J Periodontal Implant Sci.
2018 Oct;48(5):326-333. 10.5051/jpis.2018.48.5.326.
Simplified nonsurgical treatment of peri-implantitis using chlorhexidine and minocycline hydrochloride
- Affiliations
-
- 1Department of Periodontology, Pusan National University Dental Hospital, Dental Research Institute, Yangsan, Korea. jrapa@pusan.ac.kr
- 2Department of Periodontology, Pusan National University School of Dentistry, Yangsan, Korea.
- KMID: 2424866
- DOI: http://doi.org/10.5051/jpis.2018.48.5.326
Abstract
- PURPOSE
The present study investigated the outcomes of a newly-developed, simple, and practical nonsurgical treatment modality suitable for most forms of intrabony defects around failing dental implants using intrasulcular delivery of chlorhexidine solution and minocycline hydrochloride (HCl).
METHODS
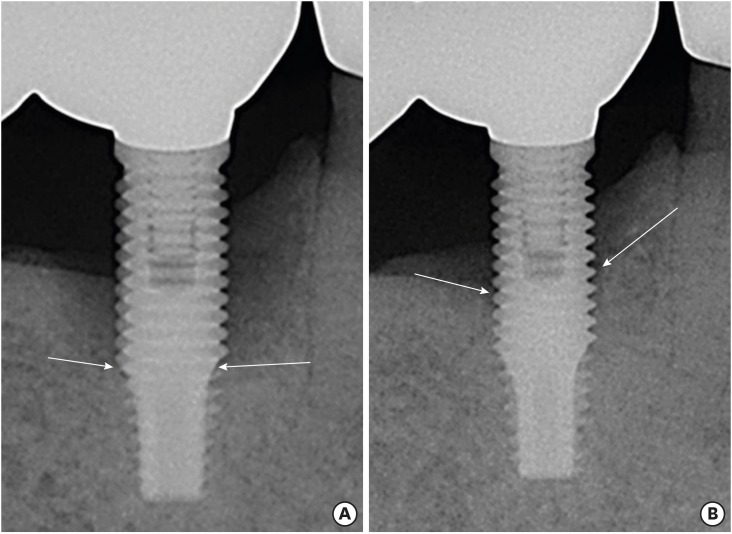
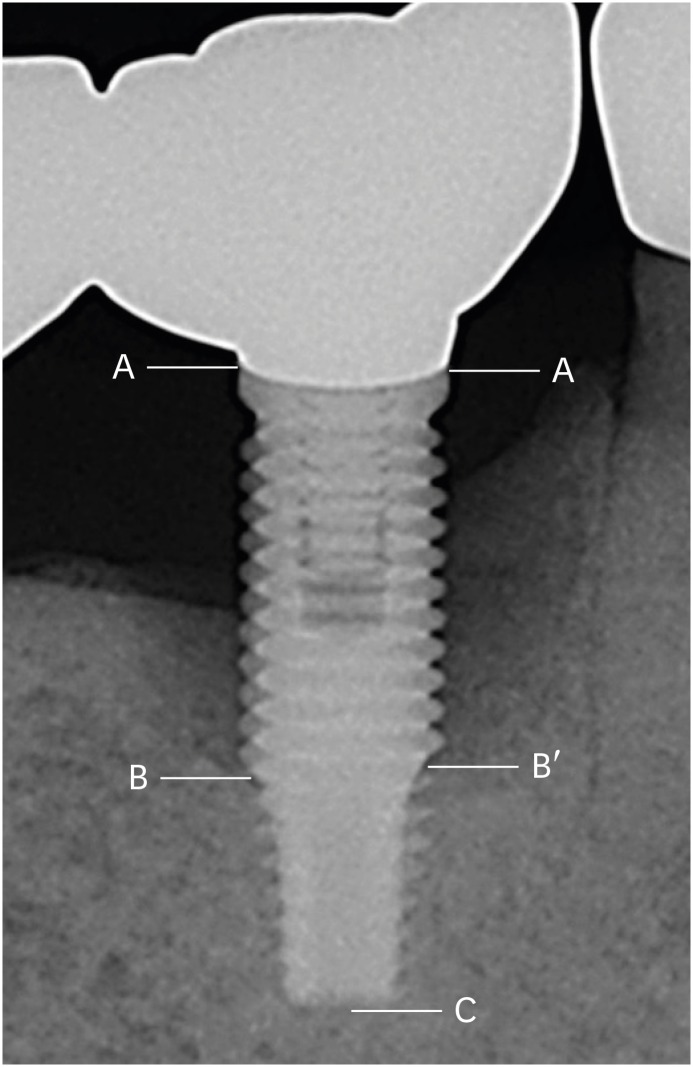
Forty-five dental implants in 20 patients diagnosed with peri-implantitis were included. At baseline and the study endpoint, the probing pocket depth (PPD), clinical attachment level (CAL), and the presence of bleeding on probing (BOP) at 6 sites around each implant were recorded. The radiographic osseous defect morphology at the mesial or distal proximal aspect of each implant was classified as 1) narrow or wide and 2) shallow or deep. For a comparative analysis of bone changes according to the defect morphology, the distance from the implant shoulder to the most coronal bone-to-implant contact point (DIB) at the mesial and distal aspects of each implant was measured at baseline and the endpoint. Patients were scheduled to visit the clinic every 2-4 weeks for intrasulcular irrigation of chlorhexidine and delivery of minocycline HCl.
RESULTS
We observed statistically significant decreases in PPD, CAL, and BOP after treatment. At the endpoint, bone levels increased in all defects, regardless of the osseous morphology of the intrabony defect. The mean DIB change in deep defects was significantly greater than that in shallow defects. Although the mean bone gain in narrow defects was greater than in wide defects, the difference was not statistically significant.
CONCLUSIONS
