J Bone Metab.
2019 Feb;26(1):45-50. 10.11005/jbm.2019.26.1.45.
Risk of Osteoporotic Fractures after Thyroid-stimulating Hormone Suppression Therapy in Patients with Thyroid Cancer
- Affiliations
-
- 1Department of Internal Medicine, Center for Thyroid Cancer, National Cancer Center, Goyang, Korea.
- 2Department of Orthopaedic Surgery, Inje University College of Medicine, Seoul Paik Hospital, Seoul, Korea.
- 3Department of Surgery, National Cancer Center, Goyang, Korea.
- 4Department of Obstetrics and Gynecology, National Cancer Center, Goyang, Korea.
- 5Department of Orthopaedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea. ykleemd@gmail.com
- KMID: 2440645
- DOI: http://doi.org/10.11005/jbm.2019.26.1.45
Abstract
- BACKGROUND
The effects of subclinical hyperthyroidism on fracture risk induced by thyroid-stimulating hormone (TSH) suppression therapy in patients with thyroid cancer still remains controversial. We performed a meta-analysis and systematic review to evaluate the effects of TSH suppression therapy on osteoporotic fracture in patients with thyroid cancer.
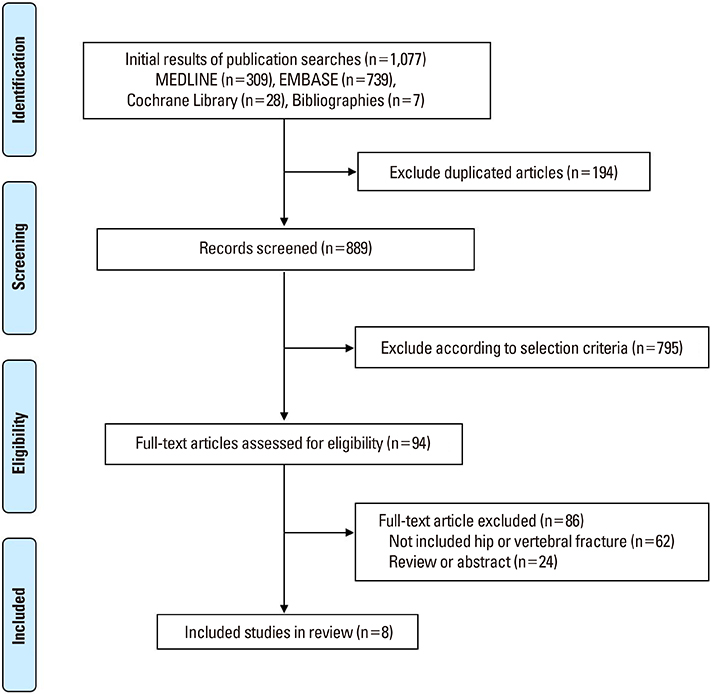
METHODS
We performed a systematic search to identify studies which included osteoporotic fractures (hip fracture and vertebral fracture) in patients on TSH suppression therapy for thyroid cancer. Main outcome measures were occurrence and risk of osteoporotic fractures including hip and vertebral fractures between patients and controls.
RESULTS
A systematic search yielded a total of 8 studies appropriate for review which included osteoporotic fracture outcome in patients on TSH suppression therapy for thyroid cancer. Studies with larger number of subjects showed the higher risk of osteoporotic fracture in group with TSH suppression therapy, although studies with smaller sample size presented a similar risk of fracture with control group.
CONCLUSIONS
Although studies were limited by small numbers, results suggested possible association between chronic TSH suppression therapy and the increased risk of osteoporotic fractures in patients with thyroid cancer.
MeSH Terms
Figure
Cited by 1 articles
-
A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang
Endocrinol Metab. 2021;36(3):574-581. doi: 10.3803/EnM.2020.943.
Reference
-
1. Williams GR, Bassett JHD. Thyroid diseases and bone health. J Endocrinol Invest. 2018; 41:99–109.
Article2. Tuchendler D, Bolanowski M. The influence of thyroid dysfunction on bone metabolism. Thyroid Res. 2014; 7:12.
Article3. Williams GR. Actions of thyroid hormones in bone. Endokrynol Pol. 2009; 60:380–388.4. Haugen BR, Alexander EK, Bible KC, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133.5. Rosario PW, Carvalho M, Calsolari MR. Symptoms of thyrotoxicosis, bone metabolism and occult atrial fibrillation in older women with mild endogenous subclinical hyperthyroidism. Clin Endocrinol (Oxf). 2016; 85:132–136.
