Yonsei Med J.
2019 May;60(5):440-445. 10.3349/ymj.2019.60.5.440.
Bleeding Complications and Clinical Safety of Endoscopic Retrograde Cholangiopancreatography in Patients with Liver Cirrhosis
- Affiliations
-
- 1Department of Internal Medicine, Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea. bang7028@yuhs.ac
- KMID: 2443247
- DOI: http://doi.org/10.3349/ymj.2019.60.5.440
Abstract
- PURPOSE
Patients with liver cirrhosis are considered to be at risk for additional adverse events during endoscopic retrograde cholangiopancreatography (ERCP). The present study was designed as a propensity-score matched analysis to investigate whether cirrhotic liver increases the risk of bleeding complications in patients undergoing ERCP.
MATERIALS AND METHODS
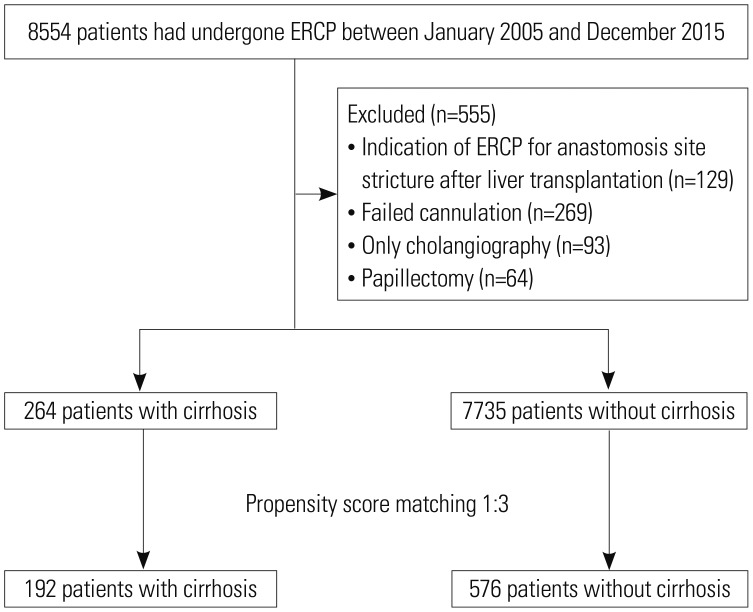
In total, 8554 patients who underwent ERCP from January 2005 to December 2015 were retrospectively analyzed. To adjust for the imbalance between patients with and those without liver cirrhosis, 1:3 propensity score matching was performed according to age and sex.
RESULTS
Liver cirrhosis was identified in 264 (3.1%) patients. After propensity score matching, a total of 768 patients were included in each of the cirrhotic (n=192) and non-cirrhotic groups (n=576). Post-procedure bleeding (10.9% vs. 4.7%, p=0.003) was more frequently observed in patients with liver cirrhosis than in those without. In multivariate analyses, liver cirrhosis was identified as an independent risk factor associated with post-ERCP bleeding (p=0.003) after further adjustment for prothrombin time, antiplatelet/coagulant, duration of ERCP, and stent insertion. Child-Pugh (CP) class C was found to be associated with an increased incidence of post-ERCP bleeding in patients with cirrhosis (odds ratio 6.144, 95% confidence interval 1.320-28.606; p=0.021).
CONCLUSION
The incidence of post-ERCP bleeding in patients with liver cirrhosis was higher than that in patients without liver cirrhosis. In particular, CP class C cirrhosis was significantly associated with post-ERCP bleeding.
MeSH Terms
Figure
Cited by 1 articles
-
Efficacy of intraoperative blood salvage and autotransfusion in living-donor liver transplantation: a retrospective cohort study
Jongchan Lee, Sujung Park, Jae Geun Lee, Sungji Choo, Bon-Nyeo Koo
Korean J Anesthesiol. 2024;77(3):345-352. doi: 10.4097/kja.23599.
Reference
-
1. Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005; 62:1–8. PMID: 15990812.
Article2. Sakai Y, Tsuyuguchi T, Sugiyama H, Nishikawa T, Tawada K, Saito M, et al. Current situation of endoscopic treatment for common bile duct stones. Hepatogastroenterology. 2012; 59:1712–1716. PMID: 22389270.
Article3. Tulassay Z, Zagoni T, Kotrlik J. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1997; 336:963. author reply 963-4. PMID: 9072704.
Article4. ASGE Standards of Practice Committee. Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben-Menachem T, et al. Complications of ERCP. Gastrointest Endosc. 2012; 75:467–473. PMID: 22341094.
Article5. Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007; 102:1781–1788. PMID: 17509029.
