Korean J Gastroenterol.
2023 Aug;82(2):63-72. 10.4166/kjg.2023.083.
Obesity and Colorectal Cancer
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2545330
- DOI: http://doi.org/10.4166/kjg.2023.083
Abstract
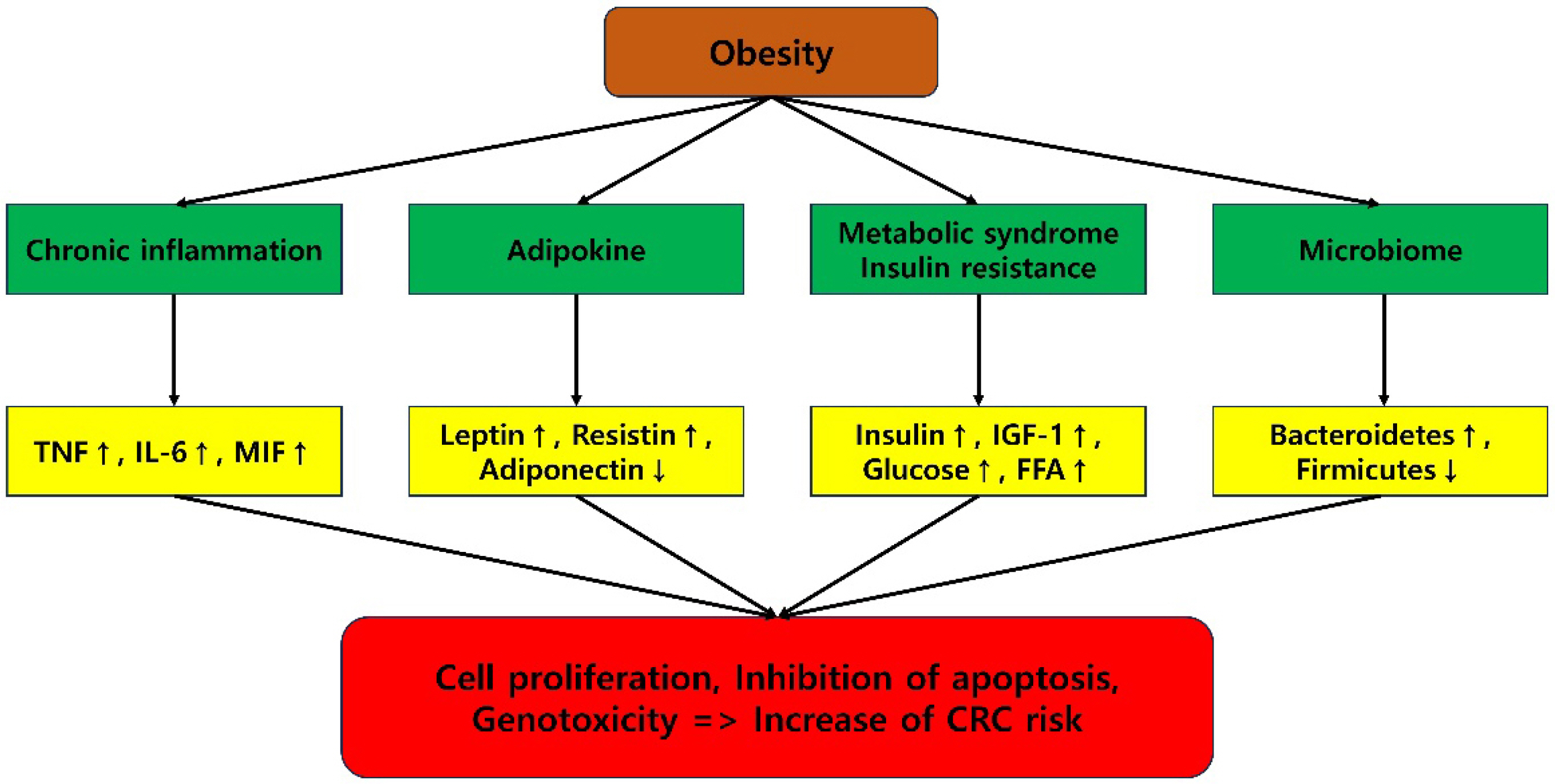
- The prevalence of obesity has increased significantly worldwide, and this trend is likely to continue in the coming years. There is substantial evidence that obesity plays a crucial role in the development of colorectal cancer. Epidemiological data have consistently demonstrated a correlation between obesity and colorectal cancer. Insulin resistance, hyperinsulinemia, chronic inflammation, altered levels of growth factors, adipocytokines, and various hormones are plausible biological mechanisms. In addition, obesity has been shown to have an impact on recurrence, treatment success, and overall survival. There are some reports, although the evidence is not conclusive, that weight loss and lifestyle changes such as dietary modification and physical activity can reduce the risk of colorectal cancer. The understanding that obesity is a potentially modifiable risk factor that can affect the incidence and prognosis of colorectal cancer is crucial knowledge that can have an impact on the prevention and treatment of the condition.
