World J Mens Health.
2019 Jan;37(1):99-104. 10.5534/wjmh.180049.
Neutrophil-Lymphocyte Ratio Predicts Organ Salvage in Testicular Torsion with Marginal Diagnostic Delay
- Affiliations
-
- 1Department of Urology, College of Medicine, Yeungnam University, Daegu, Korea. urokyh@naver.com
- KMID: 2429727
- DOI: http://doi.org/10.5534/wjmh.180049
Abstract
- PURPOSE
Though prompt diagnosis to minimize symptom duration (SD) is highly associated with organ salvage in cases of testicular torsion (TT), SD is subjective and hard to determine. We thus investigated the clinical implications of systemic inflammatory responses (SIRs) as potential surrogates of SD to improve testis survival.
MATERIALS AND METHODS
Sixty men with TT that underwent immediate operation among orchiectomy and orchiopexy following a visit to a single emergency department were retrospectively enrolled. Mandatory laboratory tests conducted included neutrophil, lymphocyte, and platelet counts.
RESULTS
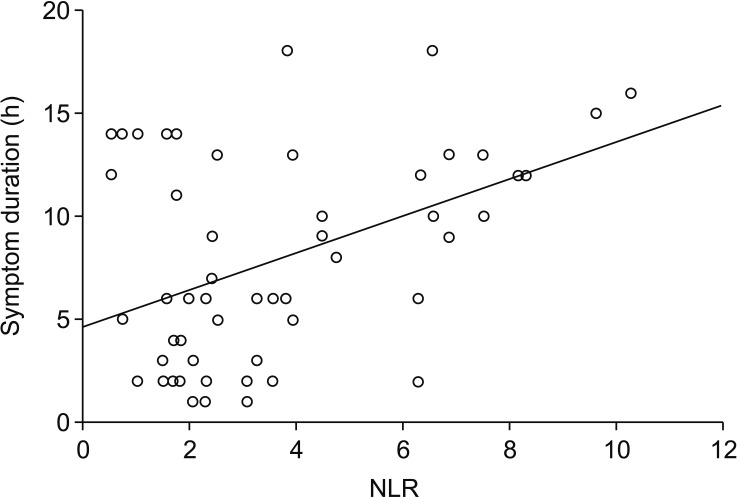
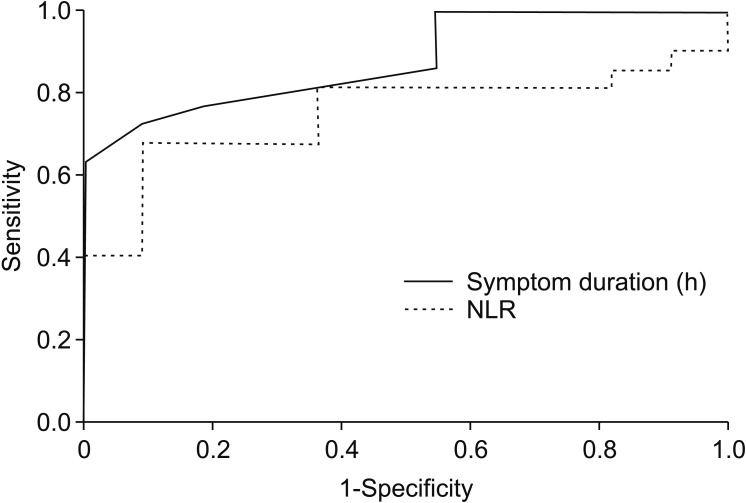
Mean age and SD was 15.7±3.7 years and 8.27±4.98 hours, respectively. Thirty-eight (63.3%) underwent orchiectomy and the remaining 22 underwent orchiopexy. Leukocytosis (p=0.001) and neutrophil-lymphocyte ratio (NLR, p < 0.001) were significantly lower in the orchiopexy group as was SD (3.27±1.88 vs. 11.16±3.80, p < 0.001). Although multivariate model showed that the only single variable associated with receipt of orchiopexy was SD (odds ratio [OR]=0.259, p < 0.001), it also revealed NLR as a sole SIR associated with SD (B=0.894, p < 0.001). While 93.3% with a SD of within 3 hours underwent orchiopexy, only 26.6% of affected testes were preserved between 3 to 12 hours (n=30). When multivariable analysis was applied to those with window period, NLR alone predicted orchiopexy rather than orchiectomy (p=0.034, OR=0.635, p=0.013). The area under curve between SD (0.882) and NLR (0.756) was similar (p=0.14).
