Intest Res.
2019 Jul;17(3):317-329. 10.5217/ir.2019.00021.
Prevalence and risk factors of colorectal cancer in Asia
- Affiliations
-
- 1Jockey Club School of Public Health and Primary Care, Faculty of Medicine, Chinese University of Hong Kong, Hong Kong Special Administrative Region, China. wong_martin@cuhk.edu.hk
- KMID: 2454740
- DOI: http://doi.org/10.5217/ir.2019.00021
Abstract
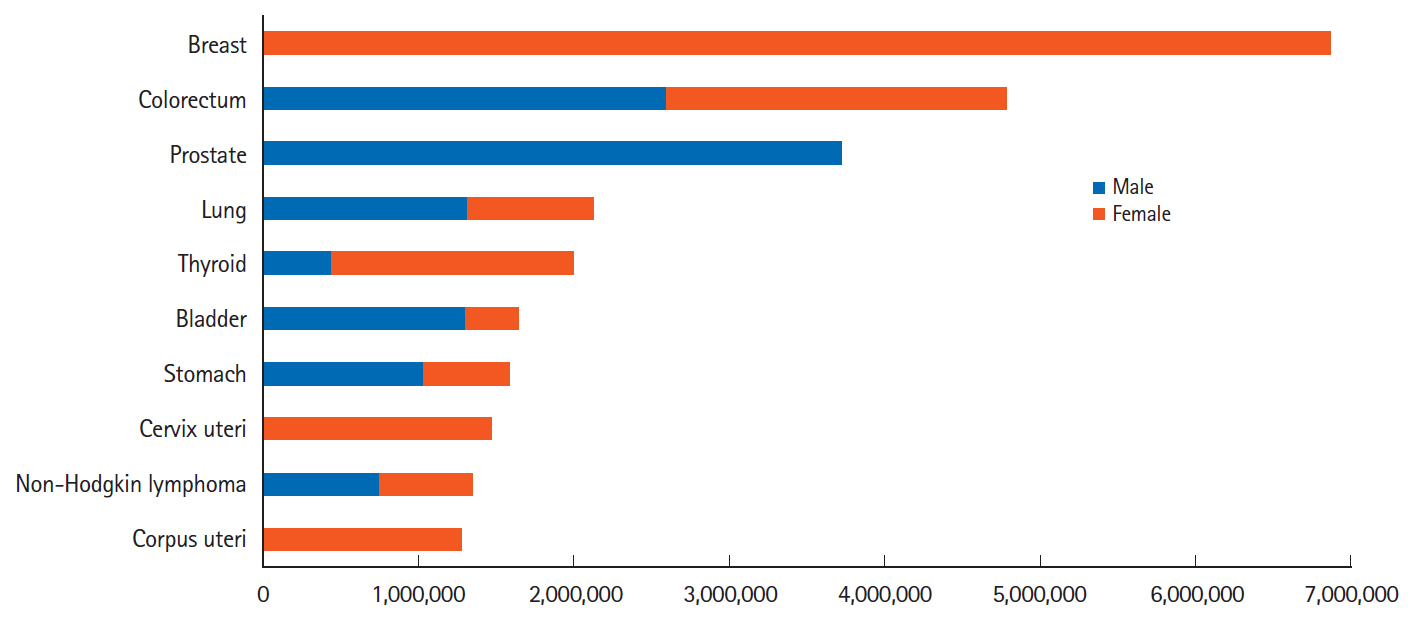
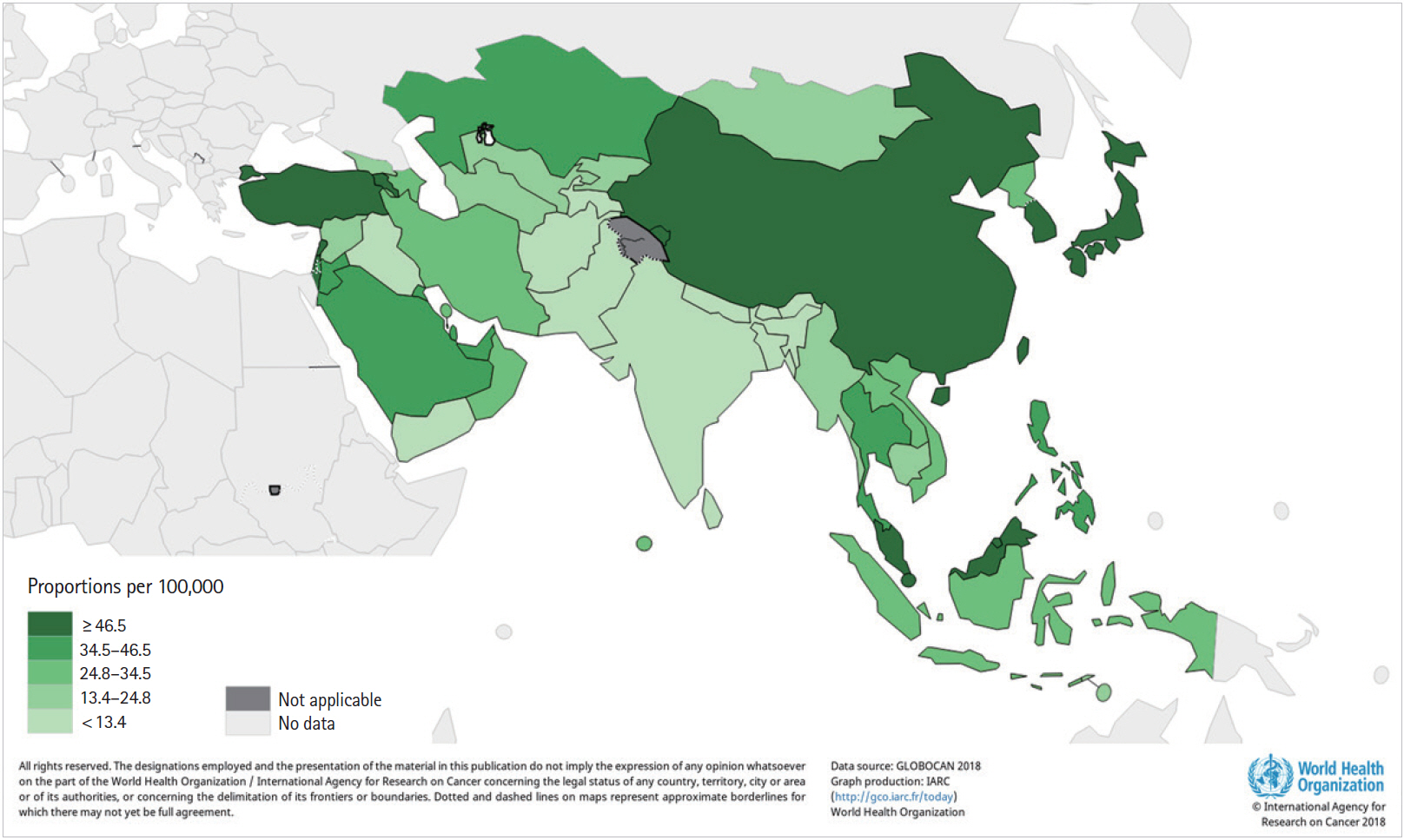
- Globally, colorectal cancer (CRC) is a substantial public health burden, and it is increasingly affecting populations in Asian countries. The overall prevalence of CRC is reported to be low in Asia when compared with that in Western nations, yet it had the highest number of prevalent cases. This review described the prevalence of CRC in Asia according to the International Agency for Research on Cancer from World Health Organization (WHO) database and summarized its major risk factors. Non-modifiable factors include genetic factors, ethnicity, age, gender, family history and body height; smoking, alcohol drinking, weight, Westernized diet, physical inactivity, chronic diseases and microbiota were involved in environmental factors. These risk factors were separately discussed in this review according to published literature from Asian countries. CRC screening has been playing an important role in reducing its disease burden. Some recommendations on its screening practices have been formulated in guidelines for Asia Pacific countries.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical outcomes of submucosal colorectal cancer diagnosed after endoscopic resection: a focus on the need for surgery
Yun Sik Choi, Wan Soo Kim, Sung Wook Hwang, Sang Hyoung Park, Dong-Hoon Yang, Byong Duk Ye, Seung-Jae Myung, Suk-Kyun Yang, Jeong-Sik Byeon
Intest Res. 2020;18(1):96-106. doi: 10.5217/ir.2019.00092.
