Ann Rehabil Med.
2019 Feb;43(1):54-61. 10.5535/arm.2019.43.1.54.
Long-Term Efficacy of Mirabegron Add-On Therapy to Antimuscarinic Agents in Patients With Spinal Cord Injury
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, National Rehabilitation Center, Seoul, Korea. iambs@nrc.go.kr
- 2Department of Physical Medicine and Rehabilitation, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2440952
- DOI: http://doi.org/10.5535/arm.2019.43.1.54
Abstract
OBJECTIVE
To evaluate the long-term efficacy of mirabegron add-on therapy in patients with spinal cord injury (SCI) based on an urodynamic study.
METHODS
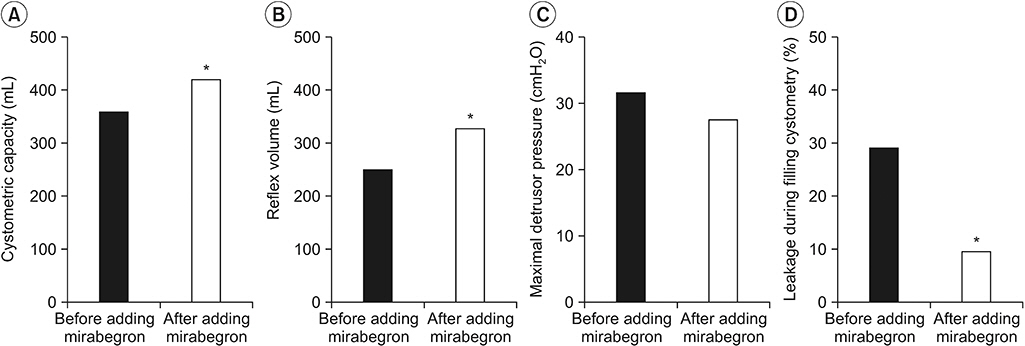
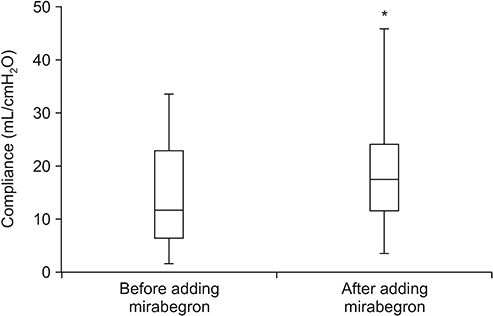
This retrospective study involved a chart audit of individuals with SCI who underwent two consecutive urodynamic studies between April 1, 2015 and April 1, 2018. After adding 50 mg of mirabegron once a day to the pre-existing antimuscarinic therapy for a period of, at least 6 months, the following variables were analyzed: change in cystometric capacity, change in bladder compliance, change in maximal detrusor pressure, change in reflex volume, and presence of significant leakage during filling cystometry.
RESULTS
A total of 31 participants with a mean age of 41±15 years were included in the analysis. A significant increase in cystometric capacity (mean, 362 to 424 mL; p=0.03), reflex volume (mean, 251 to 329 mL; p=0.02), and bladder compliance (median, 12 to 18 mL/cmHâ‚‚O; p=0.04) was observed. The presence of leakage during filling cystometry was significantly reduced (29% to 10%; p=0.03). Likewise, a non-significant decrease in the change in maximal detrusor pressure was observed (mean, 31 to 27 cmHâ‚‚O; p=0.39).
CONCLUSION
Adding mirabegron to conventional antimuscarinics further improved urodynamic parameters in patients with chronic SCI, and sustained efficacy was observed in long-term use.
MeSH Terms
Figure
Reference
-
1. Gerridzen RG, Thijssen AM, Dehoux E. Risk factors for upper tract deterioration in chronic spinal cord injury patients. J Urol. 1992; 147:416–8.
Article2. Goldmark E, Niver B, Ginsberg DA. Neurogenic bladder: from diagnosis to management. Curr Urol Rep. 2014; 15:448.
Article3. Abrams P, Artibani W, Gajewski JB, Hussain I. Assessment of treatment outcomes in patients with overactive bladder: importance of objective and subjective measures. Urology. 2006; 68(2 Suppl):17–28.
Article4. del Popolo G, Mencarini M, Nelli F, Lazzeri M. Controversy over the pharmacological treatments of storage symptoms in spinal cord injury patients: a literature overview. Spinal Cord. 2012; 50:8–13.
Article5. Benner JS, Nichol MB, Rovner ES, Jumadilova Z, Alvir J, Hussein M, et al. Patient-reported reasons for discontinuing overactive bladder medication. BJU Int. 2010; 105:1276–82.
Article6. Maman K, Aballea S, Nazir J, Desroziers K, Neine ME, Siddiqui E, et al. Comparative efficacy and safety of medical treatments for the management of overactive bladder: a systematic literature review and mixed treatment comparison. Eur Urol. 2014; 65:755–65.
Article7. Wollner J, Pannek J. Initial experience with the treatment of neurogenic detrusor overactivity with a new β-3 agonist (mirabegron) in patients with spinal cord injury. Spinal Cord. 2016; 54:78–82.
