J Korean Soc Spine Surg.
2018 Dec;25(4):169-174. 10.4184/jkss.2018.25.4.169.
A Thoracolumbar Pure Spinal Epidural Cavernous Hemangioma: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Inje University Haeundae Paik Hospital, Busan, Korea. potata98@naver.com
- 2Department of Pathology, Inje University Haeundae Paik Hospital, Busan, Korea.
- KMID: 2430142
- DOI: http://doi.org/10.4184/jkss.2018.25.4.169
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
We report a case of pure epidural cavernous hemangioma located at the thoracolumbar spine in a 53-year-old woman that mimicked a neurogenic tumor on magnetic resonance imaging (MRI). SUMMARY OF LITERATURE REVIEW: A pure spinal epidural cavernous hemangioma without bony involvement is a very rare lesion about which limited information is available in the literature.
MATERIALS AND METHODS
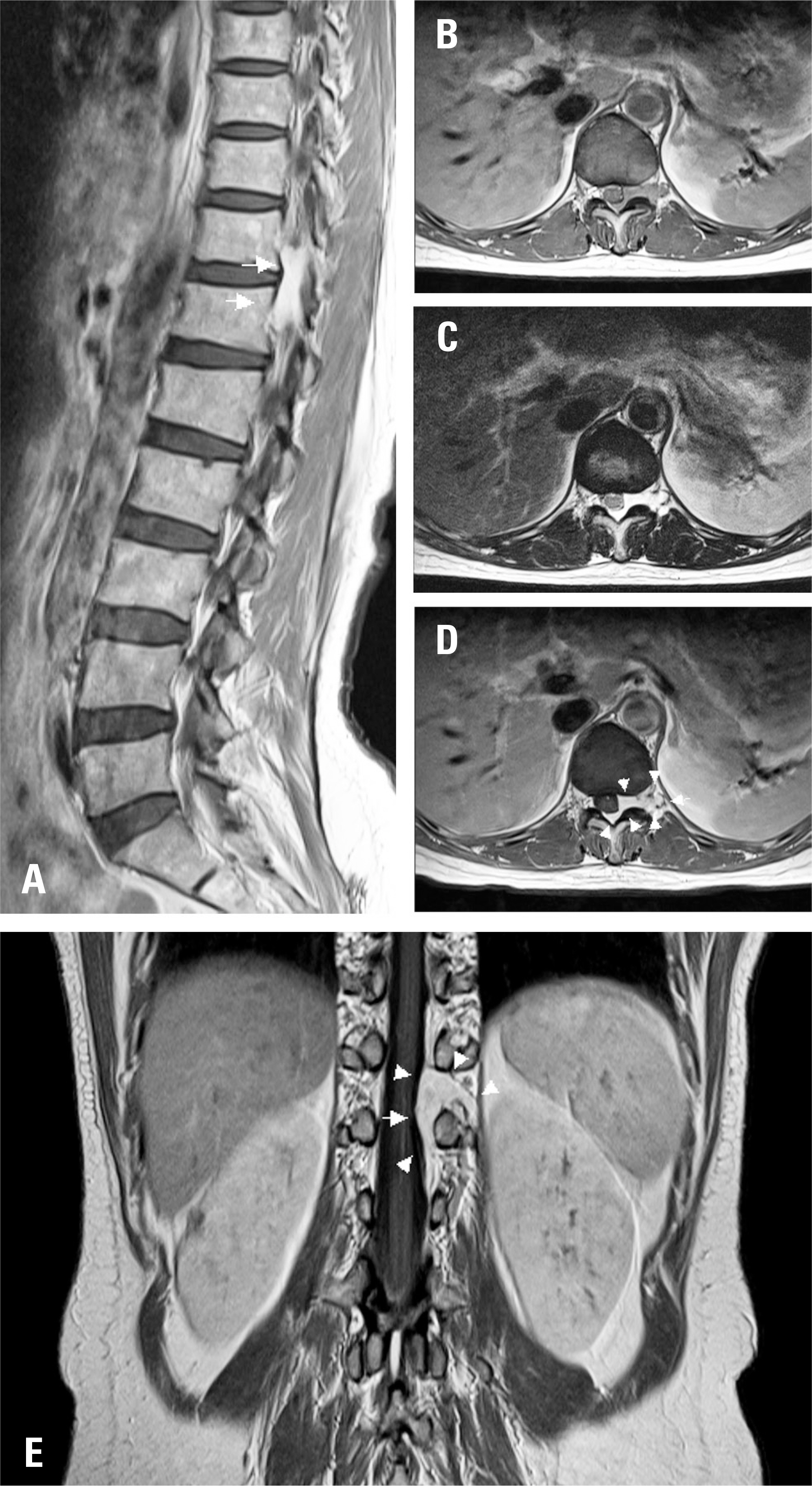
A 53-year-old woman visited our clinic for hypoesthesia with a tingling sensation in the left anterolateral thigh that had begun a month ago. No other neurologic symptoms or signs were present upon a neurologic examination. MRI from an outside hospital showed a 2.0×0.5 cm elongated mass at the T11-12 left neural foramen. The tumor was completely removed in piecemeal fashion.
