Korean J Gastroenterol.
2019 Mar;73(3):159-166. 10.4166/kjg.2019.73.3.159.
The Clinical Significance of Microsatellite Instability in Patients with Right-sided Colorectal Cancer
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea. parksj6406@daum.net
- KMID: 2442082
- DOI: http://doi.org/10.4166/kjg.2019.73.3.159
Abstract
- BACKGROUND/AIMS
Colorectal cancer (CRC) with microsatellite instability (MSI) has a better prognosis than CRC with microsatellite stable (MSS). Recent studies have reported biological differences according to tumor location in CRC. In this study, we investigated the clinical significance of MSI in patients with right-sided CRC.
METHODS
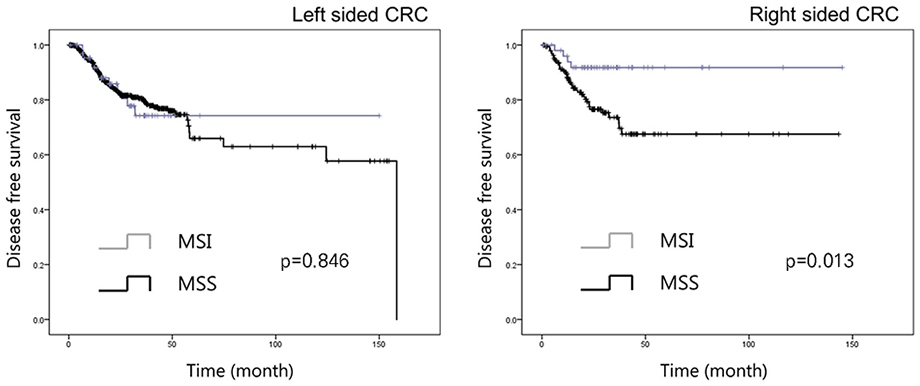
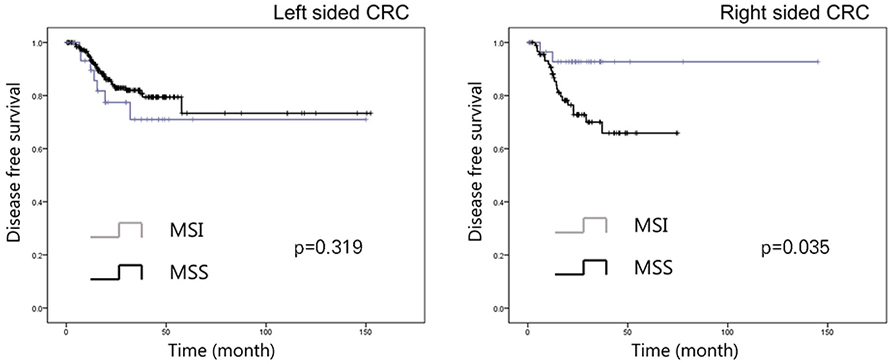
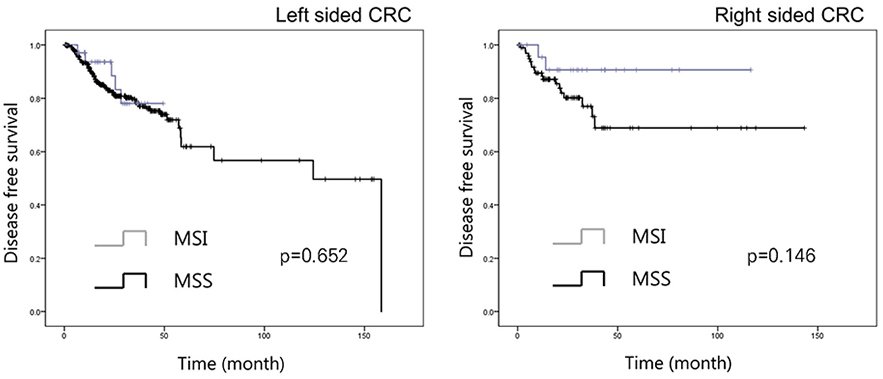
The medical records of 1,009 CRC patients diagnosed at our institute between October 2004 and December 2016 with MSI test results were retrospectively reviewed. The long-term outcomes of CRC patients with MSI were assessed with respect to tumor location using Kaplan-Meier curves and Cox regression models.
RESULTS
The median follow-up duration for all 1,009 study subjects was 25 months (interquartile range, 15-38). One hundred twenty-four of the study subjects had MSI (12.3%) and 250 had right-sided CRC (24.8%). The patients with MSI and right-sided CRC had better disease-free survival (DFS) than those with MSS as determined by the log-rank test (p=0.013), and this result was significant in females (p=0.035) but not in males with right-sided CRC. Multivariate Cox regression analysis showed MSS significantly predicted poor DFS in patients with right-sided CRC (hazard ratio 3.97, 95% CI 1.30-12.15, p=0.016) and in female patients (hazard ratio 4.69, 95% CI 1.03-21.36, p=0.045).
CONCLUSIONS
The study shows MSI is a useful predictor of DFS in patients with right-sided CRC, especially in female patients.