Reference
-
1. World Health Organization (WHO). Cancer. WHO Web site. https://www.who.int/news-room/fact-sheets/detail/cancer. Updated September 12, 2018. Accessed January 21, 2019.2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article3. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; 69:7–34.
Article4. International Agency for Research on Cancer WHO. Cancer today. IARC Web site. https://gco.iarc.fr/today/. Accessed January 21, 2019.5. Jasperson KW, Tuohy TM, Neklason DW, Burt RW. Hereditary and familial colon cancer. Gastroenterology. 2010; 138:2044–2058.
Article6. Migliore L, Migheli F, Spisni R, Coppedè F. Genetics, cytogenetics, and epigenetics of colorectal cancer. J Biomed Biotechnol. 2011; 2011:792362.
Article7. World Cancer Research Fund International. Diet, nutrition, physical activity and cancer. https://www.wcrf.org/sites/default/files/Summary-third-expert-report.pdf. Accessed May 10, 2019.8. Aune D, Chan DS, Lau R, et al. Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2011; 343:d6617.
Article9. Perera PS, Thompson RL, Wiseman MJ. Recent evidence for colorectal cancer prevention through healthy food, nutrition, and physical activity: implications for recommendations. Curr Nutr Rep. 2012; 1:44–54.
Article10. Aune D, Lau R, Chan DS, et al. Dairy products and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Ann Oncol. 2012; 23:37–45.
Article11. Vieira AR, Abar L, Chan DS, et al. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRFAICR Continuous Update Project. Ann Oncol. 2017; 28:1788–1802.
Article12. Chan DS, Lau R, Aune D, et al. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS One. 2011; 6:e20456.
Article13. Abar L, Vieira AR, Aune D, et al. Height and body fatness and colorectal cancer risk: an update of the WCRF-AICR systematic review of published prospective studies. Eur J Nutr. 2018; 57:1701–1720.
Article14. Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer. 2009; 125:171–180.
Article15. American Cancer Society. About colorectal cancer. American Cancer Society Web site. https://www.cancer.org/content/dam/CRC/PDF/Public/8604.00.pdf. Updated February 21, 2018. Accessed February 13, 2019.16. Hong Kong Cancer Registry. Overview of Hong Kong cancer statistics of 2016. Hospital Authority Web site. http://www3.ha.org.hk/cancereg/pdf/overview/Summary of CanStat 2016.pdf. Updated October 2018. Accessed February 12, 2019.17. Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017; 66:683–691.
Article18. Byeon JS, Yang SK, Kim TI, et al. Colorectal neoplasm in asymptomatic Asians: a prospective multinational multicenter colonoscopy survey. Gastrointest Endosc. 2007; 65:1015–1022.
Article19. Nam YJ, Kim KO, Park CS, Lee SH, Jang BI. Clinicopathological features of colorectal polyps in 2002 and 2012. Korean J Intern Med. 2019; 34:65–71.
Article20. Kashfi SM, Nazemalhosseini Mojarad E, Pourhoseingholi MA, Asadzadeh Aghdaei H, Anaraki F, Zali MR. Evaluation of the left-to-right shift of colon tumors in Iran: is the trend changing? J Res Med Sci. 2015; 20:978–986.
Article21. Zhou H, Shen Z, Zhao J, Zhou Z, Xu Y. Distribution characteristics and risk factors of colorectal adenomas. Zhonghua Wei Chang Wai Ke Za Zhi. 2018; 21:678–684.22. Senore C, Bellisario C, Segnan N. Distribution of colorectal polyps: implications for screening. Best Pract Res Clin Gastroenterol. 2017; 31:481–488.
Article23. Cha JM, Kozarek RA, La Selva D, et al. Disparities in prevalence, location, and shape characteristics of colorectal neoplasia between South Korean and U.S. patients. Gastrointest Endosc. 2015; 82:1080–1086.
Article24. Lee SY, Song WH, Oh SC, Min BW, Lee SI. Anatomical distribution and detection rate of colorectal neoplasms according to age in the colonoscopic screening of a Korean population. Ann Surg Treat Res. 2018; 94:36–43.