RESULTS
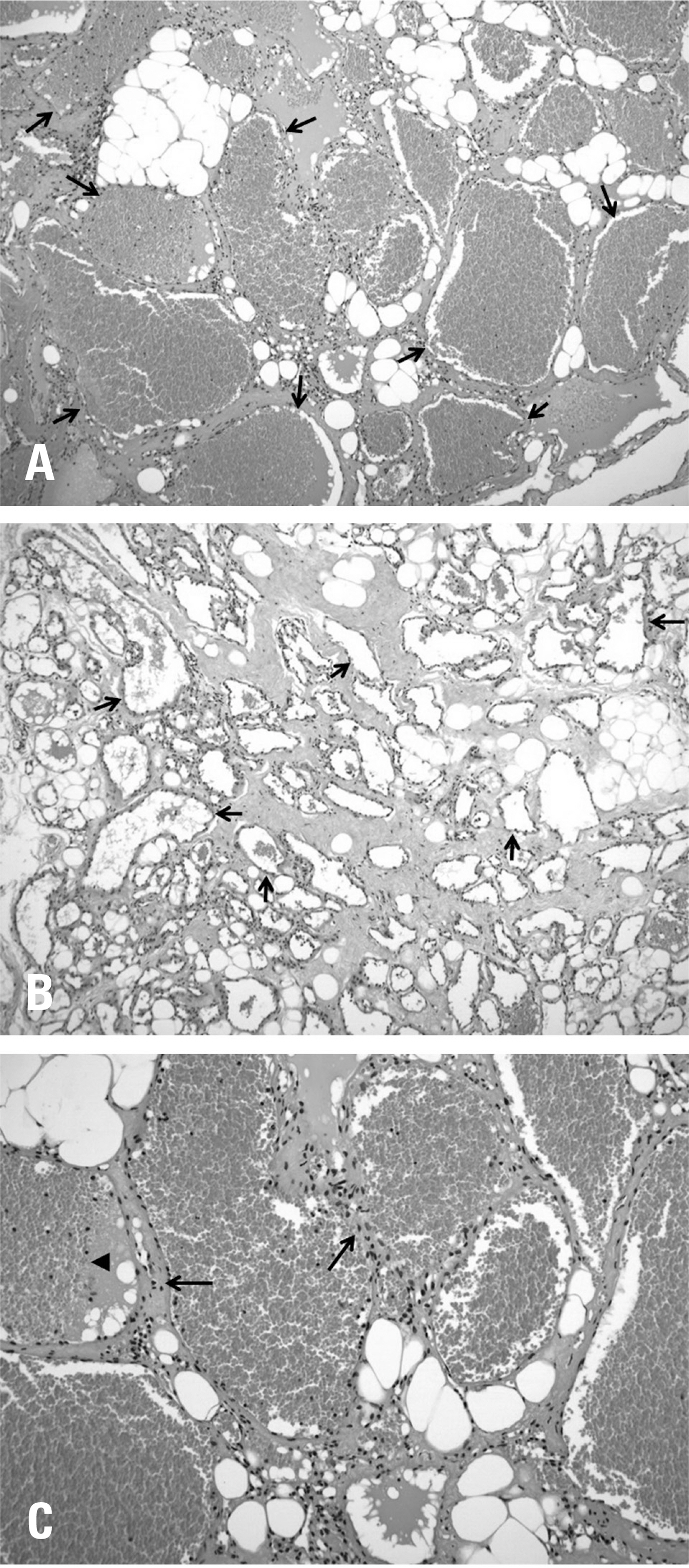
The histopathologic examination revealed a cavernous hemangioma, which was the final diagnosis. The outcome was favorable in that only operation-related mild back pain remained, without any neurologic deficits, after a postoperative follow-up of 2 years and 3 months. No recurrence was observed on MRI at 2 years postoperatively.
