Pediatr Gastroenterol Hepatol Nutr.
2019 Mar;22(2):171-180. 10.5223/pghn.2019.22.2.171.
Neurocognitive Functions in Infants with Malnutrition; Relation with Long-chain Polyunsaturated Fatty Acids, Micronutrients Levels and Magnetic Resonance Spectroscopy
- Affiliations
-
- 1Department of Pediatric Gastroenterology Hepatology and Nutrition, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey. muratcak@hotmail.com
- 2Department of Pediatrics, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey.
- 3Department of Radiology, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey.
- 4Department of Pediatric Neurology, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey.
- 5Department of Biochemistry, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey.
- KMID: 2440591
- DOI: http://doi.org/10.5223/pghn.2019.22.2.171
Abstract
- PURPOSE
Malnutrition may influence neurocognitive development in children by directly affecting the brain structural development, or indirectly by affecting the children's cognition experience. Malnutrition alters the cell numbers, cell migration, synaptogenesis, and neurotransmission due to inadequate availability of necessary micronutrients to support cell growth. We aimed to analyze neurocognitive development in infants with malnutrition and its association with long chain polyunsaturated fatty acids (LC-PUFA), micronutrients levels and magnetic resonance spectroscopy (MRS) findings.
METHODS
The study included two groups; group 1, infants with malnutrition (n=24), group 2; healthy infants (n=21). Peripheral blood was obtained from the participants for studying micronutrients and LC-PUFA levels. The neurocognitive development was analyzed by the use of an Ankara Developmental Screening Inventory test. MRS were performed on all infants.
RESULTS
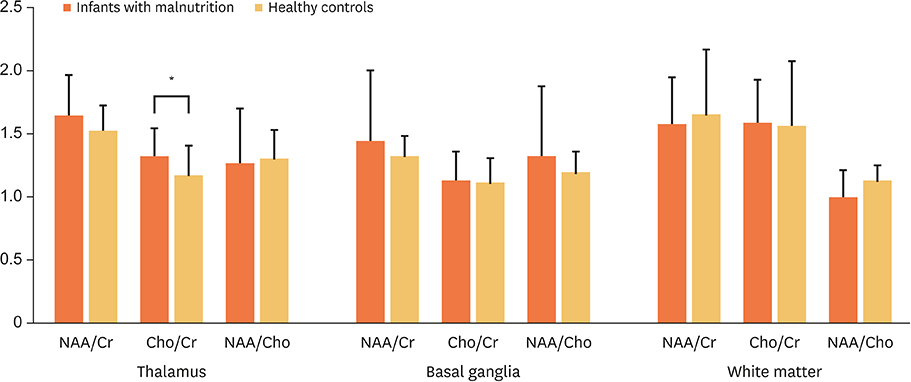
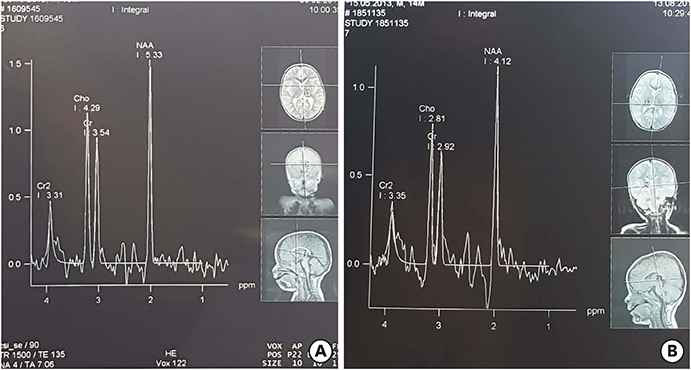
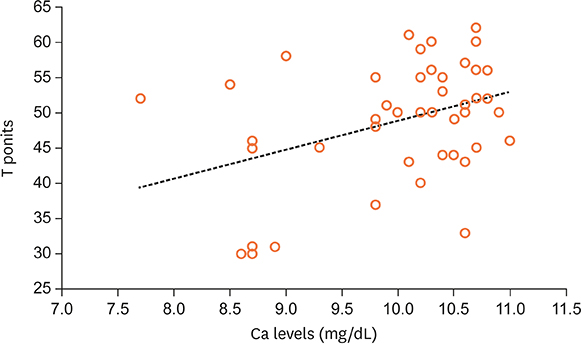
All parameters of neurocognitive development and serum calcium (9.6±0.9 mg/dL vs. 10.4±0.3 mg/dL, p < 0.05) and magnesium (2.02±0.27 mg/dL vs. 2.2±0.14 mg/dL, p < 0.05) levels were noted as being low in infants with marked malnutrition. No difference was found in LC-PUFA levels between healthy and malnourished infants. Thalamic choline/creatine levels were significantly high in infants with malnutrition (1.33±0.22 vs. 1.18±0.22, p < 0.05). Total neurocognitive development in infants was positively correlated with serum calcium levels (p < 0.05, r=0.381).
