World J Mens Health.
2019 May;37(2):219-225. 10.5534/wjmh.180061.
Long-Term Experience of Sperm Cryopreservation in Cancer Patients in a Single Fertility Center
- Affiliations
-
- 1Department of Urology, Fertility Center of CHA Gangnam Medical Center, CHA University College of Medicine, Seoul, Korea. dngskkim100@gmail.com
- 2Department of Urology, CHA Fertility Center, Seoul Station, CHA University College of Medicine, Seoul, Korea.
- 3Fertility Center of CHA Gangnam Medical Center, CHA University College of Medicine, Seoul, Korea.
- 4Department of Obstetrics and Gynecology, Fertility Center of CHA Gangnam Medical Center, CHA University College of Medicine, Seoul, Korea.
- KMID: 2443237
- DOI: http://doi.org/10.5534/wjmh.180061
Abstract
- PURPOSE
Sperm cryopreservation before cancer treatment is the most effective method to preserve the fertility of male patients. We present our 21 years experience with sperm cryopreservation for cancer patients, including an examination of semen quality, the current status of cryopreserved sperm, and the rate of sperm use for assisted reproductive technology (ART).
MATERIALS AND METHODS
A total of 721 cancer patients at Fertility Center of CHA Gangnam Medical Center successfully performed sperm cryopreservation for fertility preservation from January 1996 to December 2016. Medical chart review was used to analyze patient age, marital status, cancer type, semen volume, sperm counts and motility, length of storage, and current banking status.
RESULTS
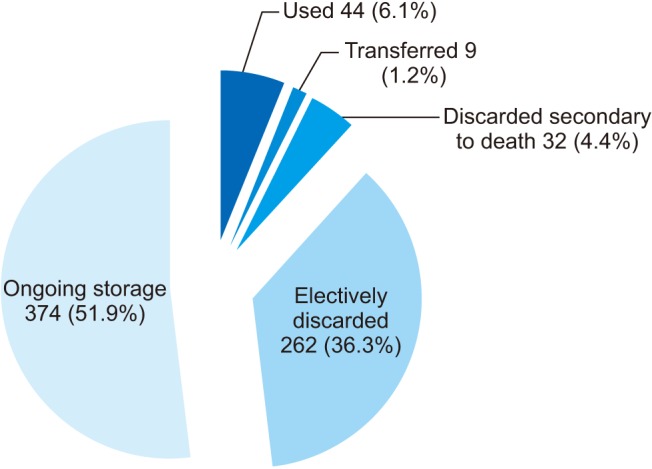
The major cancers of the 721 patients were leukemia (28.4%), lymphoma (18.3%), testis cancer (10.0%). The mean age at cryopreservation was 27.0 years, and 111 patients (15.4%) performed sperm cryopreservation during or after cancer treatment. The mean sperm concentration was 66.7±66.3 ×106/mL and the mean sperm motility was 33.8%±16.3%. During median follow-up duration of 75 months (range, 1-226 months), 44 patients (6.1%) used their banked sperm at our fertility center for ART and 9 patients (1.2%) transferred their banked sperm to another center. The median duration from cryopreservation to use was 51 months (range, 1-158 months).
CONCLUSIONS
Sperm cryopreservation before gonadotoxic treatment is the most reliable method to preserve the fertility of male cancer patients. Sperm cryopreservation should be offered as a standard of care for all men planning cancer therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Jung KW, Won YJ, Oh CM, Kong HJ, Lee DH, Lee KH. Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017; 49:292–305. PMID: 28279062.2. Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012; 62:220–241. PMID: 22700443.
Article3. Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013; 31:2500–2510. PMID: 23715580.
Article4. Trottmann M, Becker AJ, Stadler T, Straub J, Soljanik I, Schlenker B, et al. Semen quality in men with malignant diseases before and after therapy and the role of cryopreservation. Eur Urol. 2007; 52:355–367. PMID: 17498866.