Keyword
Figure
Reference
-
1. Analysis of the status of malnutrition and obesity treatment in the last five years (2017-2021). [Internet]. The Health Insurance Review and Assessment Service;cited 2022 Apr 21. Available from: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020041000100&brdScnBltNo=4&brdBltNo=10575&pageIndex=1.2. Chang P, Friedenberg F. 2014; Obesity and GERD. Gastroenterol Clin North Am. 43:161–173. DOI: 10.1016/j.gtc.2013.11.009. PMID: 24503366. PMCID: PMC3920303.
Article3. Lee CG, Lee JK, Kang YS, et al. 2015; Visceral abdominal obesity is associated with an increased risk of irritable bowel syndrome. Am J Gastroenterol. 110:310–319. DOI: 10.1038/ajg.2014.422. PMID: 25583325.
Article4. Agarwal A, Singh A, Mehtab W, et al. 2021; Patients with celiac disease are at high risk of developing metabolic syndrome and fatty liver. Intest Res. 19:106–114. DOI: 10.5217/ir.2019.00136. PMID: 32312034. PMCID: PMC7873403.
Article5. Friedenreich CM, Ryder-Burbidge C, McNeil J. 2021; Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biologic mechanisms. Mol Oncol. 15:790–800. DOI: 10.1002/1878-0261.12772. PMID: 32741068. PMCID: PMC7931121.6. Belladelli F, Montorsi F, Martini A. 2022; Metabolic syndrome, obesity and cancer risk. Curr Opin Urol. 32:594–597. DOI: 10.1097/MOU.0000000000001041. PMID: 36081396.
Article7. Death rates by major carcinoma in 2021. [Internet]. National Cancer Information Center;cited 2022 Sep 28. Available from: https://www.cancer.go.kr/lay1/S1T645C646/contents.do.8. Data on health insurance treatment status for colorectal cancer from 2012 to 2021. [Internet]. National Health Insurance Service;cited 2022 Oct 20. Available from: https://www.nhis.or.kr/nhis/together/wbhaea01600m01.do?mode=view&articleNo=10828825&article.offset=0&articleLimit=10&srSearchVal=%EB%8C%80%EC%9E%A5%EC%95%94.9. Chen Q, Wang J, Yang J, et al. 2015; Association between adult weight gain and colorectal cancer: a dose-response meta-analysis of observational studies. Int J Cancer. 136:2880–2889. DOI: 10.1002/ijc.29331. PMID: 25395274.
Article10. Garcia H, Song M. 2019; Early-life obesity and adulthood colorectal cancer risk: a meta-analysis. Rev Panam Salud Publica. 43:e3. DOI: 10.26633/RPSP.2019.3. PMID: 31093227. PMCID: PMC6393738.
Article11. Sninsky JA, Shore BM, Lupu GV, Crockett SD. 2022; Risk factors for colorectal polyps and cancer. Gastrointest Endosc Clin N Am. 32:195–213. DOI: 10.1016/j.giec.2021.12.008. PMID: 35361331.
Article12. Øines M, Helsingen LM, Bretthauer M, Emilsson L. 2017; Epidemiology and risk factors of colorectal polyps. Best Pract Res Clin Gastroenterol. 31:419–424. DOI: 10.1016/j.bpg.2017.06.004. PMID: 28842051.
Article13. Schlesinger S, Aleksandrova K, Abar L, et al. 2017; Adult weight gain and colorectal adenomas-a systematic review and meta-analysis. Ann Oncol. 28:1217–1229. DOI: 10.1093/annonc/mdx080. PMID: 28327995.
Article14. Anderson JC, Calderwood AH, Christensen BC, Robinson CM, Amos CI, Butterly L. 2018; Smoking and other risk factors in individuals with synchronous conventional high-risk adenomas and clinically significant serrated polyps. Am J Gastroenterol. 113:1828–1835. DOI: 10.1038/s41395-018-0393-0. PMID: 30385834. PMCID: PMC6768665.
Article15. Bailie L, Loughrey MB, Coleman HG. 2017; Lifestyle risk factors for serrated colorectal polyps: A systematic review and meta-analysis. Gastroenterology. 152:92–104. DOI: 10.1053/j.gastro.2016.09.003. PMID: 27639804.
Article16. Wong MC, Chan CH, Cheung W, et al. 2018; Association between investigator-measured body-mass index and colorectal adenoma: a systematic review and meta-analysis of 168,201 subjects. Eur J Epidemiol. 33:15–26. DOI: 10.1007/s10654-017-0336-x. PMID: 29288474. PMCID: PMC5803281.17. Gathirua-Mwangi WG, Monahan P, Song Y, et al. 2017; Changes in adult BMI and waist circumference are associated with increased risk of advanced colorectal neoplasia. Dig Dis Sci. 62:3177–3185. DOI: 10.1007/s10620-017-4778-5. PMID: 28983748. PMCID: PMC5653429.
