J Neurocrit Care.
2022 Jun;15(1):65-68. 10.18700/jnc.220049.
Malignant cerebral infarction after COVID-19 myocarditis in 22-year-old female: a case report
- Affiliations
-
- 1Department of Neurology, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Neurosurgery, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2532003
- DOI: http://doi.org/10.18700/jnc.220049
Abstract
- Background
Ischemic stroke is one of the serious neurological complications of coronavirus disease 2019 (COVID-19). However, ischemic stroke can develop secondary complications after cardiac involvement in COVID-19.
Case Report
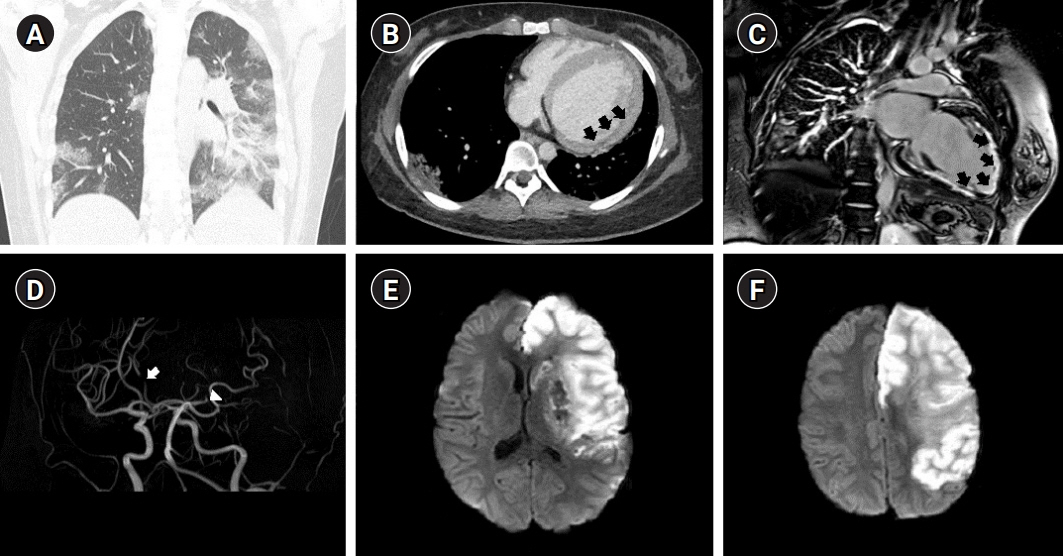
We report the case of a 22-year-old patient who presented with malignant cerebral infarction 10 months after COVID-19-related myocarditis. A 22-year-old woman was referred to the emergency room because of abnormal mental status changes. She developed heart failure and arrhythmia after COVID-19-related myocarditis. Brain magnetic resonance imaging (MRI) revealed high signal intensity on diffusion-weighted imaging that was indicative of acute cerebral infarction in the left middle cerebral artery (MCA) and left anterior cerebral artery (ACA) territory. In addition, occlusion of both the left MCA and ACA was observed on brain MRI. Craniectomy with therapeutic hypothermia was performed to treat the cerebral edema.
Conclusion
This case suggests that caution is needed in survivors with secondary complications after COVID-19.
Keyword
Figure
Reference
-
1. World Health Organization. Pneumonia of unknown cause: China. 2020. Geneva: World Health Organization;2021. [cited 2022 May 1]. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON229.2. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020; 5:831–40.
Article3. Sharifian-Dorche M, Huot P, Osherov M, Wen D, Saveriano A, Giacomini PS, et al. Neurological complications of coronavirus infection; a comparative review and lessons learned during the COVID-19 pandemic. J Neurol Sci. 2020; 417:117085.
Article4. Montalvan V, Toledo J, Nugent K. Mechanisms of stroke in coronavirus disease 2019. J Stroke. 2020; 22:282–3.
Article5. Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the epidemiology research council of the Korean Stroke Society. J Stroke. 2019; 21:42–59.
Article6. Caforio AL, Baritussio A, Basso C, Marcolongo R. Clinically suspected and biopsy-proven myocarditis temporally associated with SARS-CoV-2 infection. Annu Rev Med. 2022; 73:149–66.
Article7. Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res. 2020; 126:1443–55.
Article8. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med. 2020; 383:120–8.
Article9. Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020; 75:2352–71.
Article10. Kim IC, Kim JY, Kim HA, Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J. 2020; 41:1859.
Article11. Shantsila E, Kozieł M, Lip GY. Anticoagulation versus placebo for heart failure in sinus rhythm. Cochrane Database Syst Rev. 2021; 5:CD003336.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Myocarditis Presenting With a Hyperechoic Nodule After the First Dose of COVID-19 mRNA Vaccine
- Cerebral infarction caused by endocarditis in a patient with COVID-19
- Cardiovascular Magnetic Resonance Imaging of COVID-19 Myocarditis
- Cardiac Magnetic Resonance Imaging Findings and Clinical Features of COVID-19 Vaccine-Associated Myocarditis, Compared With Those of Other Types of Myocarditis
- Cardiovascular Manifestations of COVID-19