Article25. Iida Y, Kawai K, Tsuno NH, et al. Proximal shift of colorectal cancer along with aging. Clin Colorectal Cancer. 2014; 13:213–218.
Article26. Jeon CH, Lee HI, Shin IH, Park JW. Genetic alterations of APC, K-ras, p53, MSI, and MAGE in Korean colorectal cancer patients. Int J Colorectal Dis. 2008; 23:29–35.
Article27. Jeong SY, Shin KH, Shin JH, et al. Microsatellite instability and mutations in DNA mismatch repair genes in sporadic colorectal cancers. Dis Colon Rectum. 2003; 46:1069–1077.
Article28. Won YJ, Park KJ, Kwon HJ, et al. Germline mutations of the APC gene in Korean familial adenomatous polyposis patients. J Hum Genet. 1999; 44:103–108.
Article29. Hutter P, Rey-Berthod C, Chappuis PO, et al. Molecular and clinical characteristics in 32 families affected with familial adenomatous polyposis. Hum Mutat. 2001; 18:550.
Article30. Calistri D, Rengucci C, Seymour I, et al. Mutation analysis of p53, K-ras, and BRAF genes in colorectal cancer progression. J Cell Physiol. 2005; 204:484–488.
Article31. Oh HE, Cho SJ, Won NH, Lee D, Kim I, Yeom BW. K-ras gene mutations and expression of K-ras, p16, cyclin D1 and p53 in synchronous lesions of the colon adenoma-carcinoma sequences. Korean J Pathol. 2001; 35:291–298.32. Zeng C, Matsuda K, Jia WH, et al. Identification of susceptibility loci and genes for colorectal cancer risk. Gastroenterology. 2016; 150:1633–1645.33. Lu Y, Kweon SS, Tanikawa C, et al. Large-scale genome-wide association study of East Asians identifies loci associated with risk for colorectal cancer. Gastroenterology. 2019; 156:1455–1466.34. Wang N, Lu Y, Khankari NK, et al. Evaluation of genetic variants in association with colorectal cancer risk and survival in Asians. Int J Cancer. 2017; 141:1130–1139.
Article35. Abe M, Ito H, Oze I, Nomura M, Ogawa Y, Matsuo K. The more from East-Asian, the better: risk prediction of colorectal cancer risk by GWAS-identified SNPs among Japanese. J Cancer Res Clin Oncol. 2017; 143:2481–2492.
Article36. Song N, Shin A, Jung HS, Oh JH, Kim J. Effects of interactions between common genetic variants and smoking on colorectal cancer. BMC Cancer. 2017; 17:869.
Article37. Sung JJ, Lau JY, Young GP, et al. Asia Pacific consensus recommendations for colorectal cancer screening. Gut. 2008; 57:1166–1176.
Article38. Abu Hassan MR, Ismail I, Mohd Suan MA, et al. Incidence and mortality rates of colorectal cancer in Malaysia. Epidemiol Health. 2016; 38:e2016007.
Article39. Lee HP, Lee J, Shanmugaratnam K. Trends and ethnic variation in incidence and mortality from cancers of the colon and rectum in Singapore, 1968 to 1982. Ann Acad Med Singapore. 1987; 16:397–401.40. Ladabaum U, Clarke CA, Press DJ, et al. Colorectal cancer incidence in Asian populations in California: effect of nativity and neighborhood-level factors. Am J Gastroenterol. 2014; 109:579–588.
Article41. Noone AM, Howlader N, Krapcho M, et al. SEER cancer statistics review (CSR) 1975-2015. National Cancer Institute Web site. https://seer.cancer.gov/csr/1975_2015/. Updated September 10, 2018. Accessed February 11, 2019.42. Jung KW, Won YJ, Kong HJ, Lee ES; Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. 2018; 50:303–316.
Article43. Chen W, Sun K, Zheng R, et al. Cancer incidence and mortality in China, 2014. Chin J Cancer Res. 2018; 30:1–12.