CONCLUSION
Calcium supplementation may improve neurocognitive development in malnourished infants.
MeSH Terms
Figure
Cited by 1 articles
-
Physicians' Understanding of Nutritional Factors Determining Brain Development and Cognition in the Middle East and Africa
Yvan Vandenplas, Aditya Rakhecha, Amira Edris, Bassel Shaaban, Eslam Tawfik, Fahad A. Bashiri, Fahd AlAql, Hassan Alsabea, Joseph Haddad, Mohammed El Barbary, Mohamed Salah, Mohamed Abouelyazid, Mudit Kumar, Sulaiman Alsaad
Pediatr Gastroenterol Hepatol Nutr. 2019;22(6):536-544. doi: 10.5223/pghn.2019.22.6.536.
Reference
-
1. Agostoni C, Manzoni P. Nutrition and neurocognitive development. Early Hum Dev. 2013; 89:Suppl 1. S1–S3.
Article2. Prado EL, Dewey KG. Nutrition and brain development in early life. Nutr Rev. 2014; 72:267–284.
Article3. Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. International Child Development Steering Group. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007; 369:60–70.
Article4. Black MM. Micronutrient deficiencies and cognitive functioning. J Nutr. 2003; 133:3927S–31S.
Article5. Uauy R, Dangour AD. Nutrition in brain development and aging: role of essential fatty acids. Nutr Rev. 2006; 64:S24–33.
Article6. Ulmer S, Backens M, Ahlhelm FJ. Basic principles and clinical applications of magnetic resonance spectroscopy in neuroradiology. J Comput Assist Tomogr. 2016; 40:1–13.
Article7. World Health Organization. Severe acute malnutrition [Internet]. Geneva: World Health Organization;2009. cited 2017 Dec 10. Available from: http://www.who.int/nutrition/topics/malnutrition/en/.8. Erol N, Sezgin N, Savasir I. Validity studies for development-screening inventory. Turk J Psychol. 1993; 8:16–22.9. Savasir I, Sezgin N, Erol N. Handbook of Ankara development-screening inventory. 2nd ed. Ankara: Rekmay;1998.10. Hamaguchi H, Cleve H. Solubilization of human erythrocyte membrane glycoproteins and separation of the MN glycoprotein from a glycoprotein with I, S, and A activity. Biochim Biophys Acta. 1972; 278:271–280.
Article11. Sattler W, Puhl H, Hayn M, Kostner GM, Esterbauer H. Determination of fatty acids in the main lipoprotein classes by capillary gas chromatography: BF3/methanol transesterification of lyophilized samples instead of Folch extraction gives higher yields. Anal Biochem. 1991; 198:184–190.
Article12. Granados-Rojas L, Serrano N, Gutiérrez-Ospina G, Díaz-Cintra S. Prenatal protein malnutrition differentially affects the volume of the granule layer and mossy fibers in young male and female rats. Proc West Pharmacol Soc. 2002; 45:53–54.13. Mathangi DC, Namasivayam A. Effect of chronic protein restriction on motor co-ordination and brain neurotransmitters in albino rats. Food Chem Toxicol. 2001; 39:1039–1043.
Article14. Alamy M, Bengelloun WA. Malnutrition and brain development: an analysis of the effects of inadequate diet during different stages of life in rat. Neurosci Biobehav Rev. 2012; 36:1463–1480.
Article15. Benítez-Bribiesca L, De la Rosa-Alvarez I, Mansilla-Olivares A. Dendritic spine pathology in infants with severe protein-calorie malnutrition. Pediatrics. 1999; 104:e21.
Article16. Nyaradi A, Li J, Hickling S, Foster J, Oddy WH. The role of nutrition in children's neurocognitive development, from pregnancy through childhood. Front Hum Neurosci. 2013; 7:97.
Article17. Engle PL, Fernández PD. INCAP studies of malnutrition and cognitive behavior. Food Nutr Bull. 2010; 31:83–94.