Article18. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. 2016; Body fatness and cancer--viewpoint of the IARC working group. N Engl J Med. 375:794–798. DOI: 10.1056/NEJMsr1606602. PMID: 27557308. PMCID: PMC6754861.
Article19. Ma Y, Yang Y, Wang F, et al. 2013; Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS One. 8:e53916. DOI: 10.1371/journal.pone.0053916. PMID: 23349764. PMCID: PMC3547959.
Article20. Abar L, Vieira AR, Aune D, et al. 2018; Height and body fatness and colorectal cancer risk: an update of the WCRF-AICR systematic review of published prospective studies. Eur J Nutr. 57:1701–1720. DOI: 10.1007/s00394-017-1557-1. PMID: 29080978. PMCID: PMC6060816.
Article21. Ning Y, Wang L, Giovannucci EL. 2010; A quantitative analysis of body mass index and colorectal cancer: findings from 56 observational studies. Obes Rev. 11:19–30. DOI: 10.1111/j.1467-789X.2009.00613.x. PMID: 19538439.
Article22. O'Sullivan DE, Sutherland RL, Town S, et al. 2022; Risk factors for early-onset colorectal cancer: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 20:1229–1240.e5. DOI: 10.1016/j.cgh.2021.01.037. PMID: 33524598.23. Liu PH, Wu K, Ng K, et al. 2019; Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol. 5:37–44. DOI: 10.1001/jamaoncol.2018.4280. PMID: 30326010. PMCID: PMC6382547.
Article24. Mili N, Paschou SA, Goulis DG, Dimopoulos MA, Lambrinoudaki I, Psaltopoulou T. 2021; Obesity, metabolic syndrome, and cancer: pathophysiological and therapeutic associations. Endocrine. 74:478–497. DOI: 10.1007/s12020-021-02884-x. PMID: 34625915.
Article25. Jin EH, Han K, Lee DH, et al. 2022; Association between metabolic syndrome and the risk of colorectal cancer diagnosed before age 50 years according to tumor location. Gastroenterology. 163:637–648.e2. DOI: 10.1053/j.gastro.2022.05.032. PMID: 35643169.26. Lee J, Lee KS, Kim H, et al. 2020; The relationship between metabolic syndrome and the incidence of colorectal cancer. Environ Health Prev Med. 25:6. DOI: 10.1186/s12199-020-00845-w. PMID: 32075578. PMCID: PMC7031951.27. Chen H, Zheng X, Zong X, et al. 2021; Metabolic syndrome, metabolic comorbid conditions and risk of early-onset colorectal cancer. Gut. 70:1147–1154. DOI: 10.1136/gutjnl-2020-321661. PMID: 33037055. PMCID: PMC8032822.28. Xu P, Li J, Liu J, Wang J, Wu Z, Zhang X, Zhai Y. 2017; Mature adipocytes observed to undergo reproliferation and polyploidy. FEBS Open Bio. 7:652–658. DOI: 10.1002/2211-5463.12207. PMID: 28469978. PMCID: PMC5407891.29. Cirillo F, Catellani C, Sartori C, Lazzeroni P, Amarri S, Street ME. 2019; Obesity, insulin resistance, and colorectal cancer: could miRNA dysregulation play A role? Int J Mol Sci. 20:2922. DOI: 10.3390/ijms20122922. PMID: 31207998. PMCID: PMC6628223.
Article30. Kobayashi H, Gieniec KA, Lannagan TRM, et al. 2022; The origin and contribution of cancer-associated fibroblasts in colorectal carcinogenesis. Gastroenterology. 162:890–906. DOI: 10.1053/j.gastro.2021.11.037. PMID: 34883119. PMCID: PMC8881386.
Article31. Li C, Quan J, Wei R, et al. 2020; Leptin overexpression as a poor prognostic factor for colorectal cancer. Biomed Res Int. 2020:7532514. DOI: 10.1155/2020/7532514. PMID: 32596369. PMCID: PMC7292990.
Article32. Chen YC, Chien CY, Hsu CC, et al. 2021; Obesity-associated leptin promotes chemoresistance in colorectal cancer through YAP-dependent AXL upregulation. Am J Cancer Res. 11:4220–4240.33. Lee H, Lee IS, Choue R. 2013; Obesity, inflammation and diet. Pediatr Gastroenterol Hepatol Nutr. 16:143–152. DOI: 10.5223/pghn.2013.16.3.143. PMID: 24224147. PMCID: PMC3819692.
Article34. Rasic I, Rebic V, Rasic A, Aksamija G, Radovic S. 2018; The association of simultaneous increase in interleukin-6, C reactive protein, and matrix metalloproteinase-9 serum levels with increasing stages of colorectal cancer. J Oncol. 2018:2830503. DOI: 10.1155/2018/2830503. PMID: 30154846. PMCID: PMC6091449.
