Endocrinol Metab.
2018 Sep;33(3):395-402. 10.3803/EnM.2018.33.3.395.
Effects of Maternal Iodine Status during Pregnancy and Lactation on Maternal Thyroid Function and Offspring Growth and Development: A Prospective Study Protocol for the Ideal Breast Milk Cohort
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 4Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Biomedical Science, Seoul National University Graduate School, Seoul, Korea.
- 6Department of Obstetrics and Gynecology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. jhs0927@snu.ac.kr
- 7Department of Food Service and Nutrition Care, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 8Department of Laboratory Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 9Department of Nuclear Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. jkchung@snu.ac.kr
- KMID: 2447030
- DOI: http://doi.org/10.3803/EnM.2018.33.3.395
Abstract
- BACKGROUND
Iodine is an intrinsic element of thyroid hormone, which is essential for childhood growth and development. The Ideal Breast Milk (IBM) cohort study aims to evaluate the effects of maternal iodine status during pregnancy and lactation on maternal thyroid function, offspring growth and development, and offspring thyroid function.
METHODS
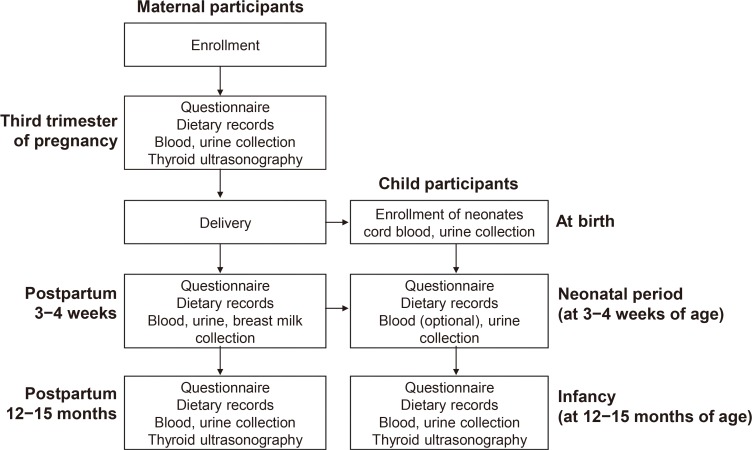
The IBM cohort study recruited pregnant women from Seoul National University Hospital between June 2016 and August 2017, followed by enrollment of their offspring after delivery. For the maternal participants, iodine status is evaluated by urinary iodine concentration (UIC) and dietary records in the third trimester and at 3 to 4 weeks and 12 to 15 months postpartum. For the child participants, cord blood sampling and UIC measurements are performed at birth. At 3 to 4 weeks of age, UIC and breastmilk iodine concentrations are measured. At 12 to 15 months of age, growth and development are assessed and measurements of UIC, a thyroid function test, and ultrasonography are performed.
RESULTS
A total of 198 pregnant women in their third trimester were recruited. Their mean age was 35.1±3.5 years, and 78 (39.4%) of them were pregnant with twins. Thirty-three (16.7%) of them had a previous history of thyroid disease.
CONCLUSION
Korea is an iodine-replete area. In particular, lactating women in Korea are commonly exposed to excess iodine due to the traditional practice of consuming brown seaweed soup postpartum. The study of the IBM cohort is expected to contribute to developing guidelines for optimal iodine nutrition in pregnant or lactating women.
Keyword
MeSH Terms
-
Breast*
Child
Cohort Studies*
Cordocentesis
Diet Records
Female
Growth and Development*
Humans
Infant
Iodine*
Korea
Lactation*
Milk, Human*
Parturition
Postpartum Period
Pregnancy Trimester, Third
Pregnancy*
Pregnant Women
Prospective Studies*
Seaweed
Seoul
Thyroid Diseases
Thyroid Function Tests
Thyroid Gland*
Twins
Ultrasonography
Iodine
Figure
Reference
-
1. Zimmermann MB, Andersson M. Update on iodine status worldwide. Curr Opin Endocrinol Diabetes Obes. 2012; 19:382–387. PMID: 22892867.
Article2. Leung AM, Braverman LE. Consequences of excess iodine. Nat Rev Endocrinol. 2014; 10:136–142. PMID: 24342882.
Article3. Wolff J, Chaikoff IL, Goldberg RC, Meier JR. The temporary nature of the inhibitory action of excess iodine on organic iodine synthesis in the normal thyroid. Endocrinology. 1949; 45:504–513. PMID: 15396709.4. Eng PH, Cardona GR, Fang SL, Previti M, Alex S, Carrasco N, et al. Escape from the acute Wolff-Chaikoff effect is associated with a decrease in thyroid sodium/iodide symporter messenger ribonucleic acid and protein. Endocrinology. 1999; 140:3404–3410. PMID: 10433193.5. Markou K, Georgopoulos N, Kyriazopoulou V, Vagenakis AG. Iodine-induced hypothyroidism. Thyroid. 2001; 11:501–510. PMID: 11396709.
Article6. Connelly KJ, Boston BA, Pearce EN, Sesser D, Snyder D, Braverman LE, et al. Congenital hypothyroidism caused by excess prenatal maternal iodine ingestion. J Pediatr. 2012; 161:760–762. PMID: 22841183.7. Shi X, Han C, Li C, Mao J, Wang W, Xie X, et al. Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7190 pregnant women in China. J Clin Endocrinol Metab. 2015; 100:1630–1638. PMID: 25629356.
