Tuberc Respir Dis.
2019 Jan;82(1):53-61. 10.4046/trd.2018.0045.
Clinical Phenotype of a First Unprovoked Acute Pulmonary Embolism Associated with Antiphospholipid Antibody Syndrome
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Chosun University Hospital, Gwangju, Korea.
- 2Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Rheumatology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Pulmonary and Critical Care Medicine, Center for Pulmonary Hypertension and Venous Thrombosis, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jsdoc1186@daum.net
- KMID: 2441730
- DOI: http://doi.org/10.4046/trd.2018.0045
Abstract
- BACKGROUND
Antiphospholipid antibody syndrome (APS), an important cause of acquired thrombophilia, is diagnosed when vascular thrombosis or pregnancy morbidity occurs with persistently positive antiphospholipid antibodies (aPL). APS is a risk factor for unprovoked recurrence of pulmonary embolism (PE). Performing laboratory testing for aPL after a first unprovoked acute PE is controversial. We investigated if a specific phenotype existed in patients with unprovoked with acute PE, suggesting the need to evaluate them for APS.
METHODS
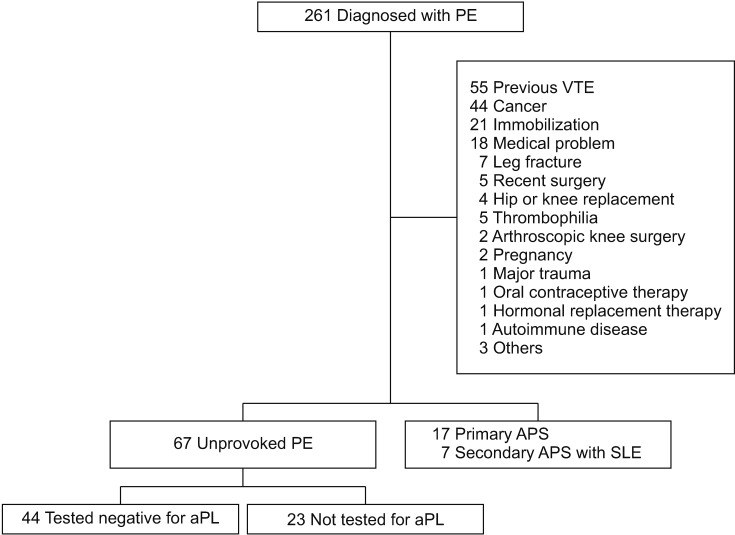
We retrospectively reviewed patients with PE and APS (n=24) and those with unprovoked PE with aPL negative (n=44), evaluated 2006-2016 at the Asan Medical Center. We compared patient demographics, clinical manifestations, laboratory findings, and radiological findings between the groups.
RESULTS
On multivariate logistic regression analysis, two models of independent risk factors for APS-PE were suggested. Model I included hemoptysis (odds ratio [OR], 12.897; 95% confidence interval [CI], 1.025-162.343), low PE severity index (OR, 0.948; 95% CI, 0.917-0.979), and activated partial thromboplastin time (aPTT; OR, 1.166; 95% CI, 1.040-1.307). Model II included age (OR, 0.930; 95% CI, 0.893-0.969) and aPTT (OR, 1.104; 95% CI, 1.000-1.217).
CONCLUSION
We conclude that patients with first unprovoked PE with hemoptysis and are age <40; have a low pulmonary embolism severity index, especially in risk class I-II; and/or prolonged aPTT (above 75th percentile of the reference interval), should be suspected of having APS, and undergo laboratory testing for aPL.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Incidence and Risk Factors of Recurrent Venous Thromboembolism after Pulmonary Embolism
Hun-Gyu Hwang, Won-Il Choi, Bora Lee, Choong Won Lee
Tuberc Respir Dis. 2019;82(4):341-347. doi: 10.4046/trd.2019.0019.
Reference
-
1. Iorio A, Kearon C, Filippucci E, Marcucci M, Macura A, Pengo V, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010; 170:1710–1716. PMID: 20975016.
Article2. Kearon C, Akl EA. Duration of anticoagulant therapy for deep vein thrombosis and pulmonary embolism. Blood. 2014; 123:1794–1801. PMID: 24497538.
Article3. Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galie N, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014; 35:3033–3069. PMID: 25173341.4. Zhu T, Martinez I, Emmerich J. Venous thromboembolism: risk factors for recurrence. Arterioscler Thromb Vasc Biol. 2009; 29:298–310. PMID: 19228602.5. Kyrle PA, Rosendaal FR, Eichinger S. Risk assessment for recurrent venous thrombosis. Lancet. 2010; 376:2032–2039. PMID: 21131039.
Article6. Heit JA. Predicting the risk of venous thromboembolism recurrence. Am J Hematol. 2012; 87(Suppl 1):S63–S67. PMID: 22367958.
Article7. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006; 4:295–306. PMID: 16420554.
Article8. Petri M. Epidemiology of the antiphospholipid antibody syndrome. J Autoimmun. 2000; 15:145–151. PMID: 10968901.
Article9. Asherson RA, Cervera R. Review: antiphospholipid antibodies and the lung. J Rheumatol. 1995; 22:62–66. PMID: 7699684.10. Espinosa G, Cervera R, Font J, Asherson RA. The lung in the antiphospholipid syndrome. Ann Rheum Dis. 2002; 61:195–198. PMID: 11830421.11. Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016; 149:315–352. PMID: 26867832.12. Mirrakhimov AE, Hill NS. Primary antiphospholipid syndrome and pulmonary hypertension. Curr Pharm Des. 2014; 20:545–551. PMID: 23565637.