Article35. Chávez-Talavera O, Tailleux A, Lefebvre P, Staels B. 2017; Bile acid control of metabolism and inflammation in obesity, type 2 diabetes, dyslipidemia, and nonalcoholic fatty liver disease. Gastroenterology. 152:1679–1694.e3. DOI: 10.1053/j.gastro.2017.01.055. PMID: 28214524.
Article36. La Frano MR, Hernandez-Carretero A, Weber N, et al. 2017; Diet-induced obesity and weight loss alter bile acid concentrations and bile acid-sensitive gene expression in insulin target tissues of C57BL/6J mice. Nutr Res. 46:11–21. DOI: 10.1016/j.nutres.2017.07.006. PMID: 29173647.
Article37. Lin H, An Y, Tang H, Wang Y. 2019; Alterations of bile acids and gut microbiota in obesity induced by high fat diet in rat model. J Agric Food Chem. 67:3624–3632. DOI: 10.1021/acs.jafc.9b00249. PMID: 30832480.
Article38. Centuori SM, Gomes CJ, Trujillo J, et al. 2016; Deoxycholic acid mediates non-canonical EGFR-MAPK activation through the induction of calcium signaling in colon cancer cells. Biochim Biophys Acta. 1861:663–670. DOI: 10.1016/j.bbalip.2016.04.006. PMID: 27086143. PMCID: PMC4900466.
Article39. Ochsenkühn T, Bayerdörffer E, Meining A, et al. 1999; Colonic mucosal proliferation is related to serum deoxycholic acid levels. Cancer. 85:1664–1669. DOI: 10.1002/(SICI)1097-0142(19990415)85:8<1664::AID-CNCR4>3.0.CO;2-O.
Article40. Nguyen TT, Ung TT, Kim NH, Jung YD. 2018; Role of bile acids in colon carcinogenesis. World J Clin Cases. 6:577–588. DOI: 10.12998/wjcc.v6.i13.577. PMID: 30430113. PMCID: PMC6232560.
Article41. Kim DS, Scherer PE. 2021; Obesity, diabetes, and increased cancer progression. Diabetes Metab J. 45:799–812. DOI: 10.4093/dmj.2021.0077. PMID: 34847640. PMCID: PMC8640143.
Article42. Renehan AG, Frystyk J, Flyvbjerg A. 2006; Obesity and cancer risk: the role of the insulin-IGF axis. Trends Endocrinol Metab. 17:328–336. DOI: 10.1016/j.tem.2006.08.006. PMID: 16956771.
Article43. Chen J, Katsifis A, Hu C, Huang XF. 2011; Insulin decreases therapeutic efficacy in colon cancer cell line HT29 via the activation of the PI3K/Akt pathway. Curr Drug Discov Technol. 8:119–125. DOI: 10.2174/157016311795563820. PMID: 21513489.
Article44. Stefani C, Miricescu D, Stanescu-Spinu II, et al. 2021; Growth factors, PI3K/AKT/mTOR and MAPK signaling pathways in colorectal cancer pathogenesis: Where are we now? Int J Mol Sci. 22:10260. DOI: 10.3390/ijms221910260. PMID: 34638601. PMCID: PMC8508474.
Article45. Kasprzak A. 2021; Insulin-like growth factor 1 (IGF-1) signaling in glucose metabolism in colorectal cancer. Int J Mol Sci. 22:6434. DOI: 10.3390/ijms22126434. PMID: 34208601. PMCID: PMC8234711.
Article46. Narayanankutty A. 2019; PI3K/Akt/mTOR pathway as a therapeutic target for colorectal cancer: A review of preclinical and clinical evidence. Curr Drug Targets. 20:1217–1226. DOI: 10.2174/1389450120666190618123846. PMID: 31215384.
Article47. Wang L, Li S, Luo H, Lu Q, Yu S. 2022; PCSK9 promotes the progression and metastasis of colon cancer cells through regulation of EMT and PI3K/AKT signaling in tumor cells and phenotypic polarization of macrophages. J Exp Clin Cancer Res. 41:303. DOI: 10.1186/s13046-022-02477-0. PMID: 36242053. PMCID: PMC9563506.
Article48. Zhao Y, Scott A, Zhang P, et al. 2017; Regulation of paxillin-p130-PI3K-AKT signaling axis by Src and PTPRT impacts colon tumorigenesis. Oncotarget. 8:48782–48793. DOI: 10.18632/oncotarget.10654. PMID: 27447856. PMCID: PMC5564724.
Article49. Chen J, Elfiky A, Han M, Chen C, Saif MW. 2014; The role of Src in colon cancer and its therapeutic implications. Clin Colorectal Cancer. 13:5–13. DOI: 10.1016/j.clcc.2013.10.003. PMID: 24361441.
