J Neurocrit Care.
2019 Dec;12(2):67-73. 10.18700/jnc.190100.
Targeted temperature management for ischemic stroke
- Affiliations
-
- 1Department of Neurology, Ajou University School of Medicine, Suwon, Republic of Korea. dacda@hanmail.net
- KMID: 2470467
- DOI: http://doi.org/10.18700/jnc.190100
Abstract
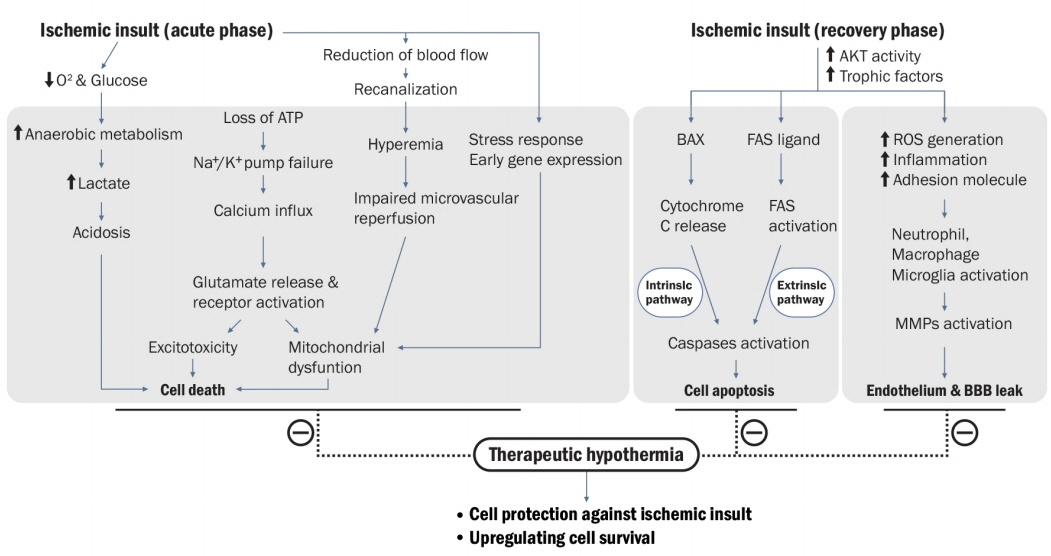
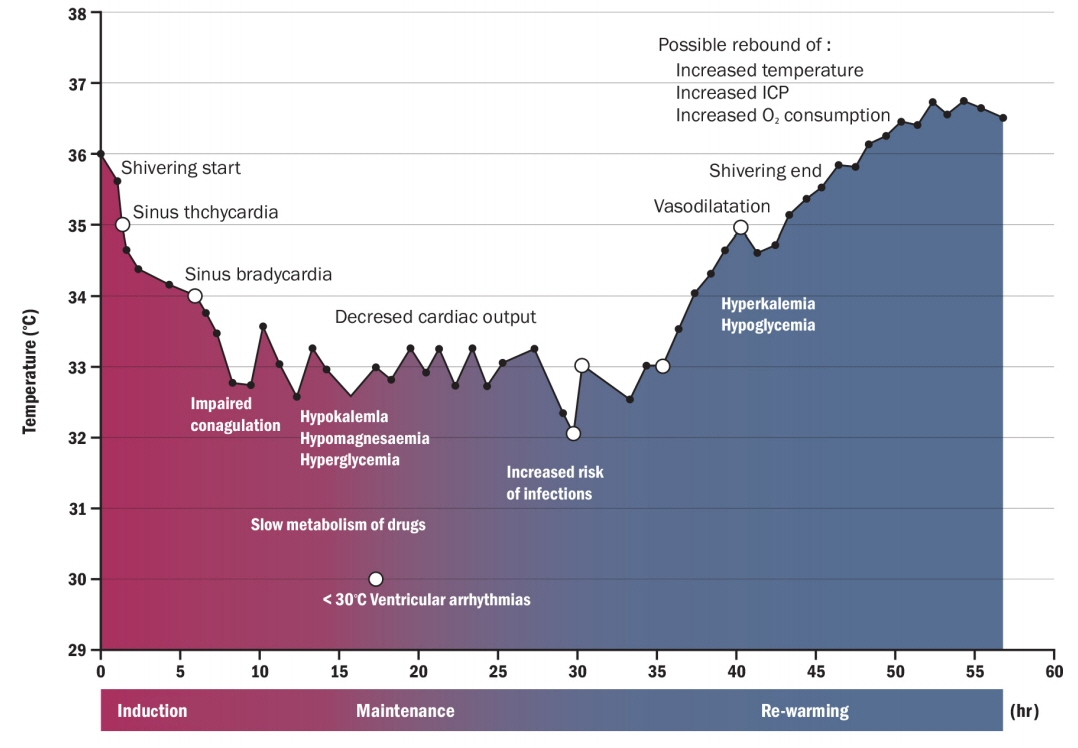
- Therapeutic hypothermia (TH) or targeted temperature management is an intentional cooling or temperature control technique using a thermostatic equipment (i.e., surface, endovascular, and focal devices) for specific therapeutic purposes. Given the modifiable determinants in the therapeutic process of acute ischemic stroke, hemorrhagic stroke, and subarachnoid hemorrhage, several studies strongly reported that fever is closely associated with more harmful neurological outcomes. Fever or hyperthermia can deteriorate the cellular ischemic cascade, causing more cerebral damage owing to increased metabolic demands, enhanced release of excitatory neurotransmitters, and increased toxic free radical production. Despite the disappointing results of various clinical trials on TH in the stroke field, many studies have repeatedly clarified its fundamental mechanisms, which proved its strong neuroprotection in experimental stroke models. In particular, the potential effectiveness of TH can be revisited in the era of endovascular thrombectomy for patients undergoing emergent large-vessel occlusion because neuroprotection is maximized in ischemia-reperfusion injury models. This review aims to incorporate current literature into risks and benefits in patients with ischemic stroke.
