Ann Surg Treat Res.
2019 Feb;96(2):78-85. 10.4174/astr.2019.96.2.78.
Does total regression of primary rectal cancer after preoperative chemoradiotherapy represent “no tumor†status?
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Colon and Rectal Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ipark@amc.seoul.kr
- 3Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2433944
- DOI: http://doi.org/10.4174/astr.2019.96.2.78
Abstract
- PURPOSE
Insistence that total regression of primary tumor would not represent long-term oncologic outcomes has been raised. Therefore, this study aimed to evaluate the outcomes of these patients after preoperative chemoradiotherapy (PCRT) and radical surgery and to evaluate the associated risk factors.
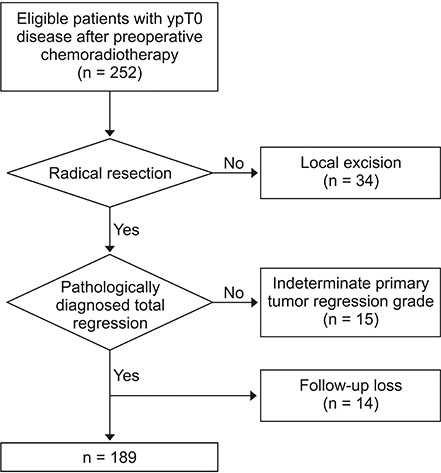
METHODS
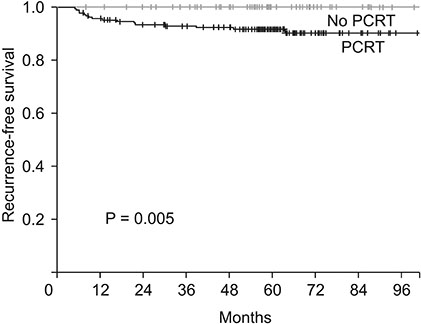
We included 189 patients with rectal cancer who showed total regression of the primary tumor after PCRT, followed by radical resection, between 2001 and 2012. Recurrence-free survival (RFS) was calculated using the Kaplan-Meier method, and the results were compared with 77 patients with Tis rectal cancer who received only radical resection. Factors associated with RFS were evaluated using Cox regression analysis.
RESULTS
Sphincter-saving resection was performed for 146 patients (77.2%). Adjuvant chemotherapy was administered to 168 patients (88.9%). During the follow-up period, recurrence occurred in 17 patients (9%). The 5-year RFS was 91.3%, which was significantly lower than that of patients with Tis rectal cancer without PCRT (P = 0.005). In univariate analysis, preoperative CEA and histologic differentiation were associated with RFS. However, no factors were found to be associated with RFS.
CONCLUSION
RFS was lower in patients with total regression of primary rectal cancer after PCRT than in those with Tis rectal cancer without PCRT, and it would not be considered as the same entity with early rectal cancer or "disappeared tumor" status.
MeSH Terms
Figure
Reference
-
1. Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004; 351:1731–1740.
Article2. Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012; 30:1926–1933.
Article3. Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U Jr, Silva e Sousa AH Jr, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg. 2004; 240:711–717.4. Garcia-Aguilar J, Renfro LA, Chow OS, Shi Q, Carrero XW, Lynn PB, et al. Organ preservation for clinical T2N0 distal rectal cancer using neoadjuvant chemoradiotherapy and local excision (ACOSOG Z6041): results of an open-label, singlearm, multi-institutional, phase 2 trial. Lancet Oncol. 2015; 16:1537–1546.
Article5. Perez RO, Habr-Gama A, Lynn PB, Sao Juliao GP, Bianchi R, Proscurshim I, et al. Transanal endoscopic microsurgery for residual rectal cancer (ypT0-2) following neoadjuvant chemoradiation therapy: another word of caution. Dis Colon Rectum. 2013; 56:6–13.6. Stipa F, Picchio M, Burza A, Soricelli E, Vitelli CE. Long-term outcome of local excision after preoperative chemoradiation for ypT0 rectal cancer. Dis Colon Rectum. 2014; 57:1245–1252.
Article7. Lee SD, Park SC, Park JW, Kim DY, Choi HS, Oh JH. Laparoscopic versus open surgery for stage I rectal cancer: long-term oncologic outcomes. World J Surg. 2013; 37:646–651.
Article8. Fokas E, Strobel P, Fietkau R, Ghadimi M, Liersch T, Grabenbauer GG, et al. Tumor regression grading after preoperative chemoradiotherapy as a prognostic factor and individual-level surrogate for disease-free survival in rectal cancer. J Natl Cancer Inst. 2017; 109.