Article50. Zhu S, Bjorge JD, Fujita DJ. 2007; PTP1B contributes to the oncogenic properties of colon cancer cells through Src activation. Cancer Res. 67:10129–10137. DOI: 10.1158/0008-5472.CAN-06-4338. PMID: 17974954.
Article51. Sekharam M, Nasir A, Kaiser HE, Coppola D. 2003; Insulin-like growth factor 1 receptor activates c-SRC and modifies transformation and motility of colon cancer in vitro. Anticancer Res. 23:1517–1524.52. Engin A. 2017; Diet-Induced obesity and the mechanism of leptin resistance. Adv Exp Med Biol. 960:381–397. DOI: 10.1007/978-3-319-48382-5_16. PMID: 28585208.
Article53. Aleksandrova K, Schlesinger S, Fedirko V, et al. 2017; Metabolic mediators of the association between adult weight gain and colorectal cancer: Data from the european prospective investigation into cancer and nutrition (EPIC) cohort. Am J Epidemiol. 185:751–764. DOI: 10.1093/aje/kww194. PMID: 28387787. PMCID: PMC5860400.
Article54. Endo H, Hosono K, Uchiyama T, et al. 2011; Leptin acts as a growth factor for colorectal tumours at stages subsequent to tumour initiation in murine colon carcinogenesis. Gut. 60:1363–1371. DOI: 10.1136/gut.2010.235754. PMID: 21406387.
Article55. Nigro E, Scudiero O, Monaco ML, et al. 2014; New insight into adiponectin role in obesity and obesity-related diseases. Biomed Res Int. 2014:658913. DOI: 10.1155/2014/658913. PMID: 25110685. PMCID: PMC4109424.
Article56. Duraiyarasan S, Adefuye M, Manjunatha N, Ganduri V, Rajasekaran K. 2022; Colon cancer and obesity: A narrative review. Cureus. 14:e27589. DOI: 10.7759/cureus.27589.
Article57. Sugiyama M, Takahashi H, Hosono K, et al. 2009; Adiponectin inhibits colorectal cancer cell growth through the AMPK/mTOR pathway. Int J Oncol. 34:339–344.
Article58. Fujisawa T, Endo H, Tomimoto A, et al. 2008; Adiponectin suppresses colorectal carcinogenesis under the high-fat diet condition. Gut. 57:1531–1538. DOI: 10.1136/gut.2008.159293. PMID: 18676419. PMCID: PMC2582344.
Article59. Wei EK, Giovannucci E, Fuchs CS, Willett WC, Mantzoros CS. 2005; Low plasma adiponectin levels and risk of colorectal cancer in men: a prospective study. J Natl Cancer Inst. 97:1688–1694. DOI: 10.1093/jnci/dji376. PMID: 16288122.
Article60. Moon HS, Liu X, Nagel JM, et al. 2013; Salutary effects of adiponectin on colon cancer: in vivo and in vitro studies in mice. Gut. 62:561–570. DOI: 10.1136/gutjnl-2012-302092. PMID: 22735569.
Article61. Ellulu MS, Patimah I, Khaza'ai H, Rahmat A, Abed Y. 2017; Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 13:851–863. DOI: 10.5114/aoms.2016.58928. PMID: 28721154. PMCID: PMC5507106.
Article62. Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S. 2007; Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes. 56:1010–1013. DOI: 10.2337/db06-1656. PMID: 17287468.
Article63. Nagasaki T, Hara M, Nakanishi H, Takahashi H, Sato M, Takeyama H. 2014; Interleukin-6 released by colon cancer-associated fibroblasts is critical for tumour angiogenesis: anti-interleukin-6 receptor antibody suppressed angiogenesis and inhibited tumour-stroma interaction. Br J Cancer. 110:469–478. DOI: 10.1038/bjc.2013.748. PMID: 24346288. PMCID: PMC3899773.
Article64. Rodrigues KF, Pietrani NT, Bosco AA, Campos FMF, Sandrim VC, Gomes KB. 2017; IL-6, TNF-α, and IL-10 levels/polymorphisms and their association with type 2 diabetes mellitus and obesity in Brazilian individuals. Arch Endocrinol Metab. 61:438–446. DOI: 10.1590/2359-3997000000254. PMID: 28225860.
Article65. Wei X, Li X, Kong F, et al. 2018; [TNF-α activates Wnt signaling pathway to promote the invasion of human colon cancer stem cells]. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 34:982–988. Chinese.66. Kern L, Mittenbühler MJ, Vesting AJ, et al. 2018; Obesity-induced TNFα and IL-6 signaling: The missing link between obesity and inflammation-driven liver and colorectal cancers. Cancers (Basel). 11:24. DOI: 10.3390/cancers11010024. PMID: 30591653. PMCID: PMC6356226.
