous healing capacity of rabbit cranial defects of various sizes
- Repair of Cartilage Defect by Cultured Mesenchymal Stem Cells from Bone Marrow
- Mesenchymal Stem Cells of Different Origin-Seeded Bioceramic Construct in Regeneration of Bone Defect in Rabbit
- Bone regeneration of mouse critical-sized calvarial defects with human mesenchymal stem cells in scaffold
- An Experimental Study of the Effect of plaster of Paris on the Bone Defects of Adult Rabbits