Yonsei Med J.
2017 Mar;58(2):401-406. 10.3349/ymj.2017.58.2.401.
The Level of Serum and Urinary Nephrin in Normal Pregnancy and Pregnancy with Subsequent Preeclampsia
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea. jaykwon@yuhs.ac
- 2Department of Obstetrics and Gynecology, MizMedi Women's Hospital, Seoul, Korea.
- 3Department of Bioanalysis, Seoul Medical Science Institute & Seoul Clinical Laboratories, Seoul, Korea.
- 4Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2427130
- DOI: http://doi.org/10.3349/ymj.2017.58.2.401
Abstract
- PURPOSE
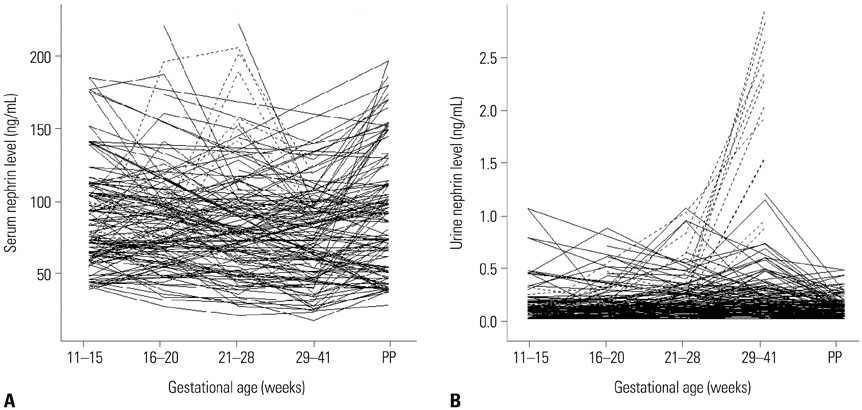
The aim of this study was to evaluate serum and urinary nephrin levels of normal pregnancy to establish a standard reference value and to compare them with patients who subsequently developed preeclampsia (PE).
MATERIALS AND METHODS
In this prospective study, 117 healthy singleton pregnancies were enrolled between 6 to 20 weeks of gestation at 2 participating medical centers during October 2010 to March 2012. Urine and serum samples were collected at the time of enrollment, each trimester, and at 4 to 6 weeks postpartum. Enzyme-linked immunosorbent assay for nephrin was performed and samples from patients who subsequently developed PE were compared to the normal patients.
RESULTS
Of 117 patients initially enrolled, 99 patients delivered at the study centers and of those patients, 12 (12.1%) developed PE at a median gestational age of 34âºâ´ weeks (range 29âºâµ-36âºâ¶). In the normal patients (n=68), serum nephrin level decreased and urinary nephrin level increased during the latter of pregnancy. In 12 patients who subsequently developed PE, a significant rise in the 3rd trimester serum and urinary nephrin levels, compared to the controls, was observed (p<0.001), and this increase occurred 9 days prior to the onset of clinical disease.
CONCLUSION
As the onset of PE was preceded by the rise in the serum and urinary nephrin in comparison to normal pregnancy, serum and urinary nephrin may be a useful predictive marker of PE.
Keyword
MeSH Terms
-
Adult
Biomarkers/blood/urine
Case-Control Studies
Enzyme-Linked Immunosorbent Assay
Female
Gestational Age
Humans
Membrane Proteins/*blood/*urine
Pre-Eclampsia/blood/*etiology/urine
Pregnancy
Pregnancy Proteins
Pregnancy Trimester, Third/blood/urine
Prospective Studies
Reference Standards
Biomarkers
Membrane Proteins
Pregnancy Proteins
Figure
Reference
-
1. Tryggvason K, Wartiovaara J. Molecular basis of glomerular permselectivity. Curr Opin Nephrol Hypertens. 2001; 10:543–549.
Article2. Kestilä M, Lenkkeri U, Männikkö M, Lamerdin J, McCready P, Putaala H, et al. Positionally cloned gene for a novel glomerular protein--nephrin--is mutated in congenital nephrotic syndrome. Mol Cell. 1998; 1:575–582.
Article3. Ng DP, Tai BC, Tan E, Leong H, Nurbaya S, Lim XL, et al. Nephrinuria associates with multiple renal traits in type 2 diabetes. Nephrol Dial Transplant. 2011; 26:2508–2514.
Article4. Ziyadeh FN, Wolf G. Pathogenesis of the podocytopathy and proteinuria in diabetic glomerulopathy. Curr Diabetes Rev. 2008; 4:39–45.
Article5. Alter ML, Kretschmer A, Von Websky K, Tsuprykov O, Reichetzeder C, Simon A, et al. Early urinary and plasma biomarkers for experimental diabetic nephropathy. Clin Lab. 2012; 58:659–671.6. Jim B, Ghanta M, Qipo A, Fan Y, Chuang PY, Cohen HW, et al. Dysregulated nephrin in diabetic nephropathy of type 2 diabetes: a cross sectional study. PLoS One. 2012; 7:e36041.
Article7. Li LL, Chen ZQ, Wang YH, Zhang JH, Yin ZW, Li LL, et al. Relationship between urinary nephrin and urinary albumin changes in diabetic rats and effects of yiqiyangyinhuayutongluo recipe. J Tradit Chin Med. 2012; 32:278–282.
Article8. Machado JR, Rocha LP, Neves PD, Cobô Ede C, Silva MV, Castellano LR, et al. An overview of molecular mechanism of nephrotic syndrome. Int J Nephrol. 2012; 2012:937623.