Article44. Cancer Information Service; National Cancer Center Japan. National estimates of cancer incidence based on cancer registries in Japan (1975-2013). Cancer Information Service Web site. https://ganjoho.jp/en/professional/statistics/table_download.html. Accessed February 13, 2019.45. Gu X, Zheng R, Xia C, et al. Interactions between life expectancy and the incidence and mortality rates of cancer in China: a population-based cluster analysis. Cancer Commun (Lond). 2018; 38:44.
Article46. The World Bank. Life expectancy at birth, total (years). The World Bank Web site. The World Bank Web site. https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=Z4&view=map&year_high_desc=true. Accessed February 14, 2019.47. Hong Kong Cancer Registry HA. Colorectal cancer in 2016. Hospital Authority Web site. http://www3.ha.org.hk/cancereg/pdf/factsheet/2016/colorectum_2016.pdf. Accessed February 13, 2019.48. Stewart RJ, Stewart AW, Turnbull PR, Isbister WH. Sex differences in subsite incidence of large-bowel cancer. Dis Colon Rectum. 1983; 26:658–660.
Article49. Bonithon-Kopp C, Benhamiche AM. Are there several colorectal cancers? Epidemiological data. Eur J Cancer Prev. 1999; 8 Suppl 1:S3–S12.
Article50. McCashland TM, Brand R, Lyden E, de Garmo P; CORI Research Project. Gender differences in colorectal polyps and tumors. Am J Gastroenterol. 2001; 96:882–886.
Article51. Newcomb PA, Zheng Y, Chia VM, et al. Estrogen plus progestin use, microsatellite instability, and the risk of colorectal cancer in women. Cancer Res. 2007; 67:7534–7539.
Article52. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002; 288:321–333.
Article53. Nguyen SP, Bent S, Chen YH, Terdiman JP. Gender as a risk factor for advanced neoplasia and colorectal cancer: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009; 7:676–681.
Article54. Sung JJ, Lau JY, Goh KL, Leung WK; Asia Pacific Working Group on Colorectal Cancer.. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol. 2005; 6:871–876.
Article55. Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009; 22:191–197.
Article56. Ng SC, Lau JY, Chan FK, et al. Increased risk of advanced neoplasms among asymptomatic siblings of patients with colorectal cancer. Gastroenterology. 2013; 144:544–550.
Article57. Liu Y, Ding WB, Yan C, Bao H, Li K, Wang C. Risk factors of colorectal cancer and its clinical epidemiological study. Biomed Res. 2017; 28:9871–9874.58. Kotake K, Koyama Y, Nasu J, Fukutomi T, Yamaguchi N. Relation of family history of cancer and environmental factors to the risk of colorectal cancer: a case-control study. Jpn J Clin Oncol. 1995; 25:195–202.59. Shin A, Joo J, Bak J, et al. Site-specific risk factors for colorectal cancer in a Korean population. PLoS One. 2011; 6:e23196.
Article60. Wong MCS, Chan CH, Lin J, et al. Lower relative contribution of positive family history to colorectal cancer risk with increasing age: a systematic review and meta-analysis of 9.28 million individuals. Am J Gastroenterol. 2018; 113:1819–1827.
Article61. Wong MC, Ching JY, Chiu HM, et al. Risk of colorectal neoplasia in individuals with self-reported family history: a prospective colonoscopy study from 16 Asia-Pacific regions. Am J Gastroenterol. 2016; 111:1621–1629.
Article62. Song X, Gong X, Zhang T, Jiang W. Height and risk of colorectal cancer: a meta-analysis. Eur J Cancer Prev. 2018; 27:521–529.
Article63. Shimizu N, Nagata C, Shimizu H, et al. Height, weight, and alcohol consumption in relation to the risk of colorectal cancer in Japan: a prospective study. Br J Cancer. 2003; 88:1038–1043.
Article64. Sung J, Song YM, Lawlor DA, Smith GD, Ebrahim S. Height and site-specific cancer risk: a cohort study of a Korean adult population. Am J Epidemiol. 2009; 170:53–64.
Article65. Otani T, Iwasaki M, Inoue M; Shoichiro Tsugane for the Japan Public Health Center-based Prospective Study Group. Body mass index, body height, and subsequent risk of colorectal cancer in middle-aged and elderly Japanese men and women: Japan public health center-based prospective study. Cancer Causes Control. 2005; 16:839–850.