MeSH Terms
Figure
Reference
-
1. Markus HS. Cerebral perfusion and stroke. J Neurol Neurosurg Psychiatry. 2004; 75:353–61.
Article2. Heron M. Deaths: leading causes for 2004. Natl Vital Stat Rep. 2007; 56:1–95.3. Lallukka T, Ervasti J, Lundström E, Mittendorfer-Rutz E, Friberg E, Virtanen M, et al. Trends in diagnosis-specific work disability before and after stroke: a longitudinal population-based study in Sweden. J Am Heart Assoc. 2018; 7:e006991.
Article4. Catanese L, Tarsia J, Fisher M. Acute ischemic stroke therapy overview. Circ Res. 2017; 120:541–58.
Article5. Hossmann KA. Viability thresholds and the penumbra of focal ischemia. Ann Neurol. 1994; 36:557–65.
Article6. Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002; 346:557–63.
Article7. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346:549–56.
Article8. Shankaran S. Therapeutic hypothermia for neonatal encephalopathy. Curr Treat Options Neurol. 2012; 14:608–19.
Article9. Hong JM, Choi MH, Sohn SI, Hwang YH, Ahn SH, Lee YB, et al. Safety and optimal neuroprotection of neu2000 in acute ischemic stroke with recanalization: study protocol for a randomized, double-blinded, placebo-controlled, phase-II trial. Trials. 2018; 19:375.
Article10. Kurisu K, Yenari MA. Therapeutic hypothermia for ischemic stroke: pathophysiology and future promise. Neuropharmacology. 2018; 134:302–9.
Article11. Neugebauer H, Schneider H, Bösel J, Hobohm C, Poli S, Kollmar R, et al. Outcomes of hypothermia in addition to decompressive hemicraniectomy in treatment of malignant middle cerebral artery stroke: a randomized clinical trial. JAMA Neurol. 2019; 76:571–9.12. Polderman KH, Herold I. Therapeutic hypothermia and controlled normothermia in the intensive care unit: practical considerations, side effects, and cooling methods. Crit Care Med. 2009; 37:1101–20.
Article13. Polderman KH. Application of therapeutic hypothermia in the ICU: opportunities and pitfalls of a promising treatment modality. Part 1: indications and evidence. Intensive Care Med. 2004; 30:556–75.
Article14. Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 2009; 37:S186–202.
Article15. Andresen M, Gazmuri JT, Marín A, Regueira T, Rovegno M. Therapeutic hypothermia for acute brain injuries. Scand J Trauma Resusc Emerg Med. 2015; 23:42.
Article16. Badjatia N, Strongilis E, Gordon E, Prescutti M, Fernandez L, Fernandez A, et al. Metabolic impact of shivering during therapeutic temperature modulation: the Bedside Shivering Assessment Scale. Stroke. 2008; 39:3242–7.17. De Georgia MA, Krieger DW, Abou-Chebl A, Devlin TG, Jauss M, Davis SM, et al. Cooling for Acute Ischemic Brain Damage (COOL AID): a feasibility trial of endovascular cooling. Neurology. 2004; 63:312–7.
Article18. Hemmen TM, Raman R, Guluma KZ, Meyer BC, Gomes JA, Cruz-Flores S, et al. Intravenous thrombolysis plus hypothermia for acute treatment of ischemic stroke (ICTuS-L): final results. Stroke. 2010; 41:2265–70.19. Lyden PD, Hemmen TM, Grotta J, Rapp K, Raman R. Endovascular therapeutic hypothermia for acute ischemic stroke: ICTuS 2/3 protocol. Int J Stroke. 2014; 9:117–25.
