J Korean Assoc Oral Maxillofac Surg.
2018 Oct;44(5):212-219. 10.5125/jkaoms.2018.44.5.212.
Subcutaneous emphysema related to dental procedures
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Gangnam Severance Hospital, Yonsei University College of Dentistry, Seoul, Korea. omshuh@yuhs.ac
- 2Department of Dentistry, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
- KMID: 2430581
- DOI: http://doi.org/10.5125/jkaoms.2018.44.5.212
Abstract
OBJECTIVES
The objective of this study was to analyze 11 cases of subcutaneous emphysema associated with dental procedures from a single hospital and discuss approaches for accurate diagnosis and treatment of the condition.
MATERIALS AND METHODS
The medical records of 11 patients who were treated for subcutaneous emphysema related to dental procedures between January 2009 and April 2017 were analyzed retrospectively. Patients with subcutaneous emphysema within the facial area or that spread to the neck and beyond, including the facial region, were assigned to two groups and compared in terms of age, sex, and durations of antibiotic use, hospitalization, and follow-up until improvement. The correlation between location of the origin tooth and range of emphysema spread was analyzed.
RESULTS
The average durations of antibiotic use during conservative treatment and follow-up until improvement were 8.55 days (standard deviation [SD], 4.46 days) and 1.82 weeks (SD, 1.19 weeks), respectively. There was no intergroup difference in duration of antibiotic use (P=0.329) or follow-up (P=0.931). Subcutaneous emphysema was more common after dental procedures involving the maxilla or posterior region than after those involving the mandible or anterior region. There was no significant difference in air distribution according to location of the air orifice (maxilla, mandible, or both; P=0.106).
CONCLUSION
Upon adequate conservative treatment accompanied by prophylactic antibiotic treatment considering the risk of infection, patients showed signs of improvement within a few days or weeks. There was no significant difference in treatment period between patients with subcutaneous emphysema localized to the facial region and those with subcutaneous emphysema spreading to the neck or beyond. These findings need to be confirmed by analysis of additional cases.
Keyword
MeSH Terms
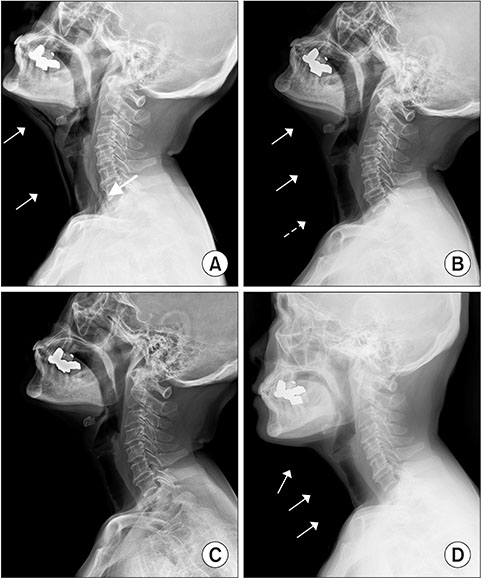
Figure
Reference
-
1. Neville BW, Damm DD, Allen CM, Chi AC. Oral and maxillofacial pathology. 4th ed. St. Louis, MO: Elsevier Health Sciences;2015.2. Mather AJ, Stoykewych AA, Curran JB. Cervicofacial and mediastinal emphysema complicating a dental procedure. J Can Dent Assoc. 2006; 72:565–568.3. Cardo VA Jr, Mooney JW, Stratigos GT. Iatrogenic dental-air emphysema: report of case. J Am Dent Assoc. 1972; 85:144–147.
Article4. Horowitz I, Hirshberg A, Freedman A. Pneumomediastinum and subcutaneous emphysema following surgical extraction of mandibular third molars: three case reports. Oral Surg Oral Med Oral Pathol. 1987; 63:25–28.
Article5. Shackelford D, Casani JA. Diffuse subcutaneous emphysema, pneumomediastinum, and pneumothorax after dental extraction. Ann Emerg Med. 1993; 22:248–250.
