Korean J Obstet Gynecol.
2012 Aug;55(8):546-551. 10.5468/KJOG.2012.55.8.546.
Difference in serum nephrin expression between normal and preeclamptic pregnancies: A preliminary study
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Institute of Women's Medical Life Science, Yonsei University College of Medicine, Seoul, Korea. ywparkob@yuhs.ac
- 2Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Biochemistry, Yonsei University, Seoul, Korea.
- KMID: 2078103
- DOI: http://doi.org/10.5468/KJOG.2012.55.8.546
Abstract
OBJECTIVE
Nephrin is one of the slit membrane proteins of podocytes in the kidney. It is known that the nephrin is shed in the urine in nephropathy accompanying proteinuira. So the aim of this study was to evaluate the difference in the serum nephrin expression between normal and preeclamptic pregnancies.
METHODS
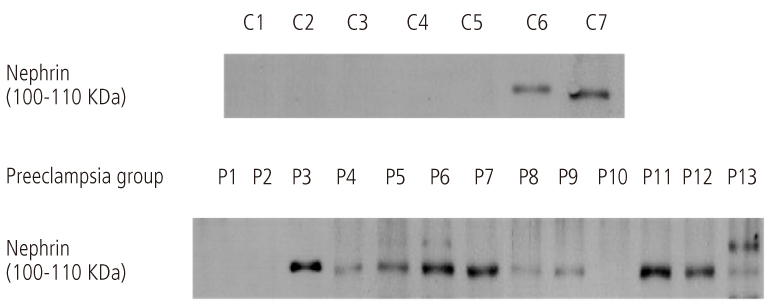
A total of 20 pregnant women from May to September 2008 who received prenatal care and underwent delivery at our institute participated in the study. The preeclamptic group includes 13 women diagnosed as preeclampsia and a normal group of 7. Their serum were collected before delivery and analyzed by Western blotting for comparing serum nephrin expression.
RESULTS
There was no difference in age, body weight of pregnant women, blood urea nitrogen, serum creatinine, urine creatinine level and gestational age between two groups. However, preeclampsia group had significantly higher systolic and diastolic blood pressure (P<0.001), serum soluble fms-like tyrosine kinase-1 level (P=0.002), and lower birth weight (P=0.011). In serum Western blot analysis, serum nephrin was detected in 10 of 13 in preeclampsia women (76.9%) but only in 2 of 7 (28.6%) in normal pregnancy women showing statistically significant difference (P=0.032).
CONCLUSION
A higher prevalence of nephrin expression in the maternal serum was found in the preeclampsia when compared to the normal pregnancy.
Keyword
MeSH Terms
Figure
Reference
-
1. Levine RJ, Thadhani R, Qian C, Lam C, Lim KH, Yu KF, et al. Urinary placental growth factor and risk of preeclampsia. JAMA. 2005. 293:77–85.2. Walker JJ. Pre-eclampsia. Lancet. 2000. 356:1260–1265.3. Roberts JM, Cooper DW. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001. 357:53–56.4. Ward K, Hata A, Jeunemaitre X, Helin C, Nelson L, Namikawa C, et al. A molecular variant of angiotensinogen associated with preeclampsia. Nat Genet. 1993. 4:59–61.5. Wallukat G, Homuth V, Fischer T, Lindschau C, Horstkamp B, Jüpner A, et al. Patients with preeclampsia develop agonistic autoantibodies against the angiotensin AT1 receptor. J Clin Invest. 1999. 103:945–952.6. Buhimschi IA, Saade GR, Chwalisz K, Garfield RE. The nitric oxide pathway in pre-eclampsia: pathophysiological implications. Hum Reprod Update. 1998. 4:25–42.7. Faas MM, Schuiling GA, Baller JF, Visscher CA, Bakker WW. A new animal model for human preeclampsia: ultra-low-dose endotoxin infusion in pregnant rats. Am J Obstet Gynecol. 1994. 171:158–164.8. Roberts JM, Redman CW. Pre-eclampsia: more than pregnancy-induced hypertension. Lancet. 1993. 341:1447–1451.9. Cockell AP, Learmont JG, Smárason AK, Redman CW, Sargent IL, Poston L. Human placental syncytiotrophoblast microvillous membranes impair maternal vascular endothelial function. Br J Obstet Gynaecol. 1997. 104:235–240.10. Holzgreve W, Ghezzi F, Di Naro E, Gänshirt D, Maymon E, Hahn S. Disturbed feto-maternal cell traffic in preeclampsia. Obstet Gynecol. 1998. 91:669–672.11. Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003. 111:649–658.12. Buhimschi CS, Magloire L, Funai E, Norwitz ER, Kuczynski E, Martin R, et al. Fractional excretion of angiogenic factors in women with severe preeclampsia. Obstet Gynecol. 2006. 107:1103–1113.13. Page NM, Woods RJ, Gardiner SM, Lomthaisong K, Gladwell RT, Butlin DJ, et al. Excessive placental secretion of neurokinin B during the third trimester causes pre-eclampsia. Nature. 2000. 405:797–800.14. Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004. 350:672–683.15. Koga K, Osuga Y, Yoshino O, Hirota Y, Ruimeng X, Hirata T, et al. Elevated serum soluble vascular endothelial growth factor receptor 1 (sVEGFR-1) levels in women with preeclampsia. J Clin Endocrinol Metab. 2003. 88:2348–2351.16. Taylor RN, Grimwood J, Taylor RS, McMaster MT, Fisher SJ, North RA. Longitudinal serum concentrations of placental growth factor: evidence for abnormal placental angiogenesis in pathologic pregnancies. Am J Obstet Gynecol. 