Article67. Kaltschmidt C, Banz-Jansen C, Benhidjeb T, et al. 2019; A role for NF-κB in organ specific cancer and cancer stem cells. Cancers (Basel). 11:655. DOI: 10.3390/cancers11050655. PMID: 31083587. PMCID: PMC6563002.
Article68. Pikarsky E, Porat RM, Stein I, et al. 2004; NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature. 431:461–466. DOI: 10.1038/nature02924. PMID: 15329734.
Article69. Kwaifa IK, Bahari H, Yong YK, Noor SM. 2020; Endothelial dysfunction in obesity-induced inflammation: Molecular mechanisms and clinical implications. Biomolecules. 10:291. DOI: 10.3390/biom10020291. PMID: 32069832. PMCID: PMC7072669.
Article70. Yoshimura T. 2018; The chemokine MCP-1 (CCL2) in the host interaction with cancer: a foe or ally? Cell Mol Immunol. 15:335–345. DOI: 10.1038/cmi.2017.135. PMID: 29375123. PMCID: PMC6052833.
Article71. Molnár I. 2020; Interactions among thyroid hormone (FT4), chemokine (MCP-1) and neurotrophin (NGF-β) levels studied in Hungarian postmenopausal and obese women. Cytokine. 127:154948. DOI: 10.1016/j.cyto.2019.154948. PMID: 31901598.
Article72. Wang H, Tian T, Zhang J. 2021; Tumor-associated macrophages (TAMs) in colorectal cancer (CRC): From mechanism to therapy and prognosis. Int J Mol Sci. 22:8470. DOI: 10.3390/ijms22168470. PMID: 34445193. PMCID: PMC8395168.
Article73. McClellan JL, Davis JM, Steiner JL, et al. 2012; Linking tumor-associated macrophages, inflammation, and intestinal tumorigenesis: role of MCP-1. Am J Physiol Gastrointest Liver Physiol. 303:G1087–G1095. DOI: 10.1152/ajpgi.00252.2012. PMID: 23019193. PMCID: PMC3517651.
Article74. Nieman KM, Kenny HA, Penicka CV, et al. 2011; Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat Med. 17:1498–1503. DOI: 10.1038/nm.2492. PMID: 22037646. PMCID: PMC4157349.
Article75. Martin-Padura I, Gregato G, Marighetti P, et al. 2012; The white adipose tissue used in lipotransfer procedures is a rich reservoir of CD34+ progenitors able to promote cancer progression. Cancer Res. 72:325–334. DOI: 10.1158/0008-5472.CAN-11-1739. PMID: 22052460.
Article76. Mukherjee A, Bilecz AJ, Lengyel E. 2022; The adipocyte microenvironment and cancer. Cancer Metastasis Rev. 41:575–587. DOI: 10.1007/s10555-022-10059-x. PMID: 35941408.
Article77. Xiao L, Wang J, Li J, et al. 2015; RORα inhibits adipocyte-conditioned medium-induced colorectal cancer cell proliferation and migration and chick embryo chorioallantoic membrane angiopoiesis. Am J Physiol Cell Physiol. 308:C385–C396. DOI: 10.1152/ajpcell.00091.2014. PMID: 25500738.
Article78. Amemori S, Ootani A, Aoki S, et al. 2007; Adipocytes and preadipocytes promote the proliferation of colon cancer cells in vitro. Am J Physiol Gastrointest Liver Physiol. 292:G923–G929. DOI: 10.1152/ajpgi.00145.2006. PMID: 17170030.
Article79. Martinez-Outschoorn UE, Sotgia F, Lisanti MP. 2012; Power surge: supporting cells "fuel" cancer cell mitochondria. Cell Metab. 15:4–5. DOI: 10.1016/j.cmet.2011.12.011. PMID: 22225869.
Article80. Murphy N, Moreno V, Hughes DJ, et al. 2019; Lifestyle and dietary environmental factors in colorectal cancer susceptibility. Mol Aspects Med. 69:2–9. DOI: 10.1016/j.mam.2019.06.005. PMID: 31233770.
Article81. Vergara-Castañeda HA, Guevara-González RG, Ramos-Gómez M, et al. 2010; Non-digestible fraction of cooked bean (Phaseolus vulgaris L.) cultivar Bayo Madero suppresses colonic aberrant crypt foci in azoxymethane-induced rats. Food Funct. 1:294–300. DOI: 10.1039/c0fo00130a. PMID: 21776479.
Article82. Reddy BS, Hirose Y, Cohen LA, Simi B, Cooma I, Rao CV. 2000; Preventive potential of wheat bran fractions against experimental colon carcinogenesis: implications for human colon cancer prevention. Cancer Res. 60:4792–4797.83. Aune D, Chan DS, Lau R, et al. 2011; Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ. 343:d6617. DOI: 10.1136/bmj.d6617. PMID: 22074852. PMCID: PMC3213242.
