J Neurocrit Care.
2019 Jun;12(1):30-36. 10.18700/jnc.190076.
Primary neurocritical care involving therapeutic hypothermia for acute ischemic stroke patients with malignant infarct cores
- Affiliations
-
- 1Department of Neurology, Ajou University School of Medicine, Suwon, Republic of Korea. dacda@hanmail.net
- KMID: 2452824
- DOI: http://doi.org/10.18700/jnc.190076
Abstract
- BACKGROUND
Acute ischemic stroke patients with malignant infarct cores were primarily treated with neurocritical care based on reperfusion and hypothermia. We evaluated the predictors for malignant progression and functional outcomes.
METHODS
From January 2010 to March 2015 ischemic stroke patients with large vessel occlusion of the anterior circulation with infarct volume >82 mL on baseline diffusion weighted image (DWI) within 6 hours from onset, with National Institutes of Health Stroke Scale ≥15 were included. All patients were managed with intent for reperfusion and neurocritical care. Malignant progression was defined as clinical signs of progressive herniation. Predictive factors for malignant progression and outcomes of decompressive hemicraniectomy (DHC) were evaluated.
RESULTS
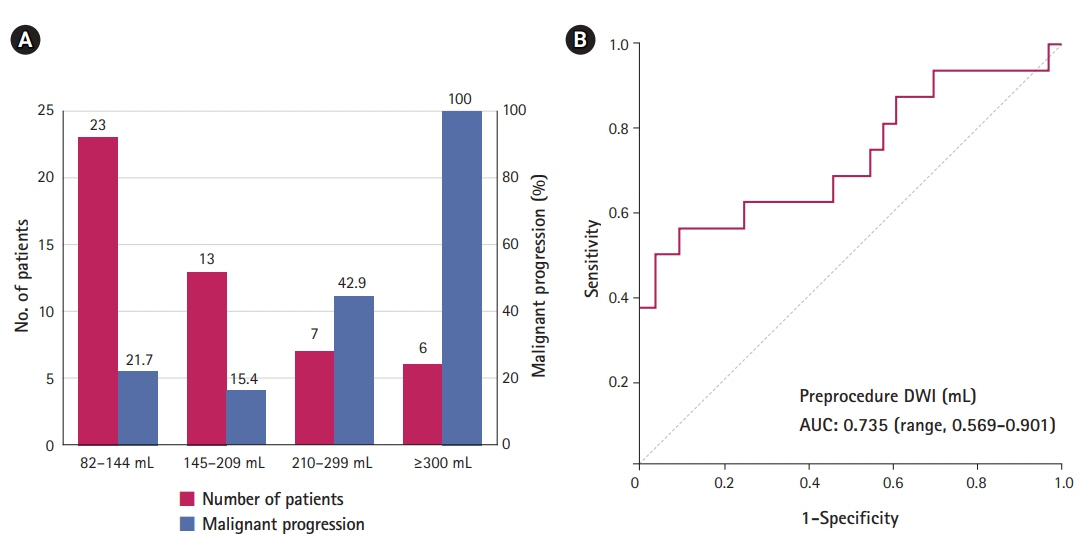
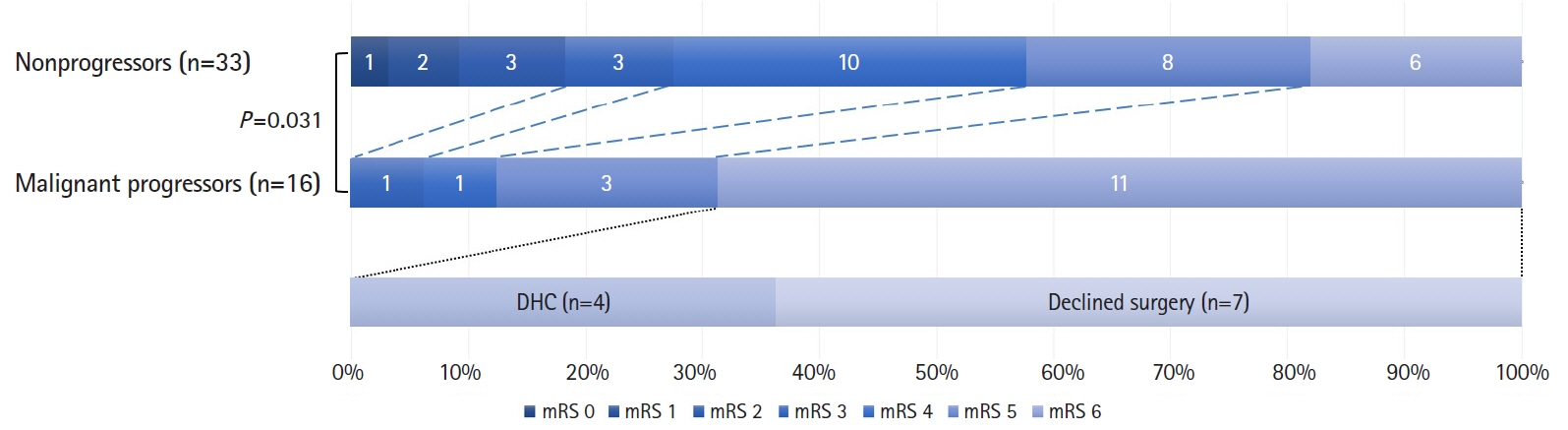
In total, 49 patients were included in the study. Among them, 33 (67.3%) could be managed with neurocritical care and malignant progression was observed in the remainder. Decompressive surgery was performed in nine patients (18.4%). Factors predictive of malignant progression were initial DWI volumes (odds ratio [OR], 1.01; 95% confidence interval [CI], 1.00 to 1.02; P=0.046) and parenchymal hematoma (OR, 6.77; 95% CI, 1.50 to 30.53; P=0.013) on computed tomography taken at Day 1. Infarct volume of >210 mL predicted malignant progression with 56.3% sensitivity and 90.9% specificity. Among the malignant progressors, 77.7% resulted in grave outcomes even with DHC, while all patients who declined surgery died.