Article8. Kirshblum S, Waring W 3rd. Updates for the international standards for neurological classification of spinal cord injury. Phys Med Rehabil Clin N Am. 2014; 25:505–17.
Article9. Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2011; 34:547–54.
Article10. Yamanishi T, Sakakibara R, Uchiyama T, Hirata K. Role of urodynamic studies in the diagnosis and treatment of lower urinary tract symptoms. Urol Sci. 2011; 22:120–8.
Article11. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003; 61:37–49.
Article12. Homma Y, Batista J, Bauer S, Griffiths D, Hilton P, Kramer G, et al. Urodynamics. Incontinence: the 2nd International consultation on incontinence. Plymouth, UK: Plymbridge Distributors;2002. p. 317–72.13. Krebs J, Pannek J. Effects of solifenacin in patients with neurogenic detrusor overactivity as a result of spinal cord lesion. Spinal Cord. 2013; 51:306–9.
Article14. Kim J, Seo BS. How to calculate sample size and why. Clin Orthop Surg. 2013; 5:235–42.
Article15. Rosner B. Fundamentals of biostatistics. 4th ed. Belmont: Duxbury Press;1995.16. Ginsberg D. The epidemiology and pathophysiology of neurogenic bladder. Am J Manag Care. 2013; 19(10 Suppl):s191–6.17. Panicker JN, Fowler CJ, Kessler TM. Lower urinary tract dysfunction in the neurological patient: clinical assessment and management. Lancet Neurol. 2015; 14:720–32.
Article18. Groen J, Pannek J, Castro Diaz D, Del Popolo G, Gross T, Hamid R, et al. Summary of European Association of Urology (EAU) guidelines on neuro-urology. Eur Urol. 2016; 69:324–33.
Article19. Stohrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G, Kramer G, et al. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol. 2009; 56:81–8.20. Stohrer M, Murtz G, Kramer G, Schnabel F, Arnold EP, Wyndaele JJ, et al. Propiverine compared to oxybutynin in neurogenic detrusor overactivity: results of a randomized, double-blind, multicenter clinical study. Eur Urol. 2007; 51:235–42.21. Staskin DR, MacDiarmid SA. Using anticholinergics to treat overactive bladder: the issue of treatment tolerability. Am J Med. 2006; 119(3 Suppl 1):9–15.
Article22. Nitti VW, Dmochowski R, Appell RA, Wang JT, Bavendam T, Guan Z, et al. Efficacy and tolerability of tolterodine extended-release in continent patients with overactive bladder and nocturia. BJU Int. 2006; 97:1262–6.
Article23. Amend B, Hennenlotter J, Schafer T, Horstmann M, Stenzl A, Sievert KD. Effective treatment of neurogenic detrusor dysfunction by combined high-dosed antimuscarinics without increased side-effects. Eur Urol. 2008; 53:1021–8.
Article24. Takeda M, Obara K, Mizusawa T, Tomita Y, Arai K, Tsutsui T, et al. Evidence for beta3-adrenoceptor subtypes in relaxation of the human urinary bladder detrusor: analysis by molecular biological and pharmacological methods. J Pharmacol Exp Ther. 1999; 288:1367–73.25. Yamaguchi O. Beta3-adrenoceptors in human detrusor muscle. Urology. 2002; 59(5 Suppl 1):25–9.26. Madhuvrata P, Singh M, Hasafa Z, Abdel-Fattah M. Anticholinergic drugs for adult neurogenic detrusor overactivity: a systematic review and meta-analysis. Eur Urol. 2012; 62:816–30.
Article27. Matsukawa Y, Takai S, Funahashi Y, Yamamoto T, Gotoh M. Urodynamic evaluation of the efficacy of mirabegron on storage and voiding functions in women with overactive bladder. Urology. 2015; 85:786–90.
Article28. Vecchioli Scaldazza C, Morosetti C. Comparison of therapeutic efficacy and urodynamic findings of solifenacin succinate versus mirabegron in women with overactive bladder syndrome: results of a randomized controlled study. Urol Int. 2016; 97:325–9.
Article29. Wada N, Iuchi H, Kita M, Hashizume K, Matsumoto S, Kakizaki H. Urodynamic efficacy and safety of mirabegron add-on treatment with tamsulosin for Japanese male patients with overactive bladder. Low Urin Tract Symptoms. 2016; 8:171–6.
Article30. Krhut J, Borovicka V, Bilkova K, Sykora R, Mika D, Mokris J, et al. Efficacy and safety of mirabegron for the treatment of neurogenic detrusor overactivity-Prospective, randomized, double-blind, placebocontrolled study. Neurourol Urodyn. 2018; 37:2226–33.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Additional low-dose antimuscarinics can improve overactive bladder symptoms in patients with suboptimal response to beta 3 agonist monotherapy
- Current Concept and Future of the Management of Spinal Cord Injury: A Systematic Review
- Anemia in the Acute Phase of Traumatic Spinal Cord Injury
- A Case Report of Spinal Cord Injury Patient From a High Velocity Gunshot Wound to the Lumbar Spine
- Meta-Analysis of the Efficacy and Safety of Mirabegron Add-On Therapy to Solifenacin for Overactive Bladder