Article9. Park IJ, You YN, Agarwal A, Skibber JM, Rodriguez-Bigas MA, Eng C, et al. Neoadjuvant treatment response as an early response indicator for patients with rectal cancer. J Clin Oncol. 2012; 30:1770–1776.
Article10. Fokas E, Liersch T, Fietkau R, Hohenberger W, Beissbarth T, Hess C, et al. Tumor regression grading after preoperative chemoradiotherapy for locally advanced rectal carcinoma revisited: updated results of the CAO/ARO/AIO-94 trial. J Clin Oncol. 2014; 32:1554–1562.
Article11. Althumairi AA, Gearhart SL. Local excision for early rectal cancer: transanal endoscopic microsurgery and beyond. J Gastrointest Oncol. 2015; 6:296–306.12. Chang HJ, Park CK, Kim WH, Kim YB, Kim YW, Kim HG, et al. A standardized pathology report for colorectal cancer. Korean J Pathol. 2006; 40:193–203.13. Huh JW, Kim CH, Kim HR, Kim YJ. Oncologic outcomes of pathologic stage I lower rectal cancer with or without preoperative chemoradiotherapy: are they comparable? Surgery. 2011; 150:980–984.
Article14. Hwang K, Park IJ, Yu CS, Lim SB, Lee JL, Yoon YS, et al. Impression of prognosis regarding pathologic stage after preoperative chemoradiotherapy in rectal cancer. World J Gastroenterol. 2015; 21:563–570.
Article15. Stitzenberg KB, Sanoff HK, Penn DC, Meyers MO, Tepper JE. Practice patterns and long-term survival for early-stage rectal cancer. J Clin Oncol. 2013; 31:4276–4282.
Article16. Allaix ME, Arezzo A, Morino M. Transanal endoscopic microsurgery for rectal cancer: T1 and beyond? An evidence-based review. Surg Endosc. 2016; 30:4841–4852.
Article17. Jung SM, Yu CS, Park IJ, Kim TW, Kim JH, Yoon YS, et al. Oncologic safety of local excision compared with total mesorectal excision for ypT0-T1 rectal cancer: a propensity score analysis. Medicine (Baltimore). 2016; 95:e3718.18. Roh MS, Colangelo LH, O'Connell MJ, Yothers G, Deutsch M, Allegra CJ, et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol. 2009; 27:5124–5130.
Article19. Rodel C, Martus P, Papadoupolos T, Fuzesi L, Klimpfinger M, Fietkau R, et al. Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol. 2005; 23:8688–8696.20. Maas M, Nelemans PJ, Valentini V, Das P, Rodel C, Kuo LJ, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol. 2010; 11:835–844.
Article21. Noh JM, Park W, Kim JS, Koom WS, Kim JH, Choi DH, et al. Outcome of local excision following preoperative chemoradiotherapy for clinically T2 distal rectal cancer: a multicenter retrospective study (KROG 12-06). Cancer Res Treat. 2014; 46:243–249.
Article22. Yeo SG, Kim DY, Park JW, Choi HS, Oh JH, Kim SY, et al. Stage-to-stage comparison of preoperative and postoperative chemoradiotherapy for T3 mid or distal rectal cancer. Int J Radiat Oncol Biol Phys. 2012; 82:856–862.
Article23. Gollins S, Sun Myint A, Haylock B, Wise M, Saunders M, Neupane R, et al. Preoperative chemoradiotherapy using concurrent capecitabine and irinotecan in magnetic resonance imaging-defined locally advanced rectal cancer: impact on long-term clinical outcomes. J Clin Oncol. 2011; 29:1042–1049.
Article24. Park IJ, You YN, Skibber JM, Rodriguez-Bigas MA, Feig B, Nguyen S, et al. Comparative analysis of lymph node metastases in patients with ypT0-2 rectal cancers after neoadjuvant chemoradiotherapy. Dis Colon Rectum. 2013; 56:135–141.
Article25. Dinaux AM, Leijssen L, Bordeianou LG, Kunitake H, Amri R, Berger DL. Outcomes of persistent lymph node involvement after neoadjuvant therapy for stage III rectal cancer. Surgery. 2018; 163:784–788.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy
- Impairment of Immunonutritional Status During Treatment is a Factor Associated With Oncologic Outcomes in Patients With Rectal Cancer Treated With Preoperative Chemoradiotherapy
- Prognostic Significance of Tumor Regression Grade after Preoperative Chemoradiotherapy for Rectal Cancer
- Preoperative Concurrent Chemoradiotherapy with Oral Fluoropyrimidine in Locally Advanced Rectal Cancer: How Good Is Good Enough?
- An Update on Preoperative Radiotherapy for Locally Advanced Rectal Cancer