CONCLUSIONS
This study showed NLR independently predicted testis survival by proper surgical correction particularly for patients with marginally delayed diagnosis, which suggest the clinical usefulness for identifying candidates for orchiopexy in emergency setting.
MeSH Terms
Figure
Reference
-
1. Zhao LC, Lautz TB, Meeks JJ, Maizels M. Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. J Urol. 2011; 186:2009–2013. PMID: 21944120.
Article2. Bodiwala D, Summerton DJ, Terry TR. Testicular prostheses: development and modern usage. Ann R Coll Surg Engl. 2007; 89:349–353. PMID: 17535609.
Article3. Fisch H, Laor E, Reid RE, Tolia BM, Freed SZ. Gonadal dysfunction after testicular torsion: luteinizing hormone and follicle-stimulating hormone response to gonadotropin releasing hormone. J Urol. 1988; 139:961–964. PMID: 3129583.
Article4. Selbst SM, Friedman MJ, Singh SB. Epidemiology and etiology of malpractice lawsuits involving children in US emergency departments and urgent care centers. Pediatr Emerg Care. 2005; 21:165–169. PMID: 15744194.5. Bowlin PR, Gatti JM, Murphy JP. Pediatric testicular torsion. Surg Clin North Am. 2017; 97:161–172. PMID: 27894425.
Article6. Boettcher M, Bergholz R, Krebs TF, Wenke K, Aronson DC. Clinical predictors of testicular torsion in children. Urology. 2012; 79:670–674. PMID: 22386422.
Article7. Rampaul MS, Hosking SW. Testicular torsion: most delay occurs outside hospital. Ann R Coll Surg Engl. 1998; 80:169–172.8. Nasrallah P, Nair G, Congeni J, Bennett CL, McMahon D. Testicular health awareness in pubertal males. J Urol. 2000; 164:1115–1117. PMID: 10958755.
Article9. Bayne AP, Madden-Fuentes RJ, Jones EA, Cisek LJ, Gonzales ET, Reavis KM, et al. Factors associated with delayed treatment of acute testicular torsion-do demographics or interhospital transfer matter? J Urol. 2010; 184(4 Suppl):1743–1747. PMID: 20728168.
Article10. Yiee JH, Chang L, Kaplan A, Kwan L, Chung PJ, Litwin MS. Patterns of care in testicular torsion: influence of hospital transfer on testicular outcomes. J Pediatr Urol. 2013; 9:713–720. PMID: 23896260.
Article11. Barada JH, Weingarten JL, Cromie WJ. Testicular salvage and age-related delay in the presentation of testicular torsion. J Urol. 1989; 142:746–748. PMID: 2769854.
Article12. Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005; 159:1167–1171. PMID: 16330742.
Article13. Güneş M, Umul M, Altok M, Akyuz M, İşoğlu CS, Uruc F, et al. Predictive role of hematologic parameters in testicular torsion. Korean J Urol. 2015; 56:324–329. PMID: 25874047.
Article14. Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013; 13:159–175. PMID: 23435331.
Article15. Bitkin A, Aydın M, Özgür BC, Irkilata L, Akgunes E, Keles M, et al. Can haematologic parameters be used for differential diagnosis of testicular torsion and epididymitis? Andrologia. 2018; 50:DOI: 10.1111/and.12819.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical observation on torsion of the testis
- The Pathological Anatomy of Intermittent Testicular Torsion
- Letter to the editor: Predictive value of the neutrophil-lymphocyte ratio and mean platelet volume in testicular torsion
- Twist and Shout: A Clinical and Experimental Review of Testicular Torsion
- Role of Early Scrotal Exploration for Torsion of Testis and Appendages in Children