Article84. Ben Q, Sun Y, Chai R, Qian A, Xu B, Yuan Y. 2014; Dietary fiber intake reduces risk for colorectal adenoma: a meta-analysis. Gastroenterology. 146:689–699.e6. DOI: 10.1053/j.gastro.2013.11.003. PMID: 24216326.
Article85. Zhang S, Jia Z, Yan Z, Yang J. 2017; Consumption of fruits and vegetables and risk of renal cell carcinoma: a meta-analysis of observational studies. Oncotarget. 8:27892–27903. DOI: 10.18632/oncotarget.15841. PMID: 28427188. PMCID: PMC5438616.
Article86. Aune D, Lau R, Chan DS, et al. 2011; Nonlinear reduction in risk for colorectal cancer by fruit and vegetable intake based on meta-analysis of prospective studies. Gastroenterology. 141:106–118. DOI: 10.1053/j.gastro.2011.04.013. PMID: 21600207.
Article87. Asghar M, George L, Lokhandwala MF. 2007; Exercise decreases oxidative stress and inflammation and restores renal dopamine D1 receptor function in old rats. Am J Physiol Renal Physiol. 293:F914–F919. DOI: 10.1152/ajprenal.00272.2007. PMID: 17634393.
Article88. Cirillo D, Rachiglio AM, la Montagna R, Giordano A, Normanno N. 2008; Leptin signaling in breast cancer: an overview. J Cell Biochem. 105:956–964. DOI: 10.1002/jcb.21911. PMID: 18821585.
Article89. Ju J, Nolan B, Cheh M, et al. 2008; Voluntary exercise inhibits intestinal tumorigenesis in Apc(Min/+) mice and azoxymethane/dextran sulfate sodium-treated mice. BMC Cancer. 8:316. DOI: 10.1186/1471-2407-8-316. PMID: 18976499. PMCID: PMC2635383.90. Rezende LFM, Sá TH, Markozannes G, et al. 2018; Physical activity and cancer: an umbrella review of the literature including 22 major anatomical sites and 770000 cancer cases. Br J Sports Med. 52:826–833. DOI: 10.1136/bjsports-2017-098391. PMID: 29146752.
Article91. Moore SC, Lee IM, Weiderpass E, et al. 2016; Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 176:816–825. DOI: 10.1001/jamainternmed.2016.1548. PMID: 27183032. PMCID: PMC5812009.
Article92. Matthews CE, Moore SC, Arem H, et al. 2020; Amount and intensity of leisure-time physical activity and lower cancer risk. J Clin Oncol. 38:686–697. DOI: 10.1200/JCO.19.02407. PMID: 31877085. PMCID: PMC7048166.
Article93. Wolin KY, Yan Y, Colditz GA. 2011; Physical activity and risk of colon adenoma: a meta-analysis. Br J Cancer. 104:882–885. DOI: 10.1038/sj.bjc.6606045. PMID: 21304525. PMCID: PMC3048199.
Article94. Zhou Y, Wu L, Li X, Wu X, Li B. 2012; Outcome of laparoscopic colorectal surgery in obese and nonobese patients: a meta-analysis. Surg Endosc. 26:783–789. DOI: 10.1007/s00464-011-1952-2. PMID: 22011944.
Article95. Makino T, Shukla PJ, Rubino F, Milsom JW. 2012; The impact of obesity on perioperative outcomes after laparoscopic colorectal resection. Ann Surg. 255:228–236. DOI: 10.1097/SLA.0b013e31823dcbf7. PMID: 22190113.
Article96. Qiu Y, Liu Q, Chen G, et al. 2016; Outcome of rectal cancer surgery in obese and nonobese patients: a meta-analysis. World J Surg Oncol. 14:23. DOI: 10.1186/s12957-016-0775-y. PMID: 26810563. PMCID: PMC4727287.
Article97. Almasaudi AS, McSorley ST, Edwards CA, McMillan DC. 2018; The relationship between body mass index and short term postoperative outcomes in patients undergoing potentially curative surgery for colorectal cancer: A systematic review and meta-analysis. Crit Rev Oncol Hematol. 121:68–73. DOI: 10.1016/j.critrevonc.2017.12.004. PMID: 29279101.
Article98. Fung A, Trabulsi N, Morris M, et al. 2017; Laparoscopic colorectal cancer resections in the obese: a systematic review. Surg Endosc. 31:2072–2088. DOI: 10.1007/s00464-016-5209-y. PMID: 27778169.
Article99. Himbert C, Ose J, Nattenmüller J, et al. 2019; Body fatness, adipose tissue compartments, and biomarkers of inflammation and angiogenesis in colorectal cancer: The ColoCare study. Cancer Epidemiol Biomarkers Prev. 28:76–82. DOI: 10.1158/1055-9965.EPI-18-0654. PMID: 30333223. PMCID: PMC6324954.