2003. 188:177–182.17. Zhou Y, Damsky CH, Fisher SJ. Preeclampsia is associated with failure of human cytotrophoblasts to mimic a vascular adhesion phenotype. One cause of defective endovascular invasion in this syndrome? J Clin Invest. 1997. 99:2152–2164.18. Torry DS, Wang HS, Wang TH, Caudle MR, Torry RJ. Preeclampsia is associated with reduced serum levels of placenta growth factor. Am J Obstet Gynecol. 1998. 179:1539–1544.19. Thadhani R, Mutter WP, Wolf M, Levine RJ, Taylor RN, Sukhatme VP, et al. First trimester placental growth factor and soluble fms-like tyrosine kinase 1 and risk for preeclampsia. J Clin Endocrinol Metab. 2004. 89:770–775.20. Tsatsaris V, Goffin F, Munaut C, Brichant JF, Pignon MR, Noel A, et al. Overexpression of the soluble vascular endothelial growth factor receptor in preeclamptic patients: pathophysiological consequences. J Clin Endocrinol Metab. 2003. 88:5555–5563.21. Baker PN, Krasnow J, Roberts JM, Yeo KT. Elevated serum levels of vascular endothelial growth factor in patients with preeclampsia. Obstet Gynecol. 1995. 86:815–821.22. Simmons LA, Hennessy A, Gillin AG, Jeremy RW. Uteroplacental blood flow and placental vascular endothelial growth factor in normotensive and pre-eclamptic pregnancy. BJOG. 2000. 107:678–685.23. Zhou Y, McMaster M, Woo K, Janatpour M, Perry J, Karpanen T, et al. Vascular endothelial growth factor ligands and receptors that regulate human cytotrophoblast survival are dysregulated in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelets syndrome. Am J Pathol. 2002. 160:1405–1423.24. Hauser PV, Collino F, Bussolati B, Camussi G. Nephrin and endothelial injury. Curr Opin Nephrol Hypertens. 2009. 18:3–8.25. Garovic VD, Wagner SJ, Petrovic LM, Gray CE, Hall P, Sugimoto H, et al. Glomerular expression of nephrin and synaptopodin, but not podocin, is decreased in kidney sections from women with preeclampsia. Nephrol Dial Transplant. 2007. 22:1136–1143.26. Foster RR, Saleem MA, Mathieson PW, Bates DO, Harper SJ. Vascular endothelial growth factor and nephrin interact and reduce apoptosis in human podocytes. Am J Physiol Renal Physiol. 2005. 288:F48–F57.27. Sugimoto H, Hamano Y, Charytan D, Cosgrove D, Kieran M, Sudhakar A, et al. Neutralization of circulating vascular endothelial growth factor (VEGF) by anti-VEGF antibodies and soluble VEGF receptor 1 (sFlt-1) induces proteinuria. J Biol Chem. 2003. 278:12605–12608.28. Karumanchi SA, Lindheimer MD. Preeclampsia and the kidney: footprints in the urine. Am J Obstet Gynecol. 2007. 196:287–288.29. Zhao S, Gu X, Groome LJ, Wang Y. Decreased nephrin and GLEPP-1, but increased VEGF, Flt-1, and nitrotyrosine, expressions in kidney tissue sections from women with preeclampsia. Reprod Sci. 2009. 16:970–979.30. Collino F, Bussolati B, Gerbaudo E, Marozio L, Pelissetto S, Benedetto C, et al. Preeclamptic sera induce nephrin shedding from podocytes through endothelin-1 release by endothelial glomerular cells. Am J Physiol Renal Physiol. 2008. 294:F1185–F1194.31. Putaala H, Soininen R, Kilpeläinen P, Wartiovaara J, Tryggvason K. The murine nephrin gene is specifically expressed in kidney, brain and pancreas: inactivation of the gene leads to massive proteinuria and neonatal death. Hum Mol Genet. 2001. 10:1–8.32. Garovic VD, Wagner SJ, Turner ST, Rosenthal DW, Watson WJ, Brost BC, et al. Urinary podocyte excretion as a marker for preeclampsia. Am J Obstet Gynecol. 2007. 196:320.e1–320.e7.33. Beall MH, Amidi F, Gayle DA, Wang S, Beloosesky R, Ross MG. Placental and fetal membrane Nephrin and Neph1 gene expression: response to inflammation. J Soc Gynecol Investig. 2005. 12:298–302.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The nitric oxide synthase activity and expression in human placenta from preeclamptic pregnancies
- Differential expression of Matrix Metalloproteinase (MMP)-2, -9 in normal and severe preeclamptic human placentas
- Urinary nephrin: A new predictive marker for pregnancies with preeclampsia and small-for-gestational age infants
- Immunohistochemical Expression of Placental Nitric Oxide Synthase in Preeclampsia and Normal Pregnancy
- The effect of the sera from severe preeclamptic patients on endothelial cell viability and endothelin-1 in cultured human umbilical vein endothelial cells