Ann Rehabil Med.
2019 Feb;43(1):19-26. 10.5535/arm.2019.43.1.19.
Transabdominal Functional Magnetic Stimulation for the Treatment of Constipation in Brain-Injured Patients: A Randomized Controlled Trial
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Presbyterian Medical Center, Jeonju, Korea. rytt@naver.com
- 2Medical Device Clinical Trial Center, Presbyterian Medical Center, Jeonju, Korea.
- 3Department of Internal Medicine, Presbyterian Medical Center, Jeonju, Korea.
- KMID: 2440948
- DOI: http://doi.org/10.5535/arm.2019.43.1.19
Abstract
OBJECTIVE
To investigate the effects of the transabdominal functional magnetic stimulation (A-FMS) for constipation in stroke or brain-injured patients.
METHODS
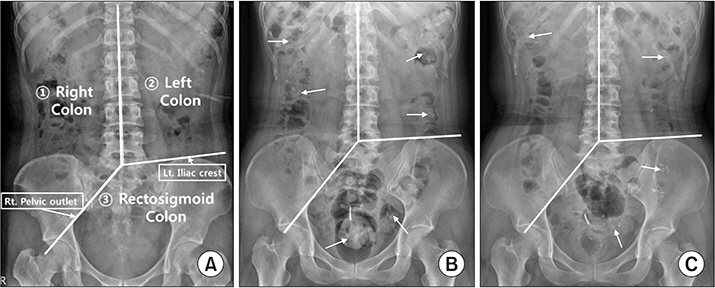
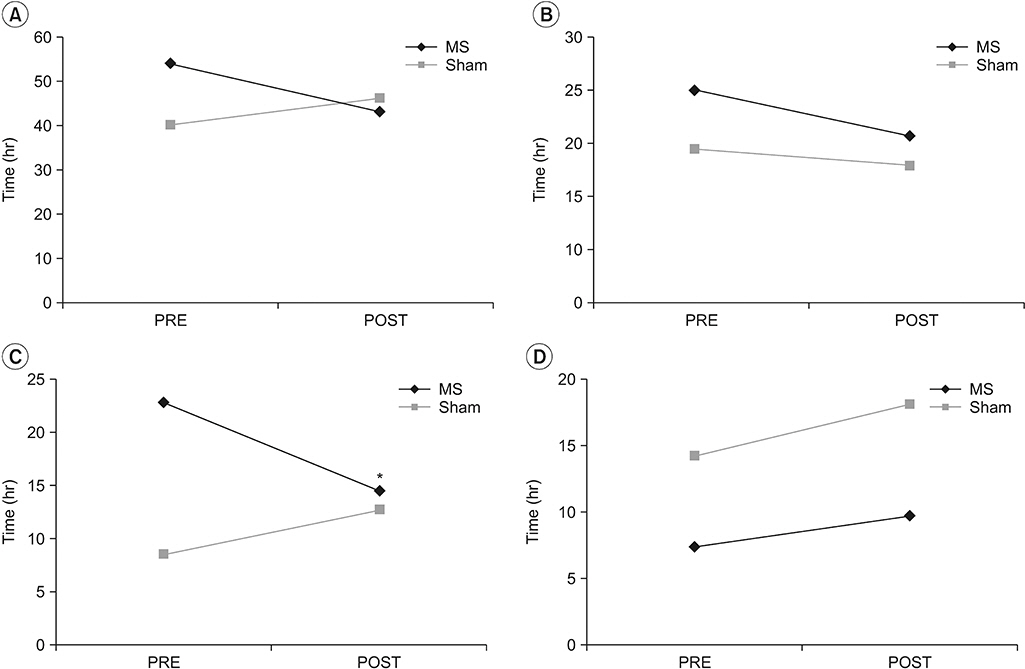
Twenty-four brain-injured patients (11 males and 13 females; median age, 65 years; 22 cases of stroke and 2 cases of traumatic brain injury) with constipation, who were admitted to the rehabilitation department, were enrolled and randomly divided into magnetic stimulation (MS) group and sham stimulation (Sham) group. Several parameters related with constipation such as total and segmental colon transit time (CTT), defecation frequency, and Bristol Stool Scale (BSS) before and after 2 weeks of A-FMS (5 times per week, total 10 times of A-FMS) were evaluated. The Korean version of the Modified Barthel Index (K-MBI) was also evaluated.
RESULTS
A significant decrease in segmental CTT in the left colon (-8.2±3.9 vs. 4.1±2.5 hours; p < 0.05 by paired sample t-test) and a significant increase in the frequency of defecation (1.5±0.2 vs 0.7±0.3; p < 0.05 by paired sample t-test) were observed in the MS group compared with the Sham group. Stool hardness became significantly softer in the MS group compared with the Sham group (2.3-3.5 in the MS and 2.6-3.1 in the Sham; p < 0.05 by chi-square test) as evaluated by BSS. No difference in the K-MBI was observed between the two groups.
CONCLUSION
The present study suggests that A-FMS can be an additional therapeutic tool for managing constipation in brain-injured patients with abnormal bowel movement, defecation frequency, and stool hardness.
