Ann Surg Treat Res.
2019 Feb;96(2):70-77. 10.4174/astr.2019.96.2.70.
Different prognostic values of individual hematologic parameters in papillary thyroid cancer due to age-related changes in immunity
- Affiliations
-
- 1Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. subi0117@naver.com
- KMID: 2433943
- DOI: http://doi.org/10.4174/astr.2019.96.2.70
Abstract
- PURPOSE
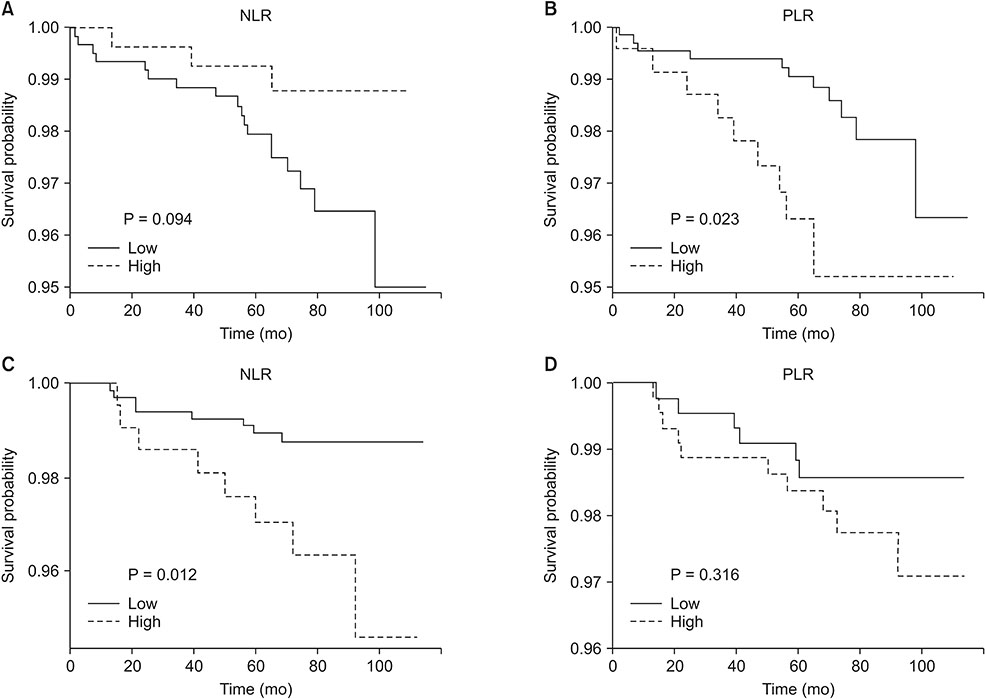
Several studies have reported the plausible association of neutrophil-to-lymphocyte ratio (NLR) with the prognosis of papillary thyroid cancer (PTC), but the results are inconsistent. In PTC, chronic inflammation is closely related to tumor progression, and the age of the patient has a great influence on prognosis. Therefore, considering the changes in the immune system with aging, we classified the patients according to age and assessed the prognostic value of individual hematologic parameters.
METHODS
This retrospective analysis included 1,921 patients who underwent thyroidectomy for PTC. Patients were divided into 2 groups based on their age: Y-group (age < 45) and O-group (age ≥ 45). Blood counts were measured within 14 days before surgery.
RESULTS
The Y-group consisted of 914 patients aged < 45 years and the O-group consisted of 932 patients aged ≥ 45. In both groups, the common prognostic factors related to disease recurrence were only 6 or more metastatic lymph node and grossly extrathyroidal extension, and hematologic parameters were different between the 2 groups. High Platelet-lymphocyte ratio (PLR) in the Y-group and high NLR in the O-group were identified as independent predictors of disease recurrence (NLR: hazard ratio [HR], 3.28; 95% confidence interval [CI], 1.23-8.73; P = 0.018; PLR: HR, 3.08; 95% CI, 1.26-7.52; P = 0.014).
CONCLUSION
The results suggest that changes in immunity with aging may affect prognosis in patients with PTC, and thus hematologic parameters might be employed as prognostic markers depending on the age of the patients.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Mechanisms of the Impact of Hashimoto Thyroiditis on Papillary Thyroid Carcinoma Progression: Relationship with the Tumor Immune Microenvironment
Oksana Sulaieva, Olena Chernenko, Oleksiy Selesnov, Oleksandr Nechay, Oleksandr Maievskyi, Tetyana Falalyeyeva, Nazarii Kobyliak, Olena Tsyryuk, Yurii Penchuk, Dmytro Shapochka
Endocrinol Metab. 2020;35(2):443-455. doi: 10.3803/EnM.2020.35.2.443.Unmet Clinical Needs in the Treatment of Patients with Thyroid Cancer
Won Bae Kim, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong
Endocrinol Metab. 2020;35(1):14-25. doi: 10.3803/EnM.2020.35.1.14.
Reference
-
1. Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol. 2005; 91:181–184.
Article2. Iyengar NM, Hudis CA, Dannenberg AJ. Obesity and inflammation: new insights into breast cancer development and progression. Am Soc Clin Oncol Educ Book. 2013; 46–51.
Article3. Moore MM, Chua W, Charles KA, Clarke SJ. Inflammation and cancer: causes and consequences. Clin Pharmacol Ther. 2010; 87:504–508.
Article4. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002; 420:860–867.
Article5. Seretis C, Gourgiotis S, Gemenetzis G, Seretis F, Lagoudianakis E, Dimitrakopoulos G. The significance of neutrophil/lymphocyte ratio as a possible marker of underlying papillary microcarcinomas in thyroidal goiters: a pilot study. Am J Surg. 2013; 205:691–696.