MeSH Terms
Figure
Reference
-
1. Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010; 116:544–573.
ArticleCancer Today: data visualization tools for exploring the global cancer burden in 2018. [Internet]. Lyon: International Association of Cancer Registries;c2018. cited 2018 Dec 20. Available from: https://gco.iarc.fr/today/home.3. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017; 67:7–30.
Article4. Loupakis F, Yang D, Yau L, et al. Primary tumor location as a prognostic factor in metastatic colorectal cancer. J Natl Cancer Inst. 2015; 107:dju427.
Article5. Boland CR, Goel A. Microsatellite instability in colorectal cancer. Gastroenterology. 2010; 138:2073–2087.e3.
Article6. Cortes-Ciriano I, Lee S, Park WY, Kim TM, Park PJ. A molecular portrait of microsatellite instability across multiple cancers. Nat Commun. 2017; 8:15180.
Article7. Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol. 2005; 23:609–618.
Article8. Aaltonen LA, Salovaara R, Kristo P, et al. Incidence of hereditary nonpolyposis colorectal cancer and the feasibility of molecular screening for the disease. N Engl J Med. 1998; 338:1481–1487.
Article9. Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017; 357:409–413.10. Le DT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015; 372:2509–2520.
Article11. Benedix F, Schmidt U, Mroczkowski P, et al. Colon carcinoma--classification into right and left sided cancer or according to colonic subsite?--analysis of 29,568 patients. Eur J Surg Oncol. 2011; 37:134–139.12. Venook AP, Niedzwiecki D, Innocenti F, et al. Impact of primary (1°) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): analysis of CALGB/SWOG 80405 (alliance). J Clin Oncol. 2016; 34:15 Suppl. 3504.
Article13. Tejpar S, Stintzing S, Ciardiello F, et al. Prognostic and predictive relevance of primary tumor location in patients with RAS wild-type metastatic colorectal cancer: retrospective analyses of the CRYSTAL and FIRE-3 trials. JAMA Oncol. 2017; 3:194–201.14. Sinicrope FA, Foster NR, Thibodeau SN, et al. DNA mismatch repair status and colon cancer recurrence and survival in clinical trials of 5-fluorouracil-based adjuvant therapy. J Natl Cancer Inst. 2011; 103:863–875.15. Sargent DJ, Marsoni S, Monges G, et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol. 2010; 28:3219–3226.16. NCCN guidelines® & clinical resources. [Internet]. Plymouth Meeting (PA): National Comprehensive Cancer Network;c2018. updated 2018 Oct 19. cited 2018 Dec 20. Available from: https://www.nccn.org/professionals/physician_gls/default.aspx#colon.17. Pawlik TM, Raut CP, Rodriguez-Bigas MA. Colorectal carcinogenesis: MSI-H versus MSI-L. Dis Markers. 2004; 20:199–206.
Article18. Nazemalhosseini Mojarad E, Kashfi SM, Mirtalebi H, et al. Low level of microsatellite instability correlates with poor clinical prognosis in stage II colorectal cancer patients. J Oncol. 2016; 2016:2196703.19. Nawa T, Kato J, Kawamoto H, et al. Differences between right- and left-sided colon cancer in patient characteristics, cancer morphology and histology. J Gastroenterol Hepatol. 2008; 23:418–423.
Article20. Roncucci L, Fante R, Losi L, et al. Survival for colon and rectal cancer in a population-based cancer registry. Eur J Cancer. 1996; 32A:295–302.
Article21. Weiss JM, Pfau PR, O'Connor ES, et al. Mortality by stage for rightversus left-sided colon cancer: analysis of surveillance, epidemiology, and end results--medicare data. J Clin Oncol. 2011; 29:4401–4409.22. Yahagi M, Okabayashi K, Hasegawa H, Tsuruta M, Kitagawa Y. The worse prognosis of right-sided compared with left-sided colon cancers: a systematic review and meta-analysis. J Gastrointest Surg. 2016; 20:648–655.
Article23. Liu F, Jiao Y, Jiao Y, Garcia-Godoy F, Gu W, Liu Q. Sex difference in EGFR pathways in mouse kidney-potential impact on the immune system. BMC Genet. 2016; 17:146.
Article24. Wang L, Xiao J, Gu W, Chen H. Sex difference of egfr expression and molecular pathway in the liver: impact on drug design and cancer treatments. J Cancer. 2016; 7:671–680.
Article25. Paulson EC, Wirtalla C, Armstrong K, Mahmoud NN. Gender influences treatment and survival in colorectal cancer surgery. Dis Colon Rectum. 2009; 52:1982–1991.
Article26. Yang Y, Wang G, He J, et al. Gender differences in colorectal cancer survival: a meta-analysis. Int J Cancer. 2017; 141:1942–1949.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinicopathological Significance of Microsatellite Instability in Sporadic Colorectal Cancer
- Hereditary Nonpolyposis Colorectal Cancer
- Genomic Instability in Colorectal Cancer; from Bench to Bed
- Impact of Microsatellite Instability in Signet-Ring Cell and Mucinous Components in Patients With Colorectal Carcinoma
- Understanding of molecular pathogenesis and genetic markers in colorectal cancer