Article18. Isik Y, Kalyoncu M, Okten A. Serum leptin levels in marasmic children and the relationship between leptin and lipid profile. Ann Nutr Metab. 2004; 48:259–262.
Article19. Akuyam A, Isah HS, Ogala WN. Serum lipid profile in malnourished Nigerian children in Zaria. Niger Postgrad Med J. 2008; 15:192–196.20. Fageer SA, Karar TA, Hag SM. Assessment of plasma levels of proteins, total cholesterol and high density. J Sci Technol. 2013; 14:35–43.21. Veiga GR, Ferreira HS, Sawaya AL, Calado J, Florêncio TM. Dyslipidaemia and undernutrition in children from impoverished areas of Maceió, state of Alagoas, Brazil. Int J Environ Res Public Health. 2010; 7:4139–4151.
Article22. Chisti MJ, Salam MA, Ashraf H, Faruque AS, Bardhan PK, Shahid AS, et al. Prevalence, clinical predictors, and outcome of hypocalcaemia in severely-malnourished under-five children admitted to an urban hospital in Bangladesh: a case-control study. J Health Popul Nutr. 2014; 32:270–275.23. Singla PN, Chand P, Kumar A, Kachhawaha JS. Serum magnesium levels in protein-energy malnutrition. J Trop Pediatr. 1998; 44:117–119.24. El-khayat H, Shaaban S, Emam EK, Elwakkad A. Cognitive functions in protein-energy malnutrition: in relation to long chain-polyunsaturated fatty acids. Pak J Biol Sci. 2007; 10:1773–1781.
Article25. Gil A, Ramirez M, Gil M. Role of long-chain polyunsaturated fatty acids in infant nutrition. Eur J Clin Nutr. 2003; 57:Suppl 1. S31–S34.
Article26. Schulzke SM, Patole SK, Simmer K. Long-chain polyunsaturated fatty acid supplementation in preterm infants. Cochrane Database Syst Rev. 2011; CD000375.
Article27. Smithers LG, Gibson RA, Makrides M. Maternal supplementation with docosahexaenoic acid during pregnancy does not affect early visual development in the infant: a randomized controlled trial. Am J Clin Nutr. 2011; 93:1293–1299.
Article28. McCann JC, Ames BN. Is docosahexaenoic acid, an n-3 long-chain polyunsaturated fatty acid, required for development of normal brain function? An overview of evidence from cognitive and behavioral tests in humans and animals. Am J Clin Nutr. 2005; 82:281–295.
Article29. Simmer K, Patole SK, Rao SC. Long-chain polyunsaturated fatty acid supplementation in infants born at term. Cochrane Database Syst Rev. 2008; CD000376.
Article30. Kendall GS, Melbourne A, Johnson S, Price D, Bainbridge A, Gunny R, et al. White matter NAA/Cho and Cho/Cr ratios at MR spectroscopy are predictive of motor outcome in preterm infants. Radiology. 2014; 271:230–238.
Article31. Guo L, Wang D, Bo G, Zhang H, Tao W, Shi Y. Early identification of hypoxic-ischemic encephalopathy by combination of magnetic resonance (MR) imaging and proton MR spectroscopy. Exp Ther Med. 2016; 12:2835–2842.
Article32. Nassar M, Shaaban S, Abbas Y, Galal A, Naguib A, Kamal El-Deen A. Proton Magnetic Resonance Spectroscopy in protein energy malnutrition patients. J Pediatr Gastroenterol Nutr. 2011; 52:Suppl 1. e63.33. Filippi CG, Uluğ AM, Deck MD, Zimmerman RD, Heier LA. Developmental delay in children: assessment with proton MR spectroscopy. AJNR Am J Neuroradiol. 2002; 23:882–888.34. Hart PH, Lucas RM, Walsh JP, Zosky GR, Whitehouse AJ, Zhu K, et al. Vitamin D in fetal development: findings from a birth cohort study. Pediatrics. 2015; 135:e167–73.
Article35. Schlögl M, Holick MF. Vitamin D and neurocognitive function. Clin Interv Aging. 2014; 9:559–568.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Trials for Preterm Infants' Neurodevelopment to the Norm: Erythropoietin and Nutritional Interventions
- Polyunsaturated Fatty Acids in Children
- Gut Microbiota-Derived Short-Chain Fatty Acids, T Cells, and Inflammation
- Analysis of Plasma Long-Chain Fatty Acids in Hypertensive Patients
- Nutrition Support in Liver Transplantation Patients