J Cerebrovasc Endovasc Neurosurg.
2018 Sep;20(3):168-175. 10.7461/jcen.2018.20.3.168.
Implications of Mechanical Endovascular Thrombectomy for Acute Basilar and Posterior Cerebral Artery Occlusion
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. sch.shin.ds@gmail.com
- KMID: 2422768
- DOI: http://doi.org/10.7461/jcen.2018.20.3.168
Abstract
OBJECTIVE
Protocols for posterior circulation ischemic stroke have not been established by randomized clinical trials. Mechanical endovascular thrombectomy (MET) devices are evolving, and many of these devices already developed or in development are suitable for posterior circulation MET.
MATERIALS AND METHODS
We investigated the medical records of patients who underwent MET for posterior circulation ischemic stroke from January 2012 to August 2016. Fifteen patients were included. MET was performed in patients with or without injected intravenous tissue plasminogen activator. MET was considered in patients with a National Institute of Health Stroke Scale score of 4 or more, older than 18 years, with definite occlusion of the basilar artery or posterior cerebral artery (PCA), and who arrived at the hospital within 24 hours from onset.
RESULTS
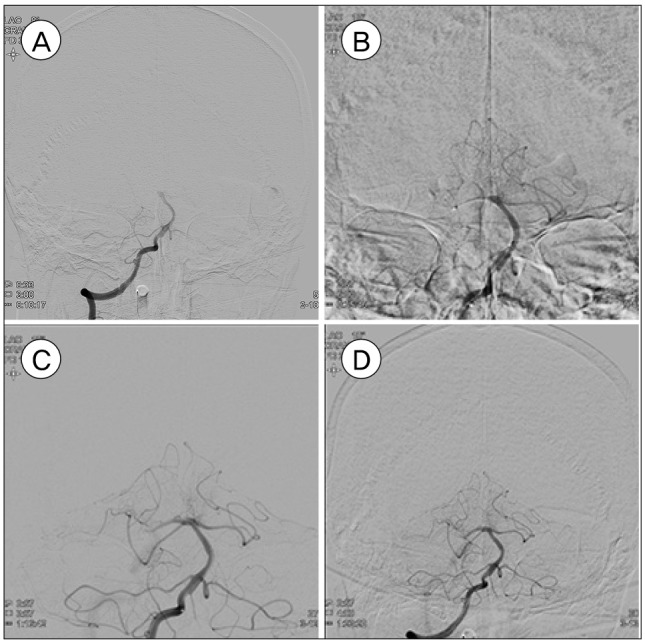
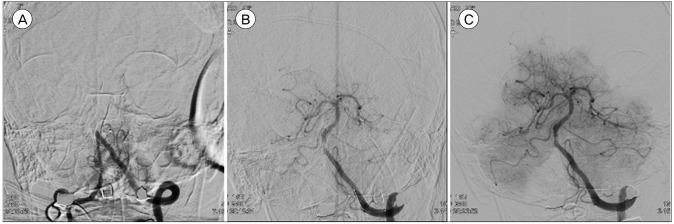
The direct catheter aspiration technique was used in five cases, and the stent retrieval technique was used in seven cases. The stent retrieval technique with the direct aspiration technique was used in three cases. Recanalization failed in two cases. Basilar occlusion without PCA involvement is the only effective factor of successful recanalization (p = 0.03). Successful recanalization (p = 0.005) and the presence of a posterior communicating artery (p = 0.005) affected the good outcome at discharge.
CONCLUSION
An early diagnosis and active MET may improve the patient outcome. MET may help recanalization and good flow restoration and the potential for a good outcome.
MeSH Terms
Figure
Reference
-
1. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 2. 378(8):708–718. PMID: 29364767.
Article2. Berkhemer OA, Fransen PS, Beumer D, Van Den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 1. 372(1):11–20. PMID: 25517348.3. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 3. 372(11):1009–1018. PMID: 25671797.
Article4. Chalela JA, Alsop DC, Gonzalez-Atavales JB, Maldjian JA, Kasner SE, Detre JA. Magnetic resonance perfusion imaging in acute ischemic stroke using continuous arterial spin labeling. Stroke. 2000; 3. 31(3):680–687. PMID: 10700504.
Article5. Cross DT 3rd, Moran CJ, Akins PT, Angtuaco EE, Derdeyn CP, Diringer MN. Collateral circulation and outcome after basilar artery thrombolysis. AJNR Am J Neuroradiol. 1998; 9. 19(8):1557–1563. PMID: 9763394.6. Furie KL, Jayaraman MV. 2018 guidelines for the early management of patients with acute ischemic stroke. Stroke. 2018; 3. 49(3):509–510. PMID: 29367335.
Article7. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 3. 372(11):1019–1030. PMID: 25671798.8. Grigoriadis S, Gomori JM, Grigoriadis N, Cohen JE. Clinically successful late recanalization of basilar artery occlusion in childhood: What are the odds?: case report and review of the literature. J Neurol Sci. 2007; 9. 260(1-2):256–260. PMID: 17482211.9. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 6. 372(24):2296–2306. PMID: 25882510.
Article10. Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. 2006; 3. 37(3):922–928. PMID: 16439705.11. Lindsberg PJ, Soinne L, Tatlisumak T, Roine RO, Kallela M, Häppölä O, et al. Long-term outcome after intravenous thrombolysis of basilar artery occlusion. JAMA. 2004; 10. 292(15):1862–1866. PMID: 15494584.
Article12. Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011; 11. 10(11):1002–1014. PMID: 22014435.
Article13. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 1. 378(1):11–21. PMID: 29129157.14. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 6. 372(24):2285–2295. PMID: 25882376.
Article15. Schomer DF, Marks MP, Steinberg GK, Johnstone IM, Boothroyd DB, Ross MR, et al. The anatomy of the posterior communicating artery as a risk factor for ischemic cerebral infarction. N Engl J Med. 1994; 6. 330(22):1565–1570. PMID: 8177246.
Article16. Tong D, Yenari M, Albers G, O'brien M, Marks M, Moseley M. Correlation of perfusion-and diffusion-weighted MRI with NIHSS score in acute (<6.5 hour) ischemic stroke. Neurology. 1998; 4. 50(4):864–870. PMID: 9566364.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dual Mechanical Thrombectomy for Recanalization of a Resistant Acute Posterior Circulation Stroke
- Acute Ischemic Stroke Involving Both Anterior and Posterior Circulation Treated by Endovascular Revascularization for Acute Basilar Artery Occlusion via Persistent Primitive Trigeminal Artery
- The Limitations of Thrombectomy with Solitaire(TM) AB as First-line Treatment in Acute Ischemic Stroke: A Single Center Experience
- Endovascular Mechanical Thrombectomy in Basilar Artery Occlusion: Initial Experience
- Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: A literature review