Article6. Karunakaran P, Maharajan C, Chockalingam R, et al. The effect of total thyroidectomy on the recovery of bone mineral density in subjects with hyperthyroidism. Surgery. 2019; 165:80–84.
Article7. Abrahamsen B, Jørgensen HL, Laulund AS, et al. The excess risk of major osteoporotic fractures in hypothyroidism is driven by cumulative hyperthyroid as opposed to hypothyroid time: an observational register-based time-resolved cohort analysis. J Bone Miner Res. 2015; 30:898–905.
Article8. Gurlek A, Gedik O. Effect of endogenous subclinical hyperthyroidism on bone metabolism and bone mineral density in premenopausal women. Thyroid. 1999; 9:539–543.
Article9. Kim CW, Hong S, Oh SH, et al. Change of bone mineral density and biochemical markers of bone turnover in patients on suppressive levothyroxine therapy for differentiated thyroid carcinoma. J Bone Metab. 2015; 22:135–141.
Article10. Fujiyama K, Kiriyama T, Ito M, et al. Suppressive doses of thyroxine do not accelerate age-related bone loss in late postmenopausal women. Thyroid. 1995; 5:13–17.
Article11. Nguyen TT, Heath H 3rd, Bryant SC, et al. Fractures after thyroidectomy in men: a population-based cohort study. J Bone Miner Res. 1997; 12:1092–1099.
Article12. Melton LJ 3rd, Ardila E, Crowson CS, et al. Fractures following thyroidectomy in women: a population-based cohort study. Bone. 2000; 27:695–700.
Article13. Heijckmann AC, Huijberts MS, Geusens P, et al. Hip bone mineral density, bone turnover and risk of fracture in patients on long-term suppressive L-thyroxine therapy for differentiated thyroid carcinoma. Eur J Endocrinol. 2005; 153:23–29.
Article14. Reverter JL, Colome E, Holgado S, et al. Bone mineral density and bone fracture in male patients receiving long-term suppressive levothyroxine treatment for differentiated thyroid carcinoma. Endocrine. 2010; 37:467–472.
Article15. Mazziotti G, Formenti AM, Frara S, et al. High prevalence of radiological vertebral fractures in women on thyroid-stimulating hormone-suppressive therapy for thyroid carcinoma. J Clin Endocrinol Metab. 2018; 103:956–964.
Article16. Lin SY, Lin CL, Chen HT, et al. Risk of osteoporosis in thyroid cancer patients using levothyroxine: a population-based study. Curr Med Res Opin. 2018; 34:805–812.
Article17. Vera L, Gay S, Campomenosi C, et al. Ten-year estimated risk of bone fracture in women with differentiated thyroid cancer under TSH-suppressive levothyroxine therapy. Endokrynol Pol. 2016; 67:350–358.
Article18. McGriff NJ, Csako G, Gourgiotis L, et al. Effects of thyroid hormone suppression therapy on adverse clinical outcomes in thyroid cancer. Ann Med. 2002; 34:554–564.
Article19. Lee JS, Buzková P, Fink HA, et al. Subclinical thyroid dysfunction and incident hip fracture in older adults. Arch Intern Med. 2010; 170:1876–1883.
Article20. Heemstra KA, Hamdy NA, Romijn JA, et al. The effects of thyrotropin-suppressive therapy on bone metabolism in patients with well-differentiated thyroid carcinoma. Thyroid. 2006; 16:583–591.
Article21. Kung AW, Lorentz T, Tam SC. Thyroxine suppressive therapy decreases bone mineral density in post-menopausal women. Clin Endocrinol (Oxf). 1993; 39:535–540.
Article22. Uzzan B, Campos J, Cucherat M, et al. Effects on bone mass of long term treatment with thyroid hormones: a meta-analysis. J Clin Endocrinol Metab. 1996; 81:4278–4289.
Article23. Hofbauer LC, Kluger S, Kuhne CA, et al. Detection and characterization of RANK ligand and osteoprotegerin in the thyroid gland. J Cell Biochem. 2002; 86:642–650.
Article24. Hofbauer LC, Hamann C, Ebeling PR. Approach to the patient with secondary osteoporosis. Eur J Endocrinol. 2010; 162:1009–1020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
- TSH Suppression after Differentiated Thyroid Cancer Surgery and Osteoporosis
- Guidelines for the Postoperative Treatment of Thyroid Cancer: Levothyroxine and Calcium/Vitamin D Supplements
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
- Levothyroxine Dosing for Thyroid-Stimulating Hormone Suppression in Patients with Differentiated Thyroid Cancer after Total Thyroidectomy