We propose that significant and sustainable improvements in both clinical and radiographic parameters can be expected when intrabony defects around dental implants are managed through a simple nonsurgical approach involving combined intrasulcular chlorhexidine irrigation and local delivery of minocycline HCl.
MeSH Terms
Figure
Reference
-
1. Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998; 17:63–76. PMID: 10337314.
Article2. Heitz-Mayfield LJ, Lang NP. Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontol 2000. 2010; 53:167–181. PMID: 20403112.
Article3. Hultin M, Gustafsson A, Hallström H, Johansson LA, Ekfeldt A, Klinge B. Microbiological findings and host response in patients with peri-implantitis. Clin Oral Implants Res. 2002; 13:349–358. PMID: 12175371.
Article4. Karring ES, Stavropoulos A, Ellegaard B, Karring T. Treatment of peri-implantitis by the Vector system. Clin Oral Implants Res. 2005; 16:288–293. PMID: 15877748.5. Renvert S, Samuelsson E, Lindahl C, Persson GR. Mechanical non-surgical treatment of peri-implantitis: a double-blind randomized longitudinal clinical study. I: clinical results. J Clin Periodontol. 2009; 36:604–609. PMID: 19538334.
Article6. van Steenberghe D, Bercy P, Kohl J, De Boever J, Adriaens P, Vanderfaeillie A, et al. Subgingival minocycline hydrochloride ointment in moderate to severe chronic adult periodontitis: a randomized, double-blind, vehicle-controlled, multicenter study. J Periodontol. 1993; 64:637–644. PMID: 8396177.
Article7. Mombelli A, Feloutzis A, Brägger U, Lang NP. Treatment of peri-implantitis by local delivery of tetracycline. Clinical, microbiological and radiological results. Clin Oral Implants Res. 2001; 12:287–294. PMID: 11488856.8. Büchter A, Meyer U, Kruse-Lösler B, Joos U, Kleinheinz J. Sustained release of doxycycline for the treatment of peri-implantitis: randomised controlled trial. Br J Oral Maxillofac Surg. 2004; 42:439–444. PMID: 15336770.
Article9. Salvi GE, Persson GR, Heitz-Mayfield LJ, Frei M, Lang NP. Adjunctive local antibiotic therapy in the treatment of peri-implantitis II: clinical and radiographic outcomes. Clin Oral Implants Res. 2007; 18:281–285. PMID: 17355354.
