Diabetes Metab J.
2018 Aug;42(4):308-319. 10.4093/dmj.2017.0076.
The Changes of Trends in the Diagnosis and Treatment of Diabetic Foot Ulcer over a 10-Year Period: Single Center Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea. helee@ynu.ac.kr
- 2Department of Nuclear Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- 3Department of Orthopedic Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- 4Division of Vascular Surgery, Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- 5Department of Plastic Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- 6Division of Cardiology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- KMID: 2418719
- DOI: http://doi.org/10.4093/dmj.2017.0076
Abstract
- BACKGROUND
This study aims to describe the trends in the severity and treatment modality of patients with diabetic foot ulcer (DFU) at a single tertiary referral center in Korea over the last 10 years and compare the outcomes before and after the introduction of a multidisciplinary diabetic foot team.
METHODS
In this retrospective observational study, electronic medical records of patients from years 2002 to 2015 at single tertiary referral center were reviewed. Based on the year of first admission, patients were assigned to a group either before or after the year 2012, the year the diabetes team launched.
RESULTS
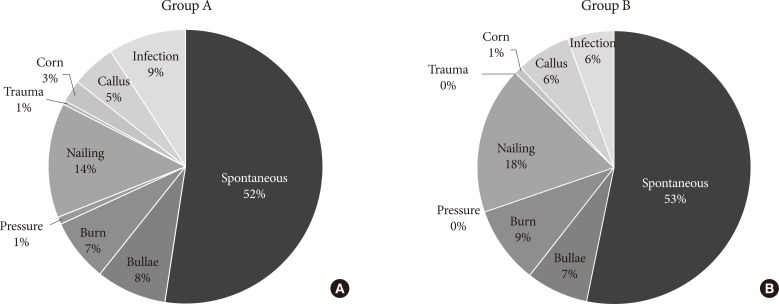
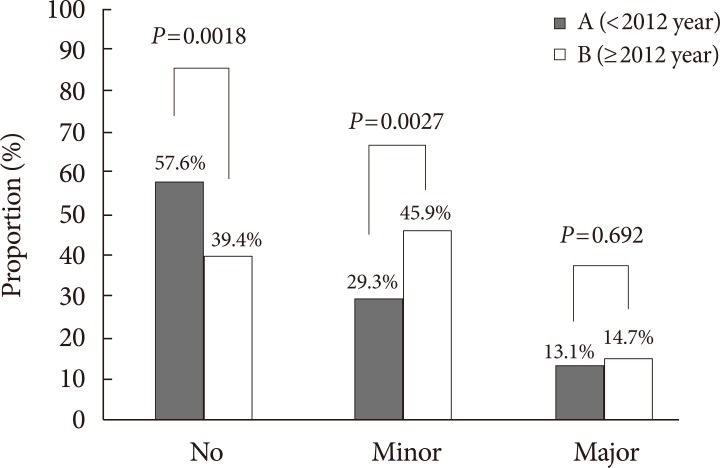
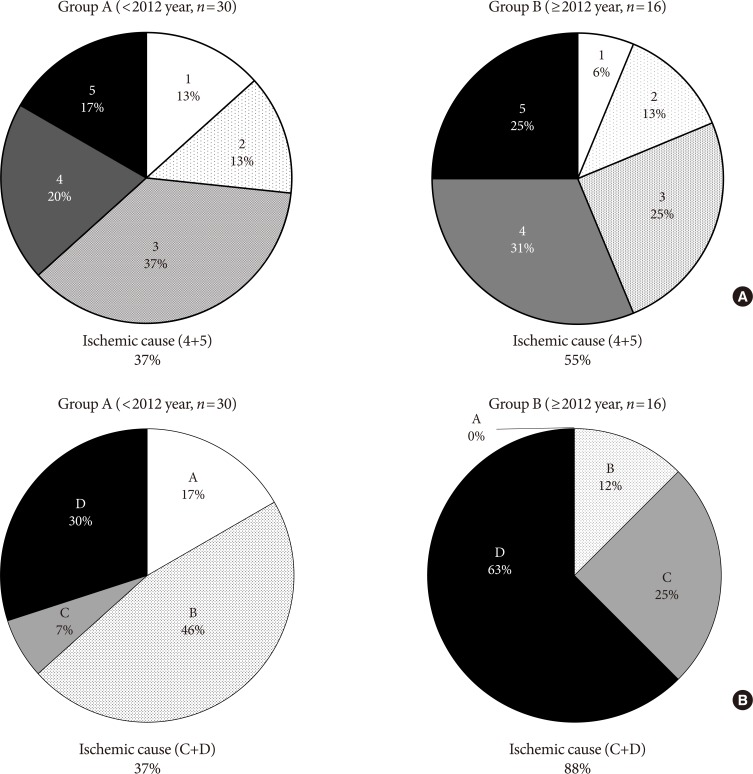
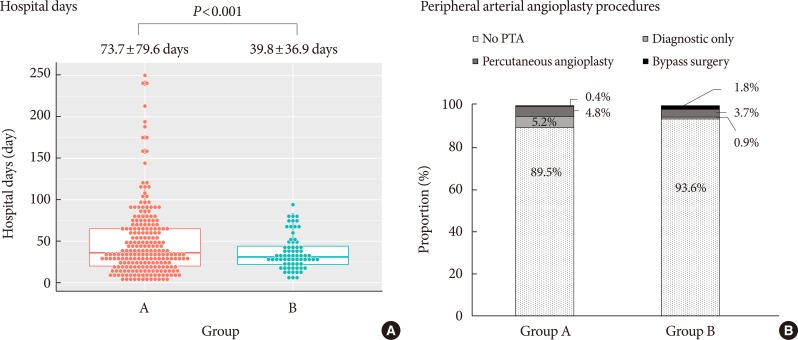
Of the 338 patients with DFU, 229 were first admitted until the year 2011 (group A), while 109 were first admitted since the year 2012 (group B). Mean age was higher in group B, and ulcer size was larger than those of group A. Whereas duration of diabetes was longer in group B, glycemic control was improved (mean glycosylated hemoglobin, 9.48% vs. 8.50%). The proportion of minor lower extremity amputation (LEA) was increased, but length of hospital stay was decreased (73.7±79.6 days vs. 39.8±36.9 days). As critical ischemic limb increased, the proportion of major LEA was not decreased.