Article20. Lyden P, Hemmen T, Grotta J, Rapp K, Ernstrom K, Rzesiewicz T, et al. Results of the ICTuS 2 trial (Intravascular Cooling in the Treatment of Stroke 2). Stroke. 2016; 47:2888–95.21. van der Worp HB, Macleod MR, Bath PM, Demotes J, Durand-Zaleski I, Gebhardt B, et al. EuroHYP-1: European multicenter, randomized, phase III clinical trial of therapeutic hypothermia plus best medical treatment vs. best medical treatment alone for acute ischemic stroke. Int J Stroke. 2014; 9:642–5.
Article22. Els T, Oehm E, Voigt S, Klisch J, Hetzel A, Kassubek J. Safety and therapeutical benefit of hemicraniectomy combined with mild hypothermia in comparison with hemicraniectomy alone in patients with malignant ischemic stroke. Cerebrovasc Dis. 2006; 21:79–85.
Article23. Schneider H, Krüger P, Algra A, Hofmeijer J, van der Worp HB, Jüttler E, et al. No benefits of hypothermia in patients treated with hemicraniectomy for large ischemic stroke. Int J Stroke. 2017; 12:732–40.
Article24. Fluri F, Schuhmann MK, Kleinschnitz C. Animal models of ischemic stroke and their application in clinical research. Drug Des Devel Ther. 2015; 9:3445–54.25. Perbet S, Mongardon N, Dumas F, Bruel C, Lemiale V, Mourvillier B, et al. Early-onset pneumonia after cardiac arrest: characteristics, risk factors and influence on prognosis. Am J Respir Crit Care Med. 2011; 184:1048–54.26. Kirkegaard H, Søreide E, de Haas I, Pettilä V, Taccone FS, Arus U, et al. Targeted temperature management for 48 vs 24 hours and neurologic outcome after out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2017; 318:341–50.27. Hong JM, Lee JS, Song HJ, Jeong HS, Choi HA, Lee K. Therapeutic hypothermia after recanalization in patients with acute ischemic stroke. Stroke. 2014; 45:134–40.
Article28. Jiang JY, Xu W, Li WP, Gao GY, Bao YH, Liang YM, et al. Effect of long-term mild hypothermia or short-term mild hypothermia on outcome of patients with severe traumatic brain injury. J Cereb Blood Flow Metab. 2006; 26:771–6.
Article29. Wijdicks EF, Sheth KN, Carter BS, Greer DM, Kasner SE, Kimberly WT, et al. Recommendations for the management of cerebral and cerebellar infarction with swelling: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:1222–38.30. van der Worp HB, Sena ES, Donnan GA, Howells DW, Macleod MR. Hypothermia in animal models of acute ischaemic stroke: a systematic review and meta-analysis. Brain. 2007; 130:3063–74.
Article31. Krieger DW, Yenari MA. Therapeutic hypothermia for acute ischemic stroke: what do laboratory studies teach us? Stroke. 2004; 35:1482–9.32. Markarian GZ, Lee JH, Stein DJ, Hong SC. Mild hypothermia: therapeutic window after experimental cerebral ischemia. Neurosurgery. 1996; 38:542–50.
Article33. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–31.
Article34. Hwang YH, Jeon JS, Kim YW, Kang DH, Kim YS, Liebeskind DS. Impact of immediate post-reperfusion cooling on outcome in patients with acute stroke and substantial ischemic changes. J Neurointerv Surg. 2017; 9:21–5.
Article35. Albers GW. Late window paradox. Stroke. 2018; 49:768–71.
Article36. Horn CM, Sun CH, Nogueira RG, Patel VN, Krishnan A, Glenn BA, et al. endovascular reperfusion and cooling in cerebral acute ischemia (ReCCLAIM I). J Neurointerv Surg. 2014; 6:91–5.
Article37. Rocha M, Jovin TG. Fast versus slow progressors of infarct growth in large vessel occlusion stroke: clinical and research implications. Stroke. 2017; 48:2621–7.38. Yoo AJ, Berkhemer OA, Fransen PSS, van den Berg LA, Beumer D, Lingsma HF, et al. Effect of baseline Alberta Stroke Program Early CT Score on safety and efficacy of intra-arterial treatment: a subgroup analysis of a randomised phase 3 trial (MR CLEAN). Lancet Neurol. 2016; 15:685–94.
Article39. Lee SJ, Lee KS, Lee JS, Choi MH, Lee SE, Hong JM. Primary neurocritical care involving therapeutic hypothermia for acute ischemic stroke patients with malignant infarct cores. J Neurocrit Care. 2019; 12:30–6.
Article40. Kuczynski AM, Demchuk AM, Almekhlafi MA. Therapeutic hypothermia: applications in adults with acute ischemic stroke. Brain Circ. 2019; 5:43–54.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Targeted temperature management in brain edema
- The Migraine-Stroke Connection
- A case of successful pediatric heat stroke treatment using normothermic targeted temperature management
- Early In-hospital Management of Acute Ischemic Stroke
- Targeted temperature management in a patient with suspected hypoxic-ischemic brain injury after successful resuscitation from cardiac arrest: a case report