MeSH Terms
Figure
Reference
-
1. Stewart WF, Liberman JN, Sandler RS, Woods MS, Stemhagen A, Chee E, et al. Epidemiology of constipation (EPOC) study in the United States: relation of clinical subtypes to sociodemographic features. Am J Gastroenterol. 1999; 94:3530–40.
Article2. Pare P, Ferrazzi S, Thompson WG, Irvine EJ, Rance L. An epidemiological survey of constipation in Canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol. 2001; 96:3130–7.
Article3. Hollerbach S, Kamath MV, Lock G, Scholmerich J, Upton AR, Tougas G. Assessment of afferent gut: brain function using cerebral evoked responses to esophageal stimulation. Z Gastroenterol. 1998; 36:313–24.4. Karakula-Juchnowicz H, Dzikowski M, Pelczarska A, Dzikowska I, Juchnowicz D. The brain-gut axis dysfunctions and hypersensitivity to food antigens in the etiopathogenesis of schizophrenia. Psychiatr Pol. 2016; 50:747–60.
Article5. Li J, Yuan M, Liu Y, Zhao Y, Wang J, Guo W. Incidence of constipation in stroke patients: a systematic review and meta-analysis. Medicine (Baltimore). 2017; 96:e7225.6. Lin CJ, Hung JW, Cho CY, Tseng CY, Chen HY, Lin FC, et al. Poststroke constipation in the rehabilitation ward: incidence, clinical course and associated factors. Singapore Med J. 2013; 54:624–9.
Article7. Camara-Lemarroy CR, Ibarra-Yruegas BE, Gongora-Rivera F. Gastrointestinal complications after ischemic stroke. J Neurol Sci. 2014; 346:20–5.
Article8. Lin VM, Frost FS, Lee SB, Cadwell J. High-frequency magnetic stimulation of the bowel in man: a pilot study [Abstract]. Muscle Nerve. 1994; 17:1098.9. Dinning PG, Fuentealba SE, Kennedy ML, Lubowski DZ, Cook IJ. Sacral nerve stimulation induces pancolonic propagating pressure waves and increases defecation frequency in patients with slow-transit constipation. Colorectal Dis. 2007; 9:123–32.
Article10. Govaert B, Maeda Y, Alberga J, Buntzen S, Laurberg S, Baeten CG. Medium-term outcome of sacral nerve modulation for constipation. Dis Colon Rectum. 2012; 55:26–31.
Article11. Lee KJ, Kim JH, Cho SW. Short-term effects of magnetic sacral dermatome stimulation for idiopathic slow transit constipation: sham-controlled, cross-over pilot study. J Gastroenterol Hepatol. 2006; 21(1 Pt 1):47–53.
Article12. Lin VW, Nino-Murcia M, Frost F, Wolfe V, Hsiao I, Perkash I. Functional magnetic stimulation of the colon in persons with spinal cord injury. Arch Phys Med Rehabil. 2001; 82:167–73.
Article13. Yoon YS, Kim ES, Choi JH, Jeon JH, Lee MY, Lee KJ. The effect of functional magnetic stimulation in stroke patients with chronic constipation. Gazz Med Ital. 2016; 175:421–6.14. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006; 130:1377–90.
Article15. Lim YH, Kim DH, Lee MY, Joo MC. Bowel dysfunction and colon transit time in brain-injured patients. Ann Rehabil Med. 2012; 36:371–8.
Article16. Robinson LR. Magnetic stimulation of the central and peripheral nervous systems. In : Dumitru D, Amato AA, Zwarts M, editors. Electrodiagnostic medicine. 2nd ed. Philadelphia: Henley & Belfus;2002. p. 415–27.17. Davey K, Luo L, Ross DA. Toward functional magnetic stimulation (FMS) theory and experiment. IEEE Trans Biomed Eng. 1994; 41:1024–30.
Article18. Lin VW, Hsieh C, Hsiao IN, Canfield J. Functional magnetic stimulation of expiratory muscles: a noninvasive and new method for restoring cough. J Appl Physiol (1985). 1998; 84:1144–50.
Article19. Chiu CM, Wang CP, Sung WH, Huang SF, Chiang SC, Tsai PY. Functional magnetic stimulation in constipation associated with Parkinson’s disease. J Rehabil Med. 2009; 41:1085–9.
Article20. Wang CP, Tsai PY. Efficacy of spinal magnetic stimulation in elderly persons with chronic constipation. J Chin Med Assoc. 2012; 75:127–31.
Article21. Sohn MK, Cho KH, Yoon SJ, Lee TS, Lee KJ. Effects of functional magnetic stimulation on hemiplegic shoulder subluxation. J Korean Acad Rehabil Med. 2007; 31:48–55.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bowel Dysfunction and Colon Transit Time in Brain-Injured Patients
- A Randomized, Double-blind, Active-controlled Exploratory Clinical Trial for the Evaluation of the Efficacy and Safety of Goodmorning S Granule® on Constipation
- Classification and Treatment of Constipation
- Effect of Low-Intensity Transcranial Focused Ultrasound Stimulation in Patients With Major Depressive Disorder: A Randomized, Double-Blind, Sham-Controlled Clinical Trial
- Nonpharmacologic Treatment of Chronic Constipation