Article13. Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, Brey R, Crowther M, Derksen R, et al. Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International Congress on antiphospholipid antibodies. Lupus. 2011; 20:206–218. PMID: 21303837.
Article14. Galli M, Luciani D, Bertolini G, Barbui T. Lupus anticoagulants are stronger risk factors for thrombosis than anticardiolipin antibodies in the antiphospholipid syndrome: a systematic review of the literature. Blood. 2003; 101:1827–1832. PMID: 12393574.
Article15. Keeling D, Mackie I, Moore GW, Greer IA, Greaves M. British Committee for Standards in Haematology. Guidelines on the investigation and management of antiphospholipid syndrome. Br J Haematol. 2012; 157:47–58. PMID: 22313321.
Article16. Pengo V, Tripodi A, Reber G, Rand JH, Ortel TL, Galli M, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2009; 7:1737–1740. PMID: 19624461.17. Aujesky D, Obrosky DS, Stone RA, Auble TE, Perrier A, Cornuz J, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med. 2005; 172:1041–1046. PMID: 16020800.
Article18. Chan CM, Woods C, Shorr AF. The validation and reproducibility of the pulmonary embolism severity index. J Thromb Haemost. 2010; 8:1509–1514. PMID: 20403093.
Article19. Boyden EA. Segmental anatomy of the lungs. New York: McGraw-Hill;1955.20. Mchrani T, Petri M. Epidemiology of the antiphospholipid syndrome. In : Asherson RA, editor. Handbook of systemic autoimmune diseases. Vol. 10. Amsterdam: Elsevier;2009. p. 13–34.21. Gomez-Puerta JA, Cervera R. Diagnosis and classification of the antiphospholipid syndrome. J Autoimmun. 2014; 48-49:20–25. PMID: 24461539.22. Piette JC, Cacoub P. Antiphospholipid syndrome in the elderly: caution. Circulation. 1998; 97:2195–2196. PMID: 9631867.
Article23. Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003; 107(23 Suppl 1):I9–16. PMID: 12814980.
Article24. Pollack CV, Schreiber D, Goldhaber SZ, Slattery D, Fanikos J, O'Neil BJ, et al. Clinical characteristics, management, and outcomes of patients diagnosed with acute pulmonary embolism in the emergency department: initial report of EMPEROR (Multicenter Emergency Medicine Pulmonary Embolism in the Real World Registry). J Am Coll Cardiol. 2011; 57:700–706. PMID: 21292129.25. He H, Stein MW, Zalta B, Haramati LB. Pulmonary infarction: spectrum of findings on multidetector helical CT. J Thorac Imaging. 2006; 21:1–7. PMID: 16538148.26. Tsao MS, Schraufnagel D, Wang NS. Pathogenesis of pulmonary infarction. Am J Med. 1982; 72:599–606. PMID: 6462058.
Article27. Miniati M, Bottai M, Ciccotosto C, Roberto L, Monti S. Predictors of pulmonary infarction. Medicine (Baltimore). 2015; 94:e1488. PMID: 26469892.
Article28. Weng CT, Chung TJ, Liu MF, Weng MY, Lee CH, Chen JY, et al. A retrospective study of pulmonary infarction in patients with systemic lupus erythematosus from southern Taiwan. Lupus. 2011; 20:876–885. PMID: 21693494.
Article29. Thrombosis and thrombocytopenia in antiphospholipid syndrome (idiopathic and secondary to SLE): first report from the Italian Registry. Italian Registry of Antiphospholipid Antibodies (IR-APA). Haematologica. 1993; 78:313–318. PMID: 8314161.30. Cuadrado MJ, Mujic F, Munoz E, Khamashta MA, Hughes GR. Thrombocytopenia in the antiphospholipid syndrome. Ann Rheum Dis. 1997; 56:194–196. PMID: 9135225.
Article31. Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, Camps MT, et al. Antiphospholipid syndrome: clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum. 2002; 46:1019–1027. PMID: 11953980.
Article32. Uthman I, Godeau B, Taher A, Khamashta M. The hematologic manifestations of the antiphospholipid syndrome. Blood Rev. 2008; 22:187–194. PMID: 18417261.
Article33. Abo SM, DeBari VA. Laboratory evaluation of the antiphospholipid syndrome. Ann Clin Lab Sci. 2007; 37:3–14. PMID: 17311864.34. Donze J, Le Gal G, Fine MJ, Roy PM, Sanchez O, Verschuren F, et al. Prospective validation of the Pulmonary Embolism Severity Index: a clinical prognostic model for pulmonary embolism. Thromb Haemost. 2008; 100:943–948. PMID: 18989542.35. Streiff MB, Agnelli G, Connors JM, Crowther M, Eichinger S, Lopes R, et al. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb Thrombolysis. 2016; 41:32–67. PMID: 26780738.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiphospholipid Syndrome Presented with Pulmonary Embolism and Deep Venous Thrombosis in Child
- Recurrent Systemic Embolizetion Caused by Aortic Thrombus in Antiphospholipid Antibody syndrome: A Case Report
- A Case of Antiphospholipid Syndrome Refractory to Secondary Anticoagulating Prophylaxis after Deep Vein Thrombosis-Pulmonary Embolism
- A Case of Primary Antiphospholipid Syndrome with Pulmonary Thromboembolism
- Antiphospholipid Antibody Syndrome