CONCLUSION
Pure epidural spinal cavernous hemangioma is very rare, and it is very difficult to differentiate from other epidural lesions. However, we believe that it should be included in the differential diagnosis of spinal epidural tumors due to its favorable prognosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Murphey MD, Fairbairn KJ, Parman LM, et al. From the archives of the AFIP. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation. Radiographics. 1995 Jul; 15(4):893–917. DOI: 10.1148/radiograph-ics.15.4.7569134.
Article2. Khalatbari MR, Abbassioun K, Amirjmshidi A. Solitary spinal epidural cavernous angioma: report of nine surgically treated cases and review of the literature. Eur Spine J. 2013 Mar; 22(3):542–7. DOI: 10.1007/s00586-012-2526-2.
Article3. Li TY, Xu YL, Yang J, et al. Primary spinal epidural cavernous hemangioma: clinical features and surgical outcome in 14 cases. J Neurosurg Spine. 2015 Jan; 22(1):39–46. DOI: 10.3171/2014.9.SPINE13901.
Article4. Hatiboglu MA, Iplikcioglu AC, Ozcan D. Epidural spinal cavernous hemangioma. Neurol Med Chir (Tokyo). 2006 Sep; 46(9):455–8. DOI: 10.2176/nmc.46.455.5. Esene IN, Ashour AM, Marvin E, et al. Pure spinal epidural cavernous hemangioma: A case series of seven cases. J Craniovertebr Junction Spine. 2016 Jul-Sep; 7(3):176–83. DOI: 10.4103/0974-8237.188419.
Article6. Feng J, Xu YK, Li L, et al. MRI diagnosis and preoperative evaluation for pure epidural cavernous hemangiomas. Neuroradiology. 2009 Nov; 51(11):741–7. DOI: 10.1007/s00234-009-0555-2. cavernous hemangioma. Acta Neurochir (Wien). 2012 Apr; 154(4):739–45. DOI: 10.1007/s00701-012-1295-3.
Article8. Min HJ, Kim KW, Kim YH, et al. Epidural hemangioma: a case report. J Korean Soc Spine Surg. 2001 Sep; 8(3):253–8. DOI: 10.4184/jkss.2001.8.3.253.9. Aoyagi N, Kojima K, Kasai H. Review of spinal epidural cavernous hemangioma. Neurol Med Chir (Tokyo). 2003 Oct; 43(10):471–5. DOI: 10.2176/nmc.43.471.
Article10. Lee JW, Cho EY, Hong SH, et al. Spinal epidural hemangiomas: various types of MR imaging features with histopathologic correlation. AJNR Am J Neuroradiol. 2007 Aug; 28(7):1242–8. DOI: 10.3174/ajnr.A0563.
Article11. Sohn MJ, Lee DJ, Jeon SR, et al. Spinal radiosurgical treatment for thoracic epidural cavernous hemangioma presenting as radiculomyelopathy: technical case report. Neurosurgery. 2009 Jun; 64(6):E1202–3. DOI: 10.1227/01. NEU.0000345940.21674.AE.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Epidural Cavernous Hemangioma in the Thoraic Spine
- Spinal Epidural Cavernous Hemangioma of the Upper Thoracic Vertebrae: Case Report
- Pure Thoracic Spinal Epidural Cavernous Hemangioma with Spinal Cord Compression: A Case Report
- Pure Epidural Cavernous Hemangioma in Thoracic Region: A Case Report
- Pure Extradural Cavernous Hemangioma Presenting as a Lumbar Radiculopathy