Article9. Matsusaka T, Sandgren E, Shintani A, Kon V, Pastan I, Fogo AB, et al. Podocyte injury damages other podocytes. J Am Soc Nephrol. 2011; 22:1275–1285.
Article10. Tufro A, Veron D. VEGF and podocytes in diabetic nephropathy. Semin Nephrol. 2012; 32:385–393.
Article11. Roberts JM, Funai EF. Pregnancy related hypertension. In : Creasy R, Resnik R, Iams JD, editors. Maternal-Fetal Medicine: Principles and Practice. 6th ed. Philadelphia: Saunders Elsevier;2009. p. 651–688.12. Krane NK, Hamrahian M. Pregnancy: kidney diseases and hypertension. Am J Kidney Dis. 2007; 49:336–345.
Article13. Makris A, Thornton C, Thompson J, Thomson S, Martin R, Ogle R, et al. Uteroplacental ischemia results in proteinuric hypertension and elevated sFLT-1. Kidney Int. 2007; 71:977–984.
Article14. Aita K, Etoh M, Hamada H, Yokoyama C, Takahashi A, Suzuki T, et al. Acute and transient podocyte loss and proteinuria in preeclampsia. Nephron Clin Pract. 2009; 112:c65–c70.
Article15. Garovic VD, Craici IM, Wagner SJ, White WM, Brost BC, Rose CH, et al. Mass spectrometry as a novel method for detection of podocyturia in pre-eclampsia. Nephrol Dial Transplant. 2013; 28:1555–1561.
Article16. Son GH, Kim JH, Hwang JH, Kim YH, Park YW, Kwon JY. Urinary excretion of nephrin in patients with severe preeclampsia. Urinary nephrin in preeclampsia. Hypertens Pregnancy. 2011; 30:408–413.17. Son GH, Kwon JY, Lee S, Park J, Kim YJ, Yun B, et al. Comparison of serum and urinary nephrin levels between normal pregnancies and severe preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2013; 166:139–144.
Article18. Henao DE, Arias LF, Mathieson PW, Ni L, Welsh GI, Bueno JC, et al. Preeclamptic sera directly induce slit-diaphragm protein redistribution and alter podocyte barrier-forming capacity. Nephron Exp Nephrol. 2008; 110:e73–e81.
Article19. Collino F, Bussolati B, Gerbaudo E, Marozio L, Pelissetto S, Benedetto C, et al. Preeclamptic sera induce nephrin shedding from podocytes through endothelin-1 release by endothelial glomerular cells. Am J Physiol Renal Physiol. 2008; 294:F1185–F1194.
Article20. Wang Y, Zhao S, Loyd S, Groome LJ. Increased urinary excretion of nephrin, podocalyxin, and βig-h3 in women with preeclampsia. Am J Physiol Renal Physiol. 2012; 302:F1084–F1089.
Article21. Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004; 350:672–683.
Article22. Lynch AM, Murphy JR, Gibbs RS, Levine RJ, Giclas PC, Salmon JE, et al. The interrelationship of complement-activation fragments and angiogenesis-related factors in early pregnancy and their association with pre-eclampsia. BJOG. 2010; 117:456–462.
Article23. Staff AC, Benton SJ, von Dadelszen P, Roberts JM, Taylor RN, Powers RW, et al. Redefining preeclampsia using placenta-derived biomarkers. Hypertension. 2013; 61:932–942.
Article24. Roberts JM, Bell MJ. If we know so much about preeclampsia, why haven’t we cured the disease? J Reprod Immunol. 2013; 99:1–9.
Article25. Koga K, Osuga Y, Yoshino O, Hirota Y, Ruimeng X, Hirata T, et al. Elevated serum soluble vascular endothelial growth factor receptor 1 (sVEGFR-1) levels in women with preeclampsia. J Clin Endocrinol Metab. 2003; 88:2348–2351.
Article26. Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003; 111:649–658.
Article27. Myatt L, Clifton RG, Roberts JM, Spong CY, Hauth JC, Varner MW, et al. First-trimester prediction of preeclampsia in nulliparous women at low risk. Obstet Gynecol. 2012; 119:1234–1242.
Article28. Myers JE, Kenny LC, McCowan LM, Chan EH, Dekker GA, Poston L, et al. Angiogenic factors combined with clinical risk factors to predict preterm pre-eclampsia in nulliparous women: a predictive test accuracy study. BJOG. 2013; 120:1215–1223.
Article29. Myers JE, Tuytten R, Thomas G, Laroy W, Kas K, Vanpoucke G, et al. Integrated proteomics pipeline yields novel biomarkers for predicting preeclampsia. Hypertension. 2013; 61:1281–1288.
Article30. Roberts JM, Cooper DW. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001; 357:53–56.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum to “The Level of Serum and Urinary Nephrin in Normal Pregnancy and Pregnancy with Subsequent Preeclampsia” by Jung YJ, et al.(Yonsei Med J 2017;58(2):401-406.)
- Urinary nephrin: A new predictive marker for pregnancies with preeclampsia and small-for-gestational age infants
- Difference in serum nephrin expression between normal and preeclamptic pregnancies: A preliminary study
- Study on the Hematologic and Blood Chemical Tests in Preelcampsia
- Umbilical Vein Serum Nitric Oxide Concentration and Fetal Growth Restriction in Preeclampsia