Brain Tumor Res Treat.
2018 Oct;6(2):101-104. 10.14791/btrt.2018.6.e18.
Pheochromocytoma with Brain Metastasis: A Extremely Rare Case in Worldwide
- Affiliations
-
- 1Department of Neurosurgery, Brain Tumor Center, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. seokgu9@gmail.com
- 2Department of Pathology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2423983
- DOI: http://doi.org/10.14791/btrt.2018.6.e18
Abstract
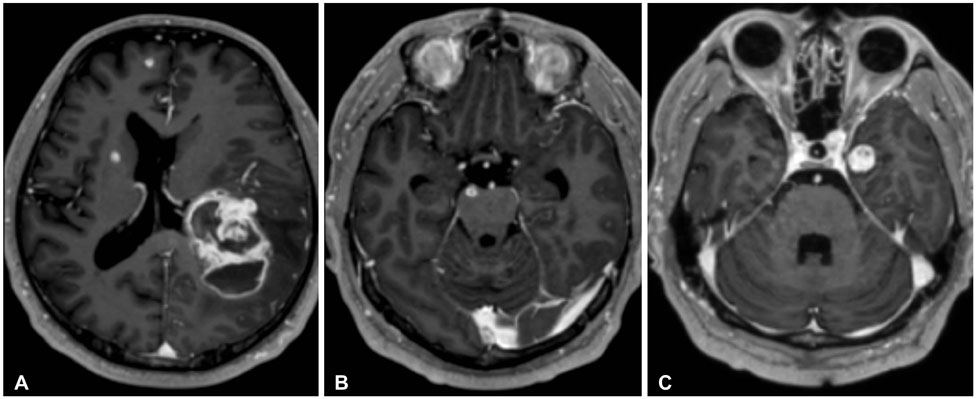
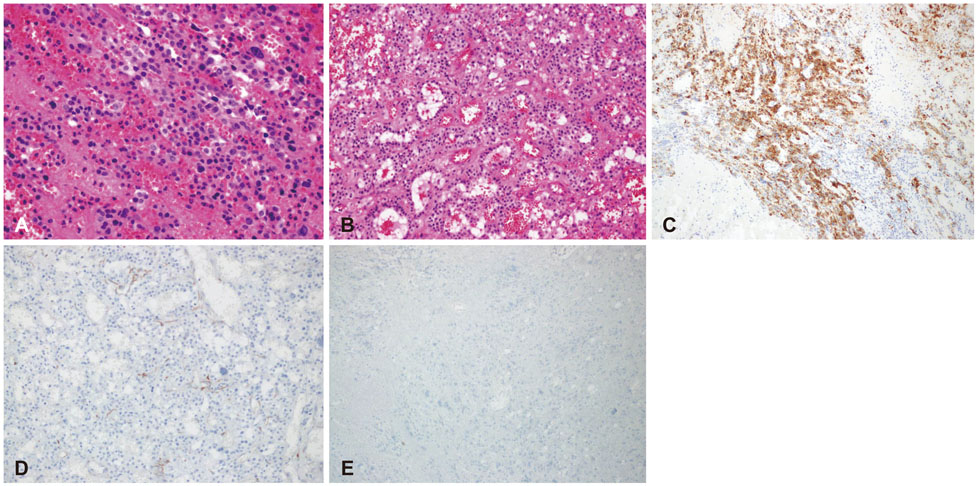
- Pheochromocytoma (PCC) is a neuroendocrine tumor that mainly arises from the medulla of the adrenal gland. Some PCCs become malignant and metastasize to other organs. For example, it typically involves skeletal system, liver, lung, and regional lymph nodes. However, only a few cases of PCC with brain metastasis have been reported worldwide. We report a case of metastatic brain tumor from PCC in South Korea in 2016. A 52-year-old man presented with headache, dizziness and motor aphasia. He had a medical history of PCC with multi-organ metastasis, previously underwent several operations, and was treated with chemotherapy and radiotherapy. Brain MRIs showed a brain tumor on the left parietal lobe. Postoperative pathology confirmed that the metastatic brain tumor derived from malignant PCC. This is the first report PCC with brain metastasis in South Korea.
Keyword
MeSH Terms
Figure
Reference
-
1. Mallory GW, Fang S, Giannini C, Van Gompel JJ, Parney IF. Brain carcinoid metastases: outcomes and prognostic factors. J Neurosurg. 2013; 118:889–895.
Article2. Hlatky R, Suki D, Sawaya R. Carcinoid metastasis to the brain. Cancer. 2004; 101:2605–2613.
Article3. Eisenhofer G, Bornstein SR, Brouwers FM, et al. Malignant pheochromocytoma: current status and initiatives for future progress. Endocr Relat Cancer. 2004; 11:423–436.
Article4. Thouënnon E, Elkahloun AG, Guillemot J, et al. Identification of potential gene markers and insights into the pathophysiology of pheochromocytoma malignancy. J Clin Endocrinol Metab. 2007; 92:4865–4872.
Article5. Ferrari G, Togni R, Pizzedaz C, Aldovini D. Cerebral metastases in pheochromocytoma. Pathologica. 1979; 71:703–710.6. Gentile S, Rainero I, Savi L, Rivoiro C, Pinessi L. Brain metastasis from pheochromocytoma in a patient with multiple endocrine neoplasia type 2A. Panminerva Med. 2001; 43:305–306.7. Melicow MM. One hundred cases of pheochromocytoma (107 tumors) at the Columbia-Presbyterian Medical Center, 1926–1976: a clinicopathological analysis. Cancer. 1977; 40:1987–2004.
Article8. Mornex R, Badet C, Peyrin L. Malignant pheochromocytoma: a series of 14 cases observed between 1966 and 1990. J Endocrinol Invest. 1992; 15:643–649.
Article9. Gimenez-Roqueplo AP, Favier J, Rustin P, et al. Mutations in the SDHB gene are associated with extra-adrenal and/or malignant phaeochromocytomas. Cancer Res. 2003; 63:5615–5621.10. Mannelli M, Lenders JW, Pacak K, Parenti G, Eisenhofer G. Subclinical phaeochromocytoma. Best Pract Res Clin Endocrinol Metab. 2012; 26:507–515.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Meningeal Pheochromocytoma: A Case Report
- A Case of Malignant Pheochromocytoma
- A Case of Pheochromocytoma Presented with Cardiogenic Shock and Followed by Spontaneous Remission
- Early Detection and Successful Laparoscopic Adrenalectomy for Pheochromocytoma in Pregnancy; A Case Report
- A Case of Adrenocortical Adenoma Associated with Incidental Pheochromocytoma