Article6. Reznick JB, Ardary WC. Cervicofacial subcutaneous air emphysema after dental extraction. J Am Dent Assoc. 1990; 120:417–419.
Article7. Chen SC, Lin FY, Chang KJ. Subcutaneous emphysema and pneumomediastinum after dental extraction. Am J Emerg Med. 1999; 17:678–680.
Article8. Frühauf J, Weinke R, Pilger U, Kerl H, Müllegger RR. Soft tissue cervicofacial emphysema after dental treatment: report of 2 cases with emphasis on the differential diagnosis of angioedema. Arch Dermatol. 2005; 141:1437–1440.
Article9. Yang SC, Chiu TH, Lin TJ, Chan HM. Subcutaneous emphysema and pneumomediastinum secondary to dental extraction: a case report and literature review. Kaohsiung J Med Sci. 2006; 22:641–645.
Article10. Kung JC, Chuang FH, Hsu KJ, Shih YL, Chen CM, Huang IY. Extensive subcutaneous emphysema after extraction of a mandibular third molar: a case report. Kaohsiung J Med Sci. 2009; 25:562–566.
Article11. Nahlieli O, Neder A. Iatrogenic pneumomediastinum after endodontic therapy. Oral Surg Oral Med Oral Pathol. 1991; 71:618–619.
Article12. Feinstone T. Infected subcutaneous emphysema: report of case. J Am Dent Assoc. 1971; 83:1309–1311.
Article13. McKenzie WS, Rosenberg M. Iatrogenic subcutaneous emphysema of dental and surgical origin: a literature review. J Oral Maxillofac Surg. 2009; 67:1265–1268.
Article14. Peterson LJ. Emphysema and the dental drill [Comment]. J Am Dent Assoc. 1990; 120:423.15. Demas PN, Braun TW. Infection associated with orbital subcutaneous emphysema. J Oral Maxillofac Surg. 1991; 49:1239–1242.
Article16. Rickles NH, Joshi BA. Death from air embolism during root canal therapy. J Am Dent Assoc. 1963; 67:397–404.
Article17. Pynn BR, Amato D, Walker DA. Subcutaneous emphysema following dental treatment: a report of two cases and review of the literature. J Can Dent Assoc. 1992; 58:496–499.18. Patel N, Lazow SK, Berger J. Cervicofacial subcutaneous emphysema: case report and review of literature. J Oral Maxillofac Surg. 2010; 68:1976–1982.
Article19. Hounsfield GN. Nobel award address. Computed medical imaging. Med Phys. 1980; 7:283–290.20. Karras SC, Sexton JJ. Cervicofacial and mediastinal emphysema as the result of a dental procedure. J Emerg Med. 1996; 14:9–13.
Article21. Greenberg RN, James RB, Marier RL, Wood WH, Sanders CV, Kent JN. Microbiologic and antibiotic aspects of infections in the oral and maxillofacial region. J Oral Surg. 1979; 37:873–884.22. Aragon SB, Dolwick MF, Buckley S. Pneumomediastinum and subcutaneous cervical emphysema during third molar extraction under general anesthesia. J Oral Maxillofac Surg. 1986; 44:141–144.
Article23. Oliver AJ, Diaz EM Jr, Helfrick JF. Air emphysema secondary to mandibular fracture: case report. J Oral Maxillofac Surg. 1993; 51:1143–1145.
Article24. Lee HY, Samit A, Mashberg A. Extensive post-traumatic subcutaneous emphysema and pneumomediastinum following a minor facial injury. J Oral Maxillofac Surg. 1987; 45:812–815.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pneumomediastinum and Subcutaneous Emphysema after Use of a High-Speed Dental Handpiece
- Subcutaneous emphysema and pneumomediastinum during dental treatment
- Extensive Bilateral Subcutaneous Emphysema after Dental Treatment: Two Case Reports
- A Facial Subcutaneous Emphysema after Using a Fish Cake Skewer: Case Report
- Emphysema following air-powder abrasive treatment for peri-implantitis