Article100. Guiu B, Petit JM, Bonnetain F, et al. 2010; Visceral fat area is an independent predictive biomarker of outcome after first-line bevacizumab-based treatment in metastatic colorectal cancer. Gut. 59:341–347. DOI: 10.1136/gut.2009.188946. PMID: 19837679.
Article101. Artaç M, Korkmaz L, Coşkun HŞ, et al. 2019; Bevacuzimab may be less effective in obese metastatic colorectal cancer patients. J Gastrointest Cancer. 50:214–220. DOI: 10.1007/s12029-017-0047-2. PMID: 29302856.
Article102. Miyamoto Y, Oki E, Emi Y, et al. 2018; Low visceral fat content is a negative predictive marker for bevacizumab in metastatic colorectal cancer. Anticancer Res. 38:491–499. DOI: 10.21873/anticanres.12249.103. Cybulska-Stopa B, Ługowska I, Wiśniowski R, et al. 2020; Overweight is associated with better prognosis in metastatic colorectal cancer patients treated with bevacizumab plus FOLFOX chemotherapy. Contemp Oncol (Pozn). 24:34–41. DOI: 10.5114/wo.2020.94728. PMID: 32514236. PMCID: PMC7265962.104. Bardou M, Barkun AN, Martel M. 2013; Obesity and colorectal cancer. Gut. 62:933–947. DOI: 10.1136/gutjnl-2013-304701. PMID: 23481261.105. Lee J, Meyerhardt JA, Giovannucci E, Jeon JY. 2015; Association between body mass index and prognosis of colorectal cancer: a meta-analysis of prospective cohort studies. PLoS One. 10:e0120706. DOI: 10.1371/journal.pone.0120706. PMID: 25811460. PMCID: PMC4374868.106. Jaspan V, Lin K, Popov V. 2021; The impact of anthropometric parameters on colorectal cancer prognosis: A systematic review and meta-analysis. Crit Rev Oncol Hematol. 159:103232. DOI: 10.1016/j.critrevonc.2021.103232. PMID: 33497759.107. Griggs JJ, Bohlke K, Balaban EP, et al. 2021; Appropriate systemic therapy dosing for obese adult patients with cancer: ASCO guideline update. J Clin Oncol. 39:2037–2048. DOI: 10.1200/JCO.21.00471. PMID: 33939491.
Article108. Hourdequin KC, Schpero WL, McKenna DR, Piazik BL, Larson RJ. 2013; Toxic effect of chemotherapy dosing using actual body weight in obese versus normal-weight patients: a systematic review and meta-analysis. Ann Oncol. 24:2952–2962. DOI: 10.1093/annonc/mdt294. PMID: 23965736.
Article109. Stocker G, Hacker UT, Fiteni F, et al. 2018; Clinical consequences of chemotherapy dose reduction in obese patients with stage III colon cancer: A retrospective analysis from the PETACC 3 study. Eur J Cancer. 99:49–57. DOI: 10.1016/j.ejca.2018.05.004. PMID: 29906734.
Article110. Christakoudi S, Pagoni P, Ferrari P, et al. 2021; Weight change in middle adulthood and risk of cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Int J Cancer. 148:1637–1651. DOI: 10.1002/ijc.33339. PMID: 33038275.
Article111. Luo J, Hendryx M, Manson JE, et al. 2019; Intentional weight loss and obesity-related cancer risk. JNCI Cancer Spectr. 3:pkz054. DOI: 10.1093/jncics/pkz054. PMID: 31737862. PMCID: PMC6795232.
Article112. Khalid SI, Maasarani S, Wiegmann J, et al. 2022; Association of bariatric surgery and risk of cancer in patients with morbid obesity. Ann Surg. 275:1–6. DOI: 10.1097/SLA.0000000000005035. PMID: 34183506.
Article113. Taube M, Peltonen M, Sjöholm K, et al. 2021; Long-term incidence of colorectal cancer after bariatric surgery or usual care in the Swedish Obese Subjects study. PLoS One. 16:e0248550. DOI: 10.1371/journal.pone.0248550. PMID: 33764991. PMCID: PMC7993847.
Article114. Mackenzie H, Markar SR, Askari A, et al. 2018; Obesity surgery and risk of cancer. Br J Surg. 105:1650–1657. DOI: 10.1002/bjs.10914. PMID: 30003539.
Article115. Murphy R, Tsai P, Jüllig M, Liu A, Plank L, Booth M. 2017; Differential changes in gut microbiota after gastric bypass and sleeve gastrectomy bariatric surgery vary according to diabetes remission. Obes Surg. 27:917–925. DOI: 10.1007/s11695-016-2399-2. PMID: 27738970.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Colorectal Cancer and Obesity
- Obesity and Colorectal Cancer
- A Case-Control Study on the Relationship between Obesity and Female Colorectal Cancer
- Long-term Oncologic Outcomes of Obesity after Laparoscopic Surgery for Colorectal Cancer in Asian Patients
- Obesity-Related Colorectal Cancer: The Role of Leptin