Article66. Pyo JH, Hong SN, Min BH, et al. Is height a risk factor for colorectal adenoma? Korean J Intern Med. 2016; 31:653–659.
Article67. Yeoh KG, Ho KY, Chiu HM, et al. The Asia-Pacific Colorectal Screening score: a validated tool that stratifies risk for colorectal advanced neoplasia in asymptomatic Asian subjects. Gut. 2011; 60:1236–1241.
Article68. Gu MJ, Huang QC, Bao CZ, et al. Attributable causes of colorectal cancer in China. BMC Cancer. 2018; 18:38.
Article69. Tsong WH, Koh WP, Yuan JM, Wang R, Sun CL, Yu MC. Cigarettes and alcohol in relation to colorectal cancer: the Singapore Chinese Health Study. Br J Cancer. 2007; 96:821–827.
Article70. Poomphakwaen K, Promthet S, Suwanrungruang K, Kamsaard S, Wiangnon S. Risk factors for colorectal cancer in Thailand. Asian Pac J Cancer Prev. 2015; 16:6105–6109.
Article71. Mafiana RN, Al Lawati AS, Waly MI, Al Farsi Y, Al Kindi M, Al Moundhri M. Association between dietary and lifestyle indices and colorectal cancer in Oman: a case-control study. Asian Pac J Cancer Prev. 2018; 19:3117–3122.
Article72. Naing C, Lai PK, Mak JW. Immediately modifiable risk factors attributable to colorectal cancer in Malaysia. BMC Public Health. 2017; 17:637.
Article73. Choi YJ, Lee DH, Han KD, et al. The relationship between drinking alcohol and esophageal, gastric or colorectal cancer: a nationwide population-based cohort study of South Korea. PLoS One. 2017; 12:e0185778.
Article74. Mizoue T, Inoue M, Wakai K, et al. Alcohol drinking and colorectal cancer in Japanese: a pooled analysis of results from five cohort studies. Am J Epidemiol. 2008; 167:1397–1406.
Article75. Akhter M, Kuriyama S, Nakaya N, et al. Alcohol consumption is associated with an increased risk of distal colon and rectal cancer in Japanese men: the Miyagi Cohort Study. Eur J Cancer. 2007; 43:383–390.
Article76. Wong TS, Chay WY, Tan MH, Chow KY, Lim WY. Reproductive factors, obesity and risk of colorectal cancer in a cohort of Asian women. Cancer Epidemiol. 2019; 58:33–43.
Article77. Guo L, Li N, Wang G, et al. Body mass index and cancer incidence: a prospective cohort study in northern China. Zhonghua Liu Xing Bing Xue Za Zhi. 2014; 35:231–236.78. Li H, Yang G, Xiang YB, et al. Body weight, fat distribution and colorectal cancer risk: a report from cohort studies of 134255 Chinese men and women. Int J Obes (Lond). 2013; 37:783–789.
Article79. Shin CM, Han K, Lee DH, et al. Association among obesity, metabolic health, and the risk for colorectal cancer in the general population in Korea using the national health insurance service-national sample cohort. Dis Colon Rectum. 2017; 60:1192–1200.
Article80. Matsuo K, Mizoue T, Tanaka K, et al. Association between body mass index and the colorectal cancer risk in Japan: pooled analysis of population-based cohort studies in Japan. Ann Oncol. 2012; 23:479–490.
Article81. Odegaard AO, Koh WP, Yu MC, Yuan JM. Body mass index and risk of colorectal cancer in Chinese Singaporeans: the Singapore Chinese Health Study. Cancer. 2011; 117:3841–3849.
Article82. Yee YK, Tan VP, Chan P, Hung IF, Pang R, Wong BC. Epidemiology of colorectal cancer in Asia. J Gastroenterol Hepatol. 2009; 24:1810–1816.
