Yonsei Med J.
2018 Nov;59(9):1115-1122. 10.3349/ymj.2018.59.9.1115.
Biomechanical Properties of the Cornea Using a Dynamic Scheimpflug Analyzer in Healthy Eyes
- Affiliations
-
- 1Department of Ophthalmology, International St. Mary's Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea.
- 2The Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. tikim@yuhs.ac
- 3Eyereum Eye Clinic, Seoul, Korea.
- 4Corneal Dystrophy Research Institute, Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2422497
- DOI: http://doi.org/10.3349/ymj.2018.59.9.1115
Abstract
- PURPOSE
To investigate biomechanical properties of the cornea using a dynamic Scheimpflug analyzer according to age.
MATERIALS AND METHODS
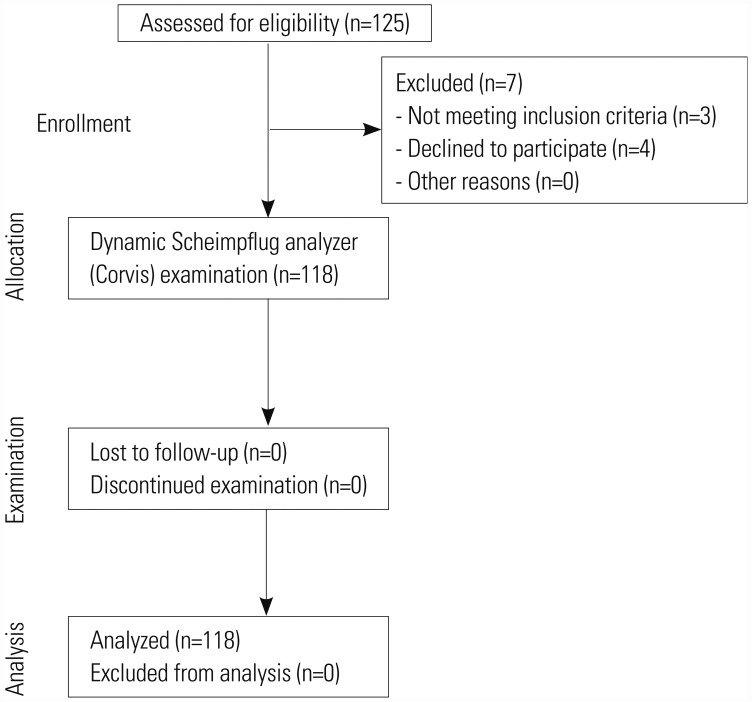
In this prospective, cross-sectional, observational study, participants underwent ophthalmic investigations including corneal biomechanical properties, keratometric values, intraocular pressure (IOP), and manifest refraction spherical equivalent (MRSE). We determined the relationship of biomechanical parameters and ocular/systemic variables (participant's age, MRSE, IOP, and mean keratometric values) by piecewise regression analysis, association of biomechanical parameters with variables by Spearman's correlation and stepwise multiple regression analyses, and reference intervals (RI) by the bootstrap method.
RESULTS
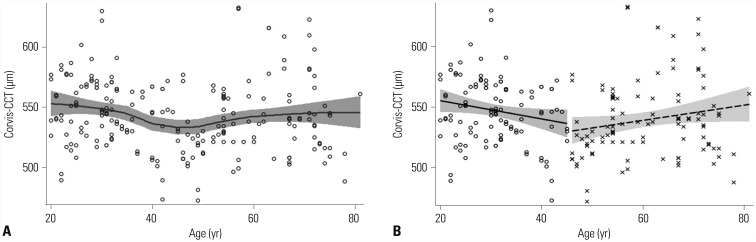
This study included 217 eyes of 118 participants (20-81 years of age). Piecewise regression analysis between Corvis-central corneal thickness (CCT) and participant's age revealed that the optimal cut-off value of age was 45 years. No clear breakpoints were detected between the corneal biomechanical parameters and MRSE, IOP, and mean keratometric values. Corneal velocity, deformation amplitude, radius, maximal concave power, Corvis-CCT, and Corvis-IOP exhibited correlations with IOP, regardless of age (all ages, 20-44 years, and over 44 years). With smaller deformation amplitude and corneal velocity as well as increased Corvis-IOP and Corvis-CCT, IOP became significantly increased. We provided the results of determination of confidence interval from RI data using bootstrap method in three separate age groups (all ages, 20-44 years, and over 44 years).
CONCLUSION
We demonstrated multiple corneal biomechanical parameters according to age, and reported that the corneal biomechanical parameters are influenced by IOP.
Figure
Reference
-
1. Soergel F, Jean B, Seiler T, Bende T, Mücke S, Pechhold W, et al. Dynamic mechanical spectroscopy of the cornea for measurement of its viscoelastic properties in vitro. Ger J Ophthalmol. 1995; 4:151–156. PMID: 7663327.2. Dupps WJ Jr, Wilson SE. Biomechanics and wound healing in the cornea. Exp Eye Res. 2006; 83:709–720. PMID: 16720023.