Article6. Proctor MJ, McMillan DC, Morrison DS, Fletcher CD, Horgan PG, Clarke SJ. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer. 2012; 107:695–699.
Article7. Liu CL, Lee JJ, Liu TP, Chang YC, Hsu YC, Cheng SP. Blood neutrophil-to-lymphocyte ratio correlates with tumor size in patients with differentiated thyroid cancer. J Surg Oncol. 2013; 107:493–497.
Article8. Liu J, Du J, Fan J, Liu K, Zhang B, Wang S, et al. The neutrophil-to-lymphocyte ratio correlates with age in patients with papillary thyroid carcinoma. ORL J Otorhinolaryngol Relat Spec. 2015; 77:109–116.
Article9. Kim JY, Park T, Jeong SH, Jeong CY, Ju YT, Lee YJ, et al. Prognostic importance of baseline neutrophil to lymphocyte ratio in patients with advanced papillary thyroid carcinomas. Endocrine. 2014; 46:526–531.
Article10. Lang BH, Ng CP, Au KB, Wong KP, Wong KK, Wan KY. Does preoperative neutrophil lymphocyte ratio predict risk of recurrence and occult central nodal metastasis in papillary thyroid carcinoma? World J Surg. 2014; 38:2605–2612.
Article11. Cho JS, Park MH, Ryu YJ, Yoon JH. The neutrophil to lymphocyte ratio can discriminate anaplastic thyroid cancer against poorly or well differentiated cancer. Ann Surg Treat Res. 2015; 88:187–192.
Article12. Manatakis DK, Tseleni-Balafouta S, Balalis D, Soulou VN, Korkolis DP, Sakorafas GH, et al. Association of baseline neutrophil-to-lymphocyte ratio with clinicopathological characteristics of papillary thyroid carcinoma. Int J Endocrinol. 2017; 2017:8471235.
Article13. Ozmen S, Timur O, Calik I, Altinkaynak K, Simsek E, Gozcu H, et al. Neutrophil-lymphocyte ratio (NLR) and platelet-lymphocyte ratio (PLR) may be superior to C-reactive protein (CRP) for predicting the occurrence of differentiated thyroid cancer. Endocr Regul. 2017; 51:131–136.
Article14. Kim SM, Kim EH, Kim BH, Kim JH, Park SB, Nam YJ, et al. Association of the preoperative neutrophil-to-ymphocyte count ratio and platelet-to-lymphocyte count ratio with clinicopathological characteristics in patients with papillary thyroid cancer. Endocrinol Metab (Seoul). 2015; 30:494–501.
Article15. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474.
Article16. Haymart MR. Understanding the relationship between age and thyroid cancer. Oncologist. 2009; 14:216–221.
Article17. Youden WJ. Index for rating diagnostic tests. Cancer. 1950; 3:32–35.
Article18. R Core Team. R: A language and environment for statistical computing [Internet]. Vienna: R Foundation for Statistical Computing;c2016. cited 2018 Feb 20. Available from: https://www.R-project.org/.19. Therneau T. A package for survival analysis in S. version 2.38 [Internet]. Vienna: R Foundation for Statistical Computing;c2015. cited 2018 Feb 20. Available from: https://CRAN.R-project.org/package=survival.20. Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. New York: Springer;2000.21. Linos D. Minimally invasive thyroidectomy: a comprehensive appraisal of existing techniques. Surgery. 2011; 150:17–24.
Article22. Kim EY, Lee KH, Park YL, Park CH, Lee CR, Jeong JJ, et al. Single-incision, gasless, endoscopic trans-axillary total thyroidectomy: a feasible and oncologic safe surgery in patients with papillary thyroid carcinoma. J Laparoendosc Adv Surg Tech A. 2017; 27:1158–1164.
Article23. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133.24. Yaylaci S, Tosun O, Sahin O, Genc AB, Aydin E, Demiral G, et al. Lack of variation in inflammatory hematological parameters between benign nodular goiter and papillary thyroid cancer. Asian Pac J Cancer Prev. 2016; 17:2321–2323.
Article25. Franceschi C, Bonafe M, Valensin S, Olivieri F, De Luca M, Ottaviani E, et al. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci. 2000; 908:244–254.
Article26. Xia S, Zhang X, Zheng S, Khanabdali R, Kalionis B, Wu J, et al. An update on inflamm-aging: mechanisms, prevention, and treatment. J Immunol Res. 2016; 2016:8426874.
Article27. Salminen A, Huuskonen J, Ojala J, Kauppinen A, Kaarniranta K, Suuronen T. Activation of innate immunity system during aging: NF-kB signaling is the molecular culprit of inflamm-aging. Ageing Res Rev. 2008; 7:83–105.
Article28. Pes GM, Lio D, Carru C, Deiana L, Baggio G, Franceschi C, et al. Association between longevity and cytokine gene polymorphisms. A study in Sardinian centenarians. Aging Clin Exp Res. 2004; 16:244–248.
Article29. Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer. 2014; 110:2524–2530.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Closer Look at Papillary Thyroid Carcinoma
- Significance of Lymphovascular Invasion as a Prognostic Factor in Patients with Papillary Thyroid Cancer: a Systematic Review and Meta-Analysis
- The Clinical Significance of Preoperative Serum Neutrophil-Lymphocyte Ratio (NLR) in Papillary Thyroid Cancer Patients
- The Clinical Significance of Expression of Cyclooxygenase-2 in the Prognosis of the Papillary Thyroid Cancer
- Expression of Cyclooxygenase-2 in Well Differentiated Thyroid Carcinoma