Article10. Persson GR, Salvi GE, Heitz-Mayfield LJ, Lang NP. Antimicrobial therapy using a local drug delivery system (Arestin) in the treatment of peri-implantitis. I: Microbiological outcomes. Clin Oral Implants Res. 2006; 17:386–393. PMID: 16907769.11. Lang NP, Wilson TG, Corbet EF. Biological complications with dental implants: their prevention, diagnosis and treatment. Clin Oral Implants Res. 2000; 11(Suppl 1):146–155. PMID: 11168263.
Article12. Liñares A, Cortellini P, Lang NP, Suvan J, Tonetti MS. European Research Group on Periodontology (ErgoPerio). Guided tissue regeneration/deproteinized bovine bone mineral or papilla preservation flaps alone for treatment of intrabony defects. II: radiographic predictors and outcomes. J Clin Periodontol. 2006; 33:351–358. PMID: 16634957.
Article13. Behneke A, Behneke N, d'Hoedt B, Wagner W. Hard and soft tissue reactions to ITI screw implants: 3-year longitudinal results of a prospective study. Int J Oral Maxillofac Implants. 1997; 12:749–757. PMID: 9425755.14. Brägger U, Bürgin WB, Hämmerle CH, Lang NP. Associations between clinical parameters assessed around implants and teeth. Clin Oral Implants Res. 1997; 8:412–421. PMID: 9612146.
Article15. Zarb GA, Symington JM. Osseointegrated dental implants: preliminary report on a replication study. J Prosthet Dent. 1983; 50:271–276. PMID: 6352914.
Article16. Stavropoulos A, Wikesjö UM. Influence of defect dimensions on periodontal wound healing/regeneration in intrabony defects following implantation of a bovine bone biomaterial and provisions for guided tissue regeneration: an experimental study in the dog. J Clin Periodontol. 2010; 37:534–543. PMID: 20507377.
Article17. Cortellini P, Carnevale G, Sanz M, Tonetti MS. Treatment of deep and shallow intrabony defects. A multicenter randomized controlled clinical trial. J Clin Periodontol. 1998; 25:981–987. PMID: 9869347.
Article18. Heitz-Mayfield LJ, Salvi GE, Botticelli D, Mombelli A, Faddy M, Lang NP, et al. Anti-infective treatment of peri-implant mucositis: a randomised controlled clinical trial. Clin Oral Implants Res. 2011; 22:237–241. PMID: 21251076.
Article19. Máximo MB, de Mendonça AC, Renata Santos V, Figueiredo LC, Feres M, Duarte PM. Short-term clinical and microbiological evaluations of peri-implant diseases before and after mechanical anti-infective therapies. Clin Oral Implants Res. 2009; 20:99–108. PMID: 19126114.
Article20. Lindhe J, Meyle J. Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008; 35:282–285. PMID: 18724855.
Article21. Renvert S, Roos-Jansåker AM, Claffey N. Non-surgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol. 2008; 35(Suppl):305–315.
Article22. Persson GR, Samuelsson E, Lindahl C, Renvert S. Mechanical non-surgical treatment of peri-implantitis: a single-blinded randomized longitudinal clinical study. II. Microbiological results. J Clin Periodontol. 2010; 37:563–573. PMID: 20507380.
Article23. Esposito M, Grusovin MG, Worthington HV. Treatment of peri-implantitis: what interventions are effective? A Cochrane systematic review. Eur J Oral Implantology. 2012; 5(Suppl):S21–S41.24. Serino G, Turri A. Outcome of surgical treatment of peri-implantitis: results from a 2-year prospective clinical study in humans. Clin Oral Implants Res. 2011; 22:1214–1220. PMID: 21309860.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case report of nonsurgical treatment of maxillary anterior peri-implantitis
- Treatment of Peri-implantitis: Cases Report
- Risk factors of peri-implantitis: a narrative review
- Unusual bone regeneration following resective surgery and decontamination of peri-implantitis: a 6-year follow-up
- Full mouth rehabilitation in a patient with peri-implantitis: A case report