J Dent Rehabil Appl Sci.
2022 Sep;38(3):171-177. 10.14368/jdras.2022.38.3.171.
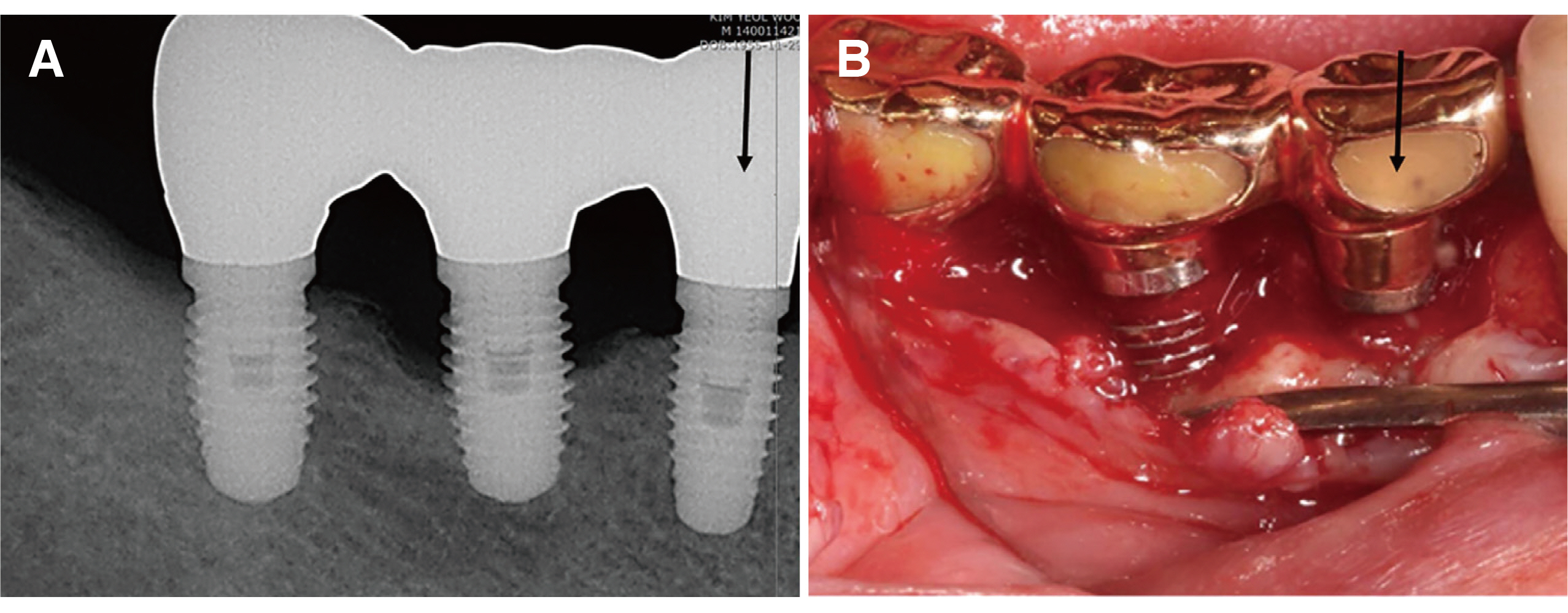
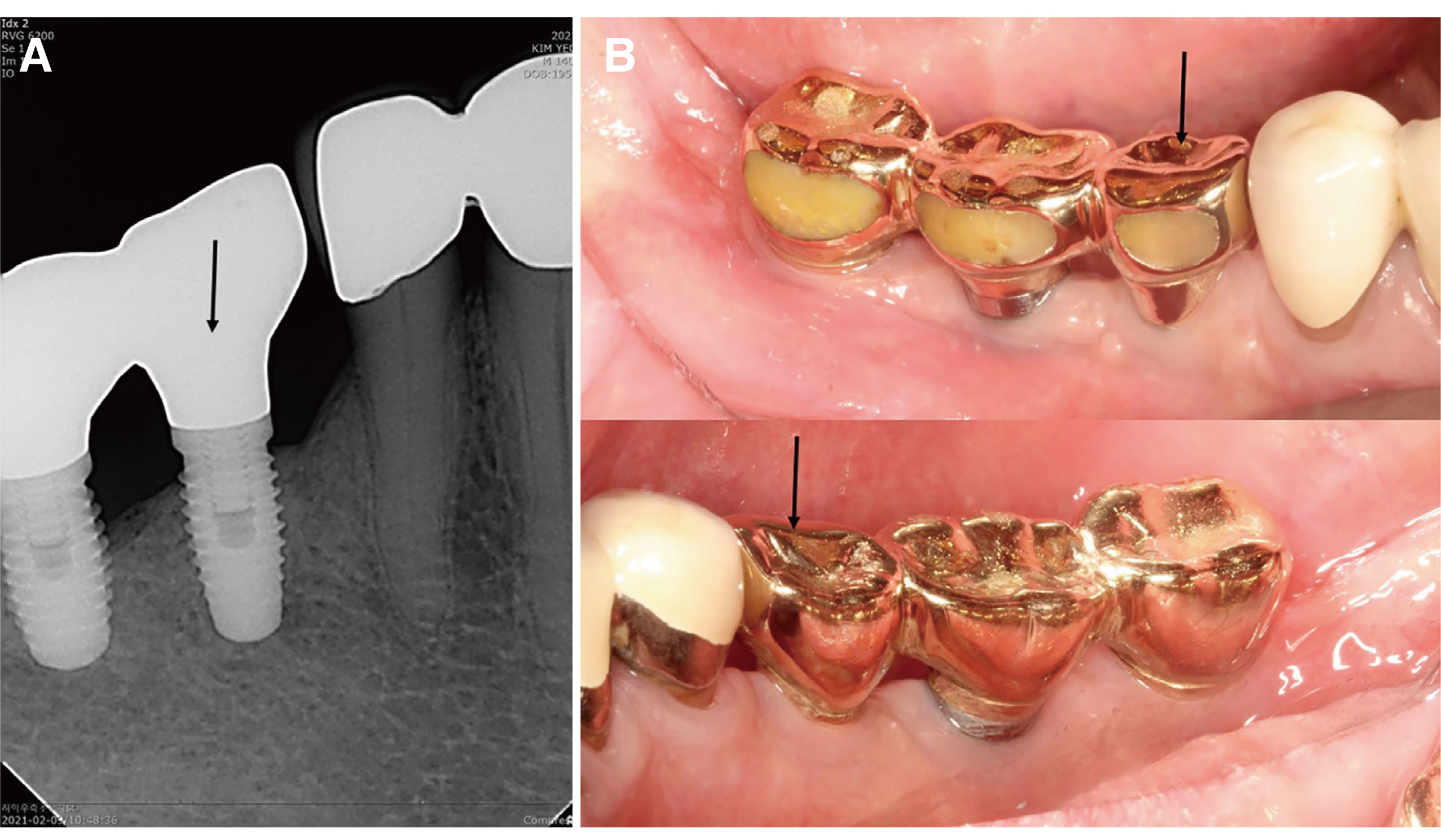
Unusual bone regeneration following resective surgery and decontamination of peri-implantitis: a 6-year follow-up
- Affiliations
-
- 1Department of Periodontology, School of Dentistry, Pusan National University, Yangsan, Republic of Korea
- KMID: 2535022
- DOI: http://doi.org/10.14368/jdras.2022.38.3.171
Abstract
- Peri-implantitis is an inflammatory lesion of the periodontium surrounding an endosseous implant, with progressive loss of the supporting peri-implant bone. The main purposes of treatment for peri-implantitis due to biological factors include addressing the inflammation and restoring a healthy but reduced periodontium around the implant, similar to the treatment of periodontitis in natural teeth. The proposed treatment protocol includes surgical treatment, mainly resective surgery, after non-surgical treatment such as oral hygiene instructions, mechanical cleansing of the fixture, and general or topical antiseptic or antibiotic application according to the extent of inflammation. In this article, we present a 6-year follow-up case showing unusual marginal bone regeneration after resective surgery and decontamination of an implant surface for the treatment of peri-implantitis and discuss the possible reasons.
Figure
Reference
-
References
1. Derks J, Schaller D, Håkansson J, Wennström JL, Tomasi C, Berglundh T. 2016; Effectiveness of implant therapy analyzed in a Swedish population: Prevalence of peri-implantitis. J Dent Res. 95:43–9. DOI: 10.1177/0022034515608832. PMID: 26701919.
Article2. Tawil G, Tawil P. 2019; Peri-implant infection concomitant with a flare-up episode of chronic periodontitis: An unusual regeneration following treatment and a 5-year follow-up. Int J Periodontics Restorative Dent. 39:415–21. DOI: 10.11607/prd.3940. PMID: 30986291.
Article3. Cho-Yan Lee J, Mattheos N, Nixon KC, Ivanovski S. 2012; Residual periodontal pockets are a risk indicator for peri-implantitis in patients treated for periodontitis. Clin Oral Implants Res. 23:325–33. DOI: 10.1111/j.1600-0501.2011.02264.x. PMID: 22092508.