Article5. Tomlinson M, Meadows J, Kohut T, Haoula Z, Naeem A, Pooley K, et al. Review and follow-up of patients using a regional sperm cryopreservation service: ensuring that resources are targeted to those patients most in need. Andrology. 2015; 3:709–716. PMID: 26084986.
Article6. Saito K, Suzuki K, Iwasaki A, Yumura Y, Kubota Y. Sperm cryopreservation before cancer chemotherapy helps in the emotional battle against cancer. Cancer. 2005; 104:521–524. PMID: 15968690.
Article7. World Health Organization. WHO laboratory manual for the examination of human semen and semen-cervical mucus interaction. 3rd ed. Cambridge: Cambridge University Press;1992.8. World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. Cambridge: Cambridge University Press;1999.9. World Health Organization. WHO laboratory manual for the examination of human semen. 5th ed. Geneva: World Health Organization;2010.10. Meistrich ML. Effects of chemotherapy and radiotherapy on spermatogenesis in humans. Fertil Steril. 2013; 100:1180–1186. PMID: 24012199.
Article11. Gandini L, Sgrò P, Lombardo F, Paoli D, Culasso F, Toselli L, et al. Effect of chemo-or radiotherapy on sperm parameters of testicular cancer patients. Hum Reprod. 2006; 21:2882–2889. PMID: 16997940.12. van der Kaaij MA, van Echten-Arends J, Simons AH, Kluin-Nelemans HC. Fertility preservation after chemotherapy for Hodgkin lymphoma. Hematol Oncol. 2010; 28:168–179. PMID: 20232475.
Article13. Pont J, Albrecht W. Fertility after chemotherapy for testicular germ cell cancer. Fertil Steril. 1997; 68:1–5. PMID: 9207575.
Article14. De Mas P, Daudin M, Vincent MC, Bourrouillou G, Calvas P, Mieusset R, et al. Increased aneuploidy in spermatozoa from testicular tumour patients after chemotherapy with cisplatin, etoposide and bleomycin. Hum Reprod. 2001; 16:1204–1208. PMID: 11387293.
Article15. Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in cancer patients. Fertil Steril. 2005; 83:1622–1628. PMID: 15950628.16. Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006; 24:2917–2931. PMID: 16651642.
Article17. Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002; 20:1890–1897. PMID: 11919249.
Article18. Menon S, Rives N, Mousset-Siméon N, Sibert L, Vannier JP, Mazurier S, et al. Fertility preservation in adolescent males: experience over 22 years at Rouen University Hospital. Hum Reprod. 2009; 24:37–44. PMID: 18945713.
Article19. Crha I, Ventruba P, Zakova J, Huser M, Kubesova B, Hudecek R, et al. Survival and infertility treatment in male cancer patients after sperm banking. Fertil Steril. 2009; 91:2344–2348. PMID: 18554588.
Article20. Ku JY, Park NC, Jeon TG, Park HJ. Semen analysis in cancer patients referred for sperm cryopreservation before chemotherapy over a 15-year period in Korea. World J Mens Health. 2015; 33:8–13. PMID: 25927057.
Article21. van Casteren NJ, Boellaard WP, Romijn JC, Dohle GR. Gonadal dysfunction in male cancer patients before cytotoxic treatment. Int J Androl. 2010; 33:73–79. PMID: 19538481.
Article22. Williams DH 4th, Karpman E, Sander JC, Spiess PE, Pisters LL, Lipshultz LI. Pretreatment semen parameters in men with cancer. J Urol. 2009; 181:736–740. PMID: 19091343.
Article23. Agarwal A, Allamaneni SS. Disruption of spermatogenesis by the cancer disease process. J Natl Cancer Inst Monogr. 2005; 9–12. PMID: 15784813.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Semen quality and sperm DNA fragmentation in cancer patients undergoing sperm cryopreservation
- The Need for Sperm Cryopreservation at the Time of Vasovasostomy or Vasoepididymostomy
- Fertility preservation in female cancer survivors
- Fertility preservation for women with malignancies: current developments of cryopreservation
- A Study on the Sperm Motility According to the Cryopreservation method of Human Semen