Article8. Choi YS, Ock S, Kwon S, Jung SB, Seok KH, Kim YJ, et al. Excessive iodine status among school-age children in Korea: a first report. Endocrinol Metab (Seoul). 2017; 32:370–374. PMID: 28956367.
Article9. Han MR, Ju DL, Park YJ, Paik HY, Song Y. An iodine database for common Korean foods and the association between iodine intake and thyroid disease in Korean adults. Int J Thyroidol. 2015; 8:170–182.
Article10. Rhee SS, Braverman LE, Pino S, He X, Pearce EN. High iodine content of Korean seaweed soup: a health risk for lactating women and their infants? Thyroid. 2011; 21:927–928. PMID: 21745110.
Article11. Moon S, Kim J. Iodine content of human milk and dietary iodine intake of Korean lactating mothers. Int J Food Sci Nutr. 1999; 50:165–171. PMID: 10627832.12. Cho YY, Kim HJ, Oh SY, Choi SJ, Lee SY, Joung JY, et al. Iodine status in healthy pregnant women in Korea: a first report. Eur J Nutr. 2016; 55:469–475. PMID: 25750059.
Article13. Medici M, Ghassabian A, Visser W, de Muinck, Jaddoe VW, Visser WE, et al. Women with high early pregnancy urinary iodine levels have an increased risk of hyperthyroid newborns: the population-based Generation R Study. Clin Endocrinol (Oxf). 2014; 80:598–606. PMID: 23992400.
Article14. Yang J, Zhu L, Li X, Zheng H, Wang Z, Hao Z, et al. Maternal iodine status during lactation and infant weight and length in Henan Province, China. BMC Pregnancy Childbirth. 2017; 17:383. PMID: 29145827.
Article15. World Health Organization. Assessment of iodine deficiency disorders and monitoring their elimination. 3rd ed. Geneva: World Health Organization;2007.16. Leung AM, Avram AM, Brenner AV, Duntas LH, Ehrenkranz J, Hennessey JV, et al. Potential risks of excess iodine ingestion and exposure: statement by the American Thyroid Association Public Health Committee. Thyroid. 2015; 25:145–146. PMID: 25275241.
Article17. Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB. Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr. 2016; 104(Suppl 3):918S–923S. PMID: 27534632.
Article18. Chung HR, Shin CH, Yang SW, Choi CW, Kim BI. Subclinical hypothyroidism in Korean preterm infants associated with high levels of iodine in breast milk. J Clin Endocrinol Metab. 2009; 94:4444–4447. PMID: 19808851.
Article19. Liu L, Wang D, Liu P, Meng F, Wen D, Jia Q, et al. The relationship between iodine nutrition and thyroid disease in lactating women with different iodine intakes. Br J Nutr. 2015; 114:1487–1495. PMID: 26365041.
Article20. Pal N, Samanta SK, Chakraborty A, Chandra NK, Chandra AK. Interrelationship between iodine nutritional status of lactating mothers and their absolutely breast-fed infants in coastal districts of Gangetic West Bengal in India. Eur J Pediatr. 2018; 177:39–45. PMID: 29063209.21. Institute of Medicine Food and Nutrition Board. Dietary reference intakes. Washington, DC: National Academies Press;2006.22. Sang Z, Wei W, Zhao N, Zhang G, Chen W, Liu H, et al. Thyroid dysfunction during late gestation is associated with excessive iodine intake in pregnant women. J Clin Endocrinol Metab. 2012; 97:E1363–E1369. PMID: 22669304.
Article23. Aakre I, Bjoro T, Norheim I, Strand TA, Barikmo I, Henjum S. Excessive iodine intake and thyroid dysfunction among lactating Saharawi women. J Trace Elem Med Biol. 2015; 31:279–284. PMID: 25447589.
Article24. Aakre I, Strand TA, Bjoro T, Norheim I, Barikmo I, Ares S, et al. Thyroid function among breastfed children with chronically excessive iodine intakes. Nutrients. 2016; 8:E398. PMID: 27367720.
Article25. Yang XF, Xu J, Hou XH, Guo HL, Hao LP, Yao P, et al. Developmental toxic effects of chronic exposure to high doses of iodine in the mouse. Reprod Toxicol. 2006; 22:725–730. PMID: 16996244.
Article26. Nishiyama S, Mikeda T, Okada T, Nakamura K, Kotani T, Hishinuma A. Transient hypothyroidism or persistent hyperthyrotropinemia in neonates born to mothers with excessive iodine intake. Thyroid. 2004; 14:1077–1083. PMID: 15650362.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutrition in Breastfeeding: Infants and Nursing Mothers
- A Study on feeding Practices and Growth Status of Infants and the Correlation of Mothers' Perceptions of Breast Feeding with Infant Feeding Methods in the Pocheon Area
- Breastfeeding and Diabetes Mellitus/Thyroid Disease
- Autism-like Behaviors in Male Juvenile Offspring after Maternal Glyphosate Exposure
- Maternal exposure to airborne particulate matter during pregnancy and lactation induces kidney injury in rat dams and their male offspring: the role of vitamin D in pregnancy and beyond