Article4. Aljateeli M, Fu JH, Wang HL. 2012; Managing periimplant bone loss: Current understanding. Clin Implant Dent Relat Res. 14(Suppl 1):e109–18. DOI: 10.1111/j.1708-8208.2011.00387.x. PMID: 21985674.
Article5. Mombelli A, Lang NP. 1998; The diagnosis and treatment of peri-implantitis. Periodontol 2000. 17:63–76. DOI: 10.1111/j.1600-0757.1998.tb00124.x. PMID: 10337314.
Article6. Singh G, O'Neal RB, Brennan WA, Strong SL, Horner JA, Van Dyke TE. 1993; Surgical treatment of induced peri-implantitis in the micro pig: clinical and histological analysis. J Periodontol. 64:984–9. DOI: 10.1902/jop.1993.64.10.984. PMID: 8277409.
Article7. Kreisler M, Kohnen W, Christoffers AB, Götz H, Jansen B, Duschner H, d'Hoedt B. 2005; In vitro evaluation of the biocompatibility of contaminated implant surfaces treated with an Er : YAG laser and an air powder system. Clin Oral Implants Res. 16:36–43. DOI: 10.1111/j.1600-0501.2004.01056.x. PMID: 15642029.
Article8. Wetzel AC, Vlassis J, Caffesse RG, Hämmerle CH, Lang NP. 1999; Attempts to obtain re-osseointegration following experimental peri-implantitis in dogs. Clin Oral Implants Res. 10:111–9. DOI: 10.1034/j.1600-0501.1999.100205.x. PMID: 10219130.
Article9. Kornman KS, Robertson PB. 2000; Fundamental principles affecting the outcomes of therapy for osseous lesions. Periodontol 2000. 22:22–43. DOI: 10.1034/j.1600-0757.2000.2220103.x. PMID: 11276514.
Article10. Malizos KN, Papatheodorou LK. 2005; The healing potential of the periosteum molecular aspects. Injury. 36(Suppl 3):S13–9. DOI: 10.1016/j.injury.2005.07.030. PMID: 16188544.11. Sharma P, Williams R, Monaghan A. 2013; Spontaneous mandibular regeneration: another option for mandibular reconstruction in children? Br J Oral Maxillofac Surg. 51:e63–6. DOI: 10.1016/j.bjoms.2012.04.255. PMID: 22578705.
Article12. Ahmad O, Omami G. 2015; Self-regeneration of the mandible following hemimandibulectomy for ameloblastoma: a case report and review of literature. J Maxillofac Oral Surg. 14(Suppl 1):245–50. DOI: 10.1007/s12663-012-0462-7. PMID: 25861189. PMCID: PMC4379248.
Article13. Verdugo F, Simonian K, D'Addona A, Pontón J, Nowzari H. 2010; Human bone repair after mandibular symphysis block harvesting: A clinical and tomographic study. J Periodontol. 81:702–9. DOI: 10.1902/jop.2010.090612. PMID: 20429649.
Article14. Verdugo F, D'Addona A, Pontón J. 2012; Clinical, tomographic, and histological assessment of periosteal guided bone regeneration with cortical perforations in advanced human critical size defects. Clin Implant Dent Relat Res. 14:112–20. DOI: 10.1111/j.1708-8208.2009.00235.x. PMID: 20491815.
Article15. Botticelli D, Berglundh T, Buser D, Lindhe J. 2003; The jumping distance revisited: An experimental study in the dog. Clin Oral Implants Res. 14:35–42. DOI: 10.1034/j.1600-0501.2003.140105.x. PMID: 12562363.16. Botticelli D, Berglundh T, Buser D, Lindhe J. 2003; Appositional bone formation in marginal defects at implants. Clin Oral Implants Res. 14:1–9. DOI: 10.1034/j.1600-0501.2003.140101.x. PMID: 12562359.
Article17. Botticelli D, Berglundh T, Lindhe J. 2004; Resolution of bone defects of varying dimension and configuration in the marginal portion of the peri-implant bone. An experimental study in the dog. J Clin Periodontol. 31:309–17. DOI: 10.1111/j.1600-051X.2004.00502.x. PMID: 15016260.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Regenerative procedure using rotary titanium brush for surface decontamination of peri-implantitis: 3 cases with a 2-year follow-up
- Combined surgical therapy for the treatment of combined supraand intrabony defects in peri-implantitis
- In situ dental implant installation after decontamination in a previously peri-implant diseased site: a pilot study
- A case report of nonsurgical treatment of maxillary anterior peri-implantitis
- Laser therapy in peri-implantitis treatment: literature review