Article6. Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001; 96:417–423. PMID: 11232684.
Article7. Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998; 48:1–10. PMID: 9684657.
Article8. Wilcox CM, Canakis J, Mönkemüller KE, Bondora AW, Geels W. Patterns of bleeding after endoscopic sphincterotomy, the subsequent risk of bleeding, and the role of epinephrine injection. Am J Gastroenterol. 2004; 99:244–248. PMID: 15046211.
Article9. Nelson DB, Freeman ML. Major hemorrhage from endoscopic sphincterotomy: risk factor analysis. J Clin Gastroenterol. 1994; 19:283–287. PMID: 7876506.
Article10. Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918. PMID: 8782497.
Article11. Inamdar S, Berzin TM, Berkowitz J, Sejpal DV, Sawhney MS, Chutanni R, et al. Decompensated cirrhosis may be a risk factor for adverse events in endoscopic retrograde cholangiopancreatography. Liver Int. 2016; 36:1457–1463. PMID: 26913829.
Article12. Li DM, Zhao J, Zhao Q, Qin H, Wang B, Li RX, et al. Safety and efficacy of endoscopic retrograde cholangiopancreatography for common bile duct stones in liver cirrhotic patients. J Huazhong Univ Sci Technolog Med Sci. 2014; 34:612–615. PMID: 25135737.
Article13. Lee MH, Tsou YK, Lin CH, Lee CS, Liu NJ, Sung KF, et al. Predictors of re-bleeding after endoscopic hemostasis for delayed post-endoscopic sphincterotomy bleeding. World J Gastroenterol. 2016; 22:3196–3201. PMID: 27003996.
Article14. Adler DG, Haseeb A, Francis G, Kistler CA, Kaplan J, Ghumman SS, et al. Efficacy and safety of therapeutic ERCP in patients with cirrhosis: a large multicenter study. Gastrointest Endosc. 2016; 83:353–359. PMID: 26297868.
Article15. Zhang J, Ye L, Zhang J, Lin M, He S, Mao X, et al. MELD scores and Child-Pugh classifications predict the outcomes of ERCP in cirrhotic patients with choledocholithiasis: a retrospective cohort study. Medicine (Baltimore). 2015; 94:e433. PMID: 25621696.16. Prat F, Tennenbaum R, Ponsot P, Altman C, Pelletier G, Fritsch J, et al. Endoscopic sphincterotomy in patients with liver cirrhosis. Gastrointest Endosc. 1996; 43(2 Pt 1):127–131. PMID: 8635706.
Article17. Kawabe T, Komatsu Y, Tada M, Toda N, Ohashi M, Shiratori Y, et al. Endoscopic papillary balloon dilation in cirrhotic patients: removal of common bile duct stones without sphincterotomy. Endoscopy. 1996; 28:694–698. PMID: 8934088.
Article18. Park DH, Kim MH, Lee SK, Lee SS, Choi JS, Song MH, et al. Endoscopic sphincterotomy vs. endoscopic papillary balloon dilation for choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc. 2004; 60:180–185. PMID: 15278041.
Article19. Kim DY, Kim SU, Ahn SH, Park JY, Lee JM, Park YN, et al. Usefulness of FibroScan for detection of early compensated liver cirrhosis in chronic hepatitis B. Dig Dis Sci. 2009; 54:1758–1763. PMID: 19005758.
Article20. Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393. PMID: 2070995.
Article21. Mariante-Neto G, Marroni CP, Fleck AM Junior, Marroni CA, Zanotelli ML, Cantisani G, et al. Impact of creatinine values on MELD scores in male and female candidates for liver transplantation. Ann Hepatol. 2013; 12:434–439. PMID: 23619260.
Article22. Romano TG, Schmidtbauer I, Silva FM, Pompilio CE, D'Albuquerque LA, Macedo E. Role of MELD score and serum creatinine as prognostic tools for the development of acute kidney injury after liver transplantation. PLoS One. 2013; 8:e64089. PMID: 23717537.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety of endoscopic retrograde cholangiopancreatography (ERCP) in cirrhosis compared to non-cirrhosis and effect of Child-Pugh score on post-ERCP complications: a systematic review and meta-analysis
- Endoscopic retrograde cholangiopancreatography complications: Techniques to reduce risk and management strategies
- Endoscopic Retrograde Cholangiopancreatography during Pregnancy: Really Guarantee to Safety?
- Training in Endoscopy: Endoscopic Retrograde Cholangiopancreatography
- Successful Stone Removal by Endoscopic Retrograde Cholangiopancreatography in Situs Inversus Totalis with Billroth-II Gastrectomy