Article3. Lau W, Pye D. Changes in corneal biomechanics and applanation tonometry with induced corneal swelling. Invest Ophthalmol Vis Sci. 2011; 52:3207–3214. PMID: 21345994.
Article4. Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005; 31:146–155. PMID: 15721707.5. Wells AP, Garway-Heath DF, Poostchi A, Wong T, Chan KC, Sachdev N. Corneal hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patients. Invest Ophthalmol Vis Sci. 2008; 49:3262–3268. PMID: 18316697.
Article6. Schweitzer C, Roberts CJ, Mahmoud AM, Colin J, Maurice-Tison S, Kerautret J. Screening of forme fruste keratoconus with the ocular response analyzer. Invest Ophthalmol Vis Sci. 2010; 51:2403–2410. PMID: 19907025.
Article7. Roberts C. Biomechanics of the cornea and wavefront-guided laser refractive surgery. J Refract Surg. 2002; 18:S589–S592. PMID: 12361163.
Article8. Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005; 31:156–162. PMID: 15721708.
Article9. Kamiya K, Shimizu K, Ohmoto F. Comparison of the changes in corneal biomechanical properties after photorefractive keratectomy and laser in situ keratomileusis. Cornea. 2009; 28:765–769. PMID: 19574911.
Article10. Pepose JS, Feigenbaum SK, Qazi MA, Sanderson JP, Roberts CJ. Changes in corneal biomechanics and intraocular pressure following LASIK using static, dynamic, and noncontact tonometry. Am J Ophthalmol. 2007; 143:39–47. PMID: 17188041.
Article11. Narayanaswamy A, Chung RS, Wu RY, Park J, Wong WL, Saw SM, et al. Determinants of corneal biomechanical properties in an adult Chinese population. Ophthalmology. 2011; 118:1253–1259. PMID: 21333357.
Article12. Vinciguerra R, Elsheikh A, Roberts CJ, Ambrósio R Jr, Kang DS, Lopes BT, et al. Influence of pachymetry and intraocular pressure on dynamic corneal response parameters in healthy patients. J Refract Surg. 2016; 32:550–561. PMID: 27505316.
Article13. Shen Y, Chen Z, Knorz MC, Li M, Zhao J, Zhou X. Comparison of corneal deformation parameters after SMILE, LASEK, and femtosecond laser-assisted LASIK. J Refract Surg. 2014; 30:310–318. PMID: 24904933.
Article14. Hassan Z, Modis L Jr, Szalai E, Berta A, Nemeth G. Examination of ocular biomechanics with a new Scheimpflug technology after corneal refractive surgery. Cont Lens Anterior Eye. 2014; 37:337–341. PMID: 24894545.
Article15. Tomita M, Mita M, Huseynova T. Accelerated versus conventional corneal collagen crosslinking. J Cataract Refract Surg. 2014; 40:1013–1020. PMID: 24857442.
Article16. Vellara HR, Ali NQ, Gokul A, Turuwhenua J, Patel DV, McGhee CN. Quantitative analysis of corneal energy dissipation and corneal and orbital deformation in response to an air-pulse in healthy eyes. Invest Ophthalmol Vis Sci. 2015; 56:6941–6947. PMID: 26513499.
Article17. Valbon BF, Ambrósio R Jr, Fontes BM, Alves MR. Effects of age on corneal deformation by non-contact tonometry integrated with an ultra-high-speed (UHS) Scheimpflug camera. Arq Bras Oftalmol. 2013; 76:229–232. PMID: 24061834.
Article18. Lee H, Kang DS, Ha BJ, Choi JY, Kim EK, Seo KY, et al. Biomechanical properties of the cornea measured with the dynamic Scheimpflug analyzer in young healthy adults. Cornea. 2017; 36:53–58. PMID: 27560031.
Article19. Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, et al. The Lens Opacities Classification System III. The longitudinal study of cataract study group. Arch Ophthalmol. 1993; 111:831–836. PMID: 8512486.20. Sahin A, Bayer A, Ozge G, Mumcuogğlu T. Corneal biomechanical changes in diabetes mellitus and their influence on intraocular pressure measurements. Invest Ophthalmol Vis Sci. 2009; 50:4597–4604. PMID: 19443722.
Article21. Kotecha A, Oddone F, Sinapis C, Elsheikh A, Sinapis D, Sinapis A, et al. Corneal biomechanical characteristics in patients with diabetes mellitus. J Cataract Refract Surg. 2010; 36:1822–1828. PMID: 21029887.
Article22. Zhong Y, Shen X, Yu J, Tan H, Cheng Y. The comparison of the effects of latanoprost, travoprost, and bimatoprost on central corneal thickness. Cornea. 2011; 30:861–864. PMID: 21499083.