Article83. Azeem S, Gillani SW, Siddiqui A, Jandrajupalli SB, Poh V, Syed Sulaiman SA. Diet and colorectal cancer risk in Asia: a systematic review. Asian Pac J Cancer Prev. 2015; 16:5389–5396.84. Chiu BC, Ji BT, Dai Q, et al. Dietary factors and risk of colon cancer in Shanghai, China. Cancer Epidemiol Biomarkers Prev. 2003; 12:201–208.85. Park Y, Lee J, Oh JH, Shin A, Kim J. Dietary patterns and colorectal cancer risk in a Korean population: a case-control study. Medicine (Baltimore). 2016; 95:e3759.86. Oba S, Shimizu N, Nagata C, et al. The relationship between the consumption of meat, fat, and coffee and the risk of colon cancer: a prospective study in Japan. Cancer Lett. 2006; 244:260–267.
Article87. Wada K, Oba S, Tsuji M, et al. Meat consumption and colorectal cancer risk in Japan: the Takayama study. Cancer Sci. 2017; 108:1065–1070.
Article88. Shin A, Li H, Shu XO, Yang G, Gao YT, Zheng W. Dietary intake of calcium, fiber and other micronutrients in relation to colorectal cancer risk: results from the Shanghai Women’s Health Study. Int J Cancer. 2006; 119:2938–2942.
Article89. Sato Y, Nakaya N, Kuriyama S, Nishino Y, Tsubono Y, Tsuji I. Meat consumption and risk of colorectal cancer in Japan: the Miyagi Cohort Study. Eur J Cancer Prev. 2006; 15:211–218.
Article90. Otani T, Iwasaki M, Ishihara J, et al. Dietary fiber intake and subsequent risk of colorectal cancer: the Japan Public Health Center-based prospective study. Int J Cancer. 2006; 119:1475–1480.
Article91. Butler LM, Wang R, Koh WP, Yu MC. Prospective study of dietary patterns and colorectal cancer among Singapore Chinese. Br J Cancer. 2008; 99:1511–1516.
Article92. Kumagai Y, Chou WT, Tomata Y, et al. Dietary patterns and colorectal cancer risk in Japan: the Ohsaki Cohort Study. Cancer Causes Control. 2014; 25:727–736.
Article93. Pham NM, Mizoue T, Tanaka K, et al. Physical activity and colorectal cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol. 2012; 42:2–13.94. Chan AO, Jim MH, Lam KF, et al. Prevalence of colorectal neoplasm among patients with newly diagnosed coronary artery disease. JAMA. 2007; 298:1412–1419.
Article95. Sobhani I, Tap J, Roudot-Thoraval F, et al. Microbial dysbiosis in colorectal cancer (CRC) patients. PLoS One. 2011; 6:e16393.
Article96. Yu J, Feng Q, Wong SH, et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut. 2017; 66:70–78.
Article97. Zeller G, Tap J, Voigt AY, et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol Syst Biol. 2014; 10:766.
Article98. Nakatsu G, Zhou H, Wu WK, et al. Alterations in enteric virome are associated with colorectal cancer and survival outcomes. Gastroenterology. 2018; 155:529–541.
Article99. Kwong TN, Wang X, Nakatsu G, et al. Association between bacteremia from specific microbes and subsequent diagnosis of colorectal cancer. Gastroenterology. 2018; 155:383–390.
Article100. Zumkeller N, Brenner H, Zwahlen M, Rothenbacher D. Helicobacter pylori infection and colorectal cancer risk: a metaanalysis. Helicobacter. 2006; 11:75–80.
Article101. Guo Y, Li HY. Association between Helicobacter pylori infection and colorectal neoplasm risk: a meta-analysis based on East Asian population. J Cancer Res Ther. 2014; 10 Suppl:263–266.
Article102. Sung JJ, Ng SC, Chan FK, et al. An updated Asia Pacific consensus recommendations on colorectal cancer screening. Gut. 2015; 64:121–132.
Article103. Lee BI, Hong SP, Kim SE, et al. Korean guidelines for colorectal cancer screening and polyp detection. J Korean Soc Radiol. 2012; 66:385–406.
Article104. Tatar M, Tatar F. Colorectal cancer in Turkey: current situation and challenges for the future. Eur J Health Econ. 2010; 10 Suppl 1:S99–S105.