CONCLUSION
Acute ischemic stroke patients with malignant cores between 82 to 209 mL can be primarily treated with neurocritical care based on reperfusion and hypothermia with feasible results. In patients undergoing surgical decompression due to malignant progression, the functional outcomes were not satisfactory.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Targeted temperature management for ischemic stroke
Ji Man Hong
J Neurocrit Care. 2019;12(2):67-73. doi: 10.18700/jnc.190100.
Reference
-
1. Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007; 6:215–22.
Article2. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–29.
Article3. Lee JS, Demchuk AM. Choosing a hyperacute stroke imaging protocol for proper patient selection and time efficient endovascular treatment: lessons from recent trials. J Stroke. 2015; 17:221–8.
Article4. Hong JM, Lee JS, Song HJ, Jeong HS, Choi HA, Lee K. Therapeutic hypothermia after recanalization in patients with acute ischemic stroke. Stroke. 2014; 45:134–40.
Article5. Kollmar R, Schwab S. Therapeutic hypothermia in neurological critical care. Dtsch Med Wochenschr. 2010; 135:2361–5.6. Hwang YH, Jeon JS, Kim YW, Kang DH, Kim YS, Liebeskind DS. Impact of immediate post-reperfusion cooling on outcome in patients with acute stroke and substantial ischemic changes. J Neurointerv Surg. 2017; 9:21–5.
Article7. Fuhrer H, Schönenberger S, Niesen WD, Seide S, Meyne J, Gerner ST, et al. Endovascular stroke treatment's impact on malignant type of edema (ESTIMATE). J Neurol. 2019; 266:223–31.
Article8. Vahedi K, Vicaut E, Mateo J, Kurtz A, Orabi M, Guichard JP, et al. Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke. 2007; 38:2506–17.
Article9. Hofmeijer J, Kappelle LJ, Algra A, Amelink GJ, van Gijn J, van der Worp HB, et al. Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol. 2009; 8:326–33.
Article10. Thomalla G, Hartmann F, Juettler E, Singer OC, Lehnhardt FG, Köhrmann M, et al. Prediction of malignant middle cerebral artery infarction by magnetic resonance imaging within 6 hours of symptom onset: a prospective multicenter observational study. Ann Neurol. 2010; 68:435–45.
Article11. Krieger DW, Demchuk AM, Kasner SE, Jauss M, Hantson L. Early clinical and radiological predictors of fatal brain swelling in ischemic stroke. Stroke. 1999; 30:287–92.
Article12. Jeon SB, Koh Y, Choi HA, Lee K. Critical care for patients with massive ischemic stroke. J Stroke. 2014; 16:146–60.
Article13. Mayer SA, Coplin WM, Raps EC. Cerebral edema, intracranial pressure, and herniation syndromes. J Stroke Cerebrovasc Dis. 1999; 8:183–91.
Article14. Hofmeijer J, Algra A, Kappelle LJ, van der Worp HB. Predictors of life-threatening brain edema in middle cerebral artery infarction. Cerebrovasc Dis. 2008; 25:176–84.
Article15. Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, et al. Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke. 1999; 30:2280–4.16. Albers GW. Late window paradox. Stroke. 2018; 49:768–71.
Article17. Hwang YH, Kang DH, Kim YW, Kim YS, Park SP, Liebeskind DS. Impact of time-to-reperfusion on outcome in patients with poor collaterals. AJNR Am J Neuroradiol. 2015; 36:495–500.
Article18. Lee SU, Hong JM, Kim SY, Bang OY, Demchuk AM, Lee JS. Differentiating carotid terminus occlusions into two distinct populations based on Willisian collateral status. J Stroke. 2016; 18:179–86.
Article19. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–35.
Article20. Noorian AR, Rangaraju S, Sun CH, Owada K, Nahab F, Belagaje SR, et al. Endovascular therapy in strokes with ASPECTS 5-7 may result in smaller infarcts and better outcomes as compared to medical treatment alone. Interv Neurol. 2015; 4:30–7.
Article21. Boers AMM, Jansen IGH, Beenen LFM, Devlin TG, San Roman L, Heo JH, et al. Association of follow-up infarct volume with functional outcome in acute ischemic stroke: a pooled analysis of seven randomized trials. J Neurointerv Surg. 2018; 10:1137–42.
Article22. Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. 'Malignant' middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996; 53:309–15.23. Lee JS, Lee SJ, Hong JM, Choi JW, Hong JH, Chang HW, et al. Temporal changes in care processes and outcomes for endovascular treatment of acute ischemic stroke: retrospective registry data from three Korean centers. Neurointervention. 2018; 13:2–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Targeted temperature management for ischemic stroke
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- Early In-hospital Management of Acute Ischemic Stroke
- Malignant cerebral infarction after COVID-19 myocarditis in 22-year-old female: a case report
- Applications of diffusion-weighted imaging in diagnosis, evaluation, and treatment of acute ischemic stroke