Article23. Koprowski R. Automatic method of analysis and measurement of additional parameters of corneal deformation in the Corvis tonometer. Biomed Eng Online. 2014; 13:150. PMID: 25406740.
Article24. Shen Y, Zhao J, Yao P, Miao H, Niu L, Wang X, et al. Changes in corneal deformation parameters after lenticule creation and extraction during small incision lenticule extraction (SMILE) procedure. PLoS One. 2014; 9:e103893. PMID: 25121508.
Article25. Hon Y, Lam AK. Corneal deformation measurement using Scheimpflug noncontact tonometry. Optom Vis Sci. 2013; 90:e1–e8. PMID: 23238261.
Article26. Naumova EN, Must A, Laird NM. Tutorial in biostatistics: evaluating the impact of ‘critical periods’ in longitudinal studies of growth using piecewise mixed effects models. Int J Epidemiol. 2001; 30:1332–1341. PMID: 11821342.
Article27. Ryan SE, Porth LS. A tutorial on the piecewise regression approach applied to bedload transport data. Fort Collins (CO): US Department of Agriculture, Forest Service, Rocky Mountain Research Station;2007.28. Friedrichs KR, Harr KE, Freeman KP, Szladovits B, Walton RM, Barnhart KF, et al. ASVCP reference interval guidelines: determination of de novo reference intervals in veterinary species and other related topics. Vet Clin Pathol. 2012; 41:441–453. PMID: 23240820.
Article29. Horowitz GL, Altaie S, Boyd JC, Ceriotti F, Garg U, Horn P, et al. Defining, establishing, and verifying reference intervals in the clinical laboratory; approved guidelines. CLSI document C28-A3. 3rd ed. Wayne (PA): Clinical and Laboratory Standards Institute;2008.30. Valbon BF, Ambrósio R Jr, Fontes BM, Luz A, Roberts CJ, Alves MR. Ocular biomechanical metrics by CorVis ST in healthy Brazilian patients. J Refract Surg. 2014; 30:468–473. PMID: 24877553.
Article31. Bak-Nielsen S, Pedersen IB, Ivarsen A, Hjortdal J. Dynamic Scheimpflug-based assessment of keratoconus and the effects of corneal cross-linking. J Refract Surg. 2014; 30:408–414. PMID: 24972407.
Article32. Huseynova T, Waring GO 4th, Roberts C, Krueger RR, Tomita M. Corneal biomechanics as a function of intraocular pressure and pachymetry by dynamic infrared signal and Scheimpflug imaging analysis in normal eyes. Am J Ophthalmol. 2014; 157:885–893. PMID: 24388837.
Article33. Asaoka R, Nakakura S, Tabuchi H, Murata H, Nakao Y, Ihara N, et al. The relationship between Corvis ST tonometry measured corneal parameters and intraocular pressure, corneal thickness and corneal curvature. PLoS One. 2015; 10:e0140385. PMID: 26485129.
Article34. Kotecha A, Russell RA, Sinapis A, Pourjavan S, Sinapis D, Garway-Heath DF. Biomechanical parameters of the cornea measured with the Ocular Response Analyzer in normal eyes. BMC Ophthalmol. 2014; 14:11. PMID: 24479520.
Article35. Knox Cartwright NE, Tyrer JR, Marshall J. Age-related differences in the elasticity of the human cornea. Invest Ophthalmol Vis Sci. 2011; 52:4324–4329. PMID: 20847118.
Article36. Elsheikh A, Wang D, Brown M, Rama P, Campanelli M, Pye D. Assessment of corneal biomechanical properties and their variation with age. Curr Eye Res. 2007; 32:11–19. PMID: 17364730.
Article37. Daxer A, Misof K, Grabner B, Ettl A, Fratzl P. Collagen fibrils in the human corneal stroma: structure and aging. Invest Ophthalmol Vis Sci. 1998; 39:644–648. PMID: 9501878.38. Ortiz D, Piñero D, Shabayek MH, Arnalich-Montiel F, Alió JL. Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. J Cataract Refract Surg. 2007; 33:1371–1375. PMID: 17662426.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Use of a Dynamic Scheimpflug Analyzer to Measure Changes of Post-keratoplasty Corneal Biomechanical Properties
- Change in Corneal Biomechanical Parameters in Diabetes Mellitus
- Corneal Biomechanical Properties of Normal Tension Glaucoma in Young Patients Evaluated with the Ocular Response Analyzer
- Comparison of Anterior, Posterior, and Total Corneal Astigmatism Measured Using a Single Scheimpflug Camera in Healthy and Keratoconus Eyes
- Evaluation of Corneal Biomechanical Properties Following Penetrating Keratoplasty Using the Ocular Response Analyzer