Article105. Ministry of Health Singapore. Screen for life. Ministry of Health Singapore Web site. https://www.healthhub.sg/programmes/61/Screen_for_Life. Accessed February 14, 2019.106. Sung JJ, Chan FK, Leung WK, et al. Screening for colorectal cancer in Chinese: comparison of fecal occult blood test, flexible sigmoidoscopy, and colonoscopy. Gastroenterology. 2003; 124:608–614.
Article107. Choe JW, Chang HS, Yang SK, et al. Screening colonoscopy in asymptomatic average-risk Koreans: analysis in relation to age and sex. J Gastroenterol Hepatol. 2007; 22:1003–1008.
Article108. Chiu HM, Wang HP, Lee YC, et al. A prospective study of the frequency and the topographical distribution of colon neoplasia in asymptomatic average-risk Chinese adults as determined by colonoscopic screening. Gastrointest Endosc. 2005; 61:547–553.
Article109. Leung WK, Ho KY, Kim WH, et al. Colorectal neoplasia in Asia: a multicenter colonoscopy survey in symptomatic patients. Gastrointest Endosc. 2006; 64:751–759.
Article110. Kim JY, Choi S, Park T, et al. Development and validation of a scoring system for advanced colorectal neoplasm in young Korean subjects less than age 50 years. Intest Res. 2019; 17:253–264.
Article111. Ma E, Sasazuki S, Iwasaki M, et al. 10-Year risk of colorectal cancer: development and validation of a prediction model in middle-aged Japanese men. Cancer Epidemiol. 2010; 34:534–541.
Article112. Meng W, Cai SR, Zhou L, Dong Q, Zheng S, Zhang SZ. Performance value of high risk factors in colorectal cancer screening in China. World J Gastroenterol. 2009; 15:6111–6116.
Article113. Cancer Expert Working Group on Cancer Prevention and Screening (CHP). Prevention and screening for colorectal cancer. CHP of Department of Health Web site. https://www.chp.gov.hk/files/pdf/colorectal_ca_en.pdf. Accessed February 14, 2019.114. Wong MC, Ching JY, Ng SC, et al. Prediction of proximal advanced neoplasia: a comparison of four existing sigmoidoscopy-based strategies in a Chinese population. Gut. 2015; 64:776–783.
Article115. Wong MC, Lam TY, Tsoi KK, et al. A validated tool to predict colorectal neoplasia and inform screening choice for asymptomatic subjects. Gut. 2014; 63:1130–1136.
Article116. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for colorectal cancer: US preventive services task force recommendation statement. JAMA. 2016; 315:2564–2575.117. Wolf AM, Fontham ET, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018; 68:250–281.
Article118. Jung KJ, Won D, Jeon C, et al. A colorectal cancer prediction model using traditional and genetic risk scores in Koreans. BMC Genet. 2015; 16:49.
Article119. Li J, Chang J, Zhu Y, et al. Risk prediction of colorectal cancer with common genetic variants and conventional non-genetic factors in a Chinese Han population. Zhonghua Liu Xing Bing Xue Za Zhi. 2015; 36:1053–1057.120. Iwasaki M, Tanaka-Mizuno S, Kuchiba A, et al. Inclusion of a genetic risk score into a validated risk prediction model for colorectal cancer in Japanese men improves performance. Cancer Prev Res (Phila). 2017; 10:535–541.
Article121. Wong MC, Ching JY, Lam TY, et al. Association of interactive reminders and automated messages with persistent adherence to colorectal cancer screening: a randomized clinical trial. JAMA Oncol. 2017; 3:1281–1283.
Article122. Wong MC, Ching JY, Huang J, et al. Effectiveness of reminder strategies on cancer screening adherence: a randomised controlled trial. Br J Gen Pract. 2018; 68:e604–e611.
Article123. Wong MC. Colorectal cancer screening in Hong Kong: investment of more resources needed to strengthen screening services and inform governmental policy. Hong Kong Med J. 2011; 17:348–349.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Screening strategy for colorectal cancer according to risk
- Strategies for colorectal cancer screening and post-polypectomy surveillance for young adults under age 50
- Inflammatory Bowel Disease-related Colorectal Cancer in the Asia-Pacific Region: Past, Present, and Future
- Prevalence and Risk Factors of Irritable Bowel Syndrome in Asia
- Obesity and Colorectal Cancer