CONCLUSION
Improved glycemic control, multidisciplinary strategies with prompt surgical treatment resulted in reduced length of hospital stay, but these measures did not reduce major LEAs. The increase in critical ischemic limb may have played a role in the unexpected outcome, and may suggest the need for increased vascular intervention strategies in DFU treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Bakker K, Schaper NC. International Working Group on Diabetic Foot Editorial Board. The development of global consensus guidelines on the management and prevention of the diabetic foot 2011. Diabetes Metab Res Rev. 2012; 28(Suppl 1):116–118. PMID: 22271736.
Article2. Brem H, Sheehan P, Boulton AJ. Protocol for treatment of diabetic foot ulcers. Am J Surg. 2004; 187:1S–10S. PMID: 15147985.
Article3. Apelqvist J, Bakker K, van Houtum WH, Schaper NC. International Working Group on the Diabetic Foot (IWGDF) Editorial Board. Practical guidelines on the management and prevention of the diabetic foot: based upon the International Consensus on the Diabetic Foot (2007) Prepared by the International Working Group on the Diabetic Foot. Diabetes Metab Res Rev. 2008; 24(Suppl 1):S181–S187. PMID: 18442189.4. Noor S, Khan RU, Ahmad J. Understanding diabetic foot infection and its management. Diabetes Metab Syndr. 2017; 11:149–156. PMID: 27377687.
Article5. Vileikyte L. Diabetic foot ulcers: a quality of life issue. Diabetes Metab Res Rev. 2001; 17:246–249. PMID: 11544609.
Article6. Resnick HE, Carter EA, Sosenko JM, Henly SJ, Fabsitz RR, Ness FK, Welty TK, Lee ET, Howard BV. Strong Heart Study. Incidence of lower-extremity amputation in American Indians: the Strong Heart Study. Diabetes Care. 2004; 27:1885–1891. PMID: 15277412.7. Lehto S, Ronnemaa T, Pyorala K, Laakso M. Risk factors predicting lower extremity amputations in patients with NIDDM. Diabetes Care. 1996; 19:607–612. PMID: 8725860.
Article8. Jørgensen ME, Almdal TP, Faerch K. Reduced incidence of lower-extremity amputations in a Danish diabetes population from 2000 to 2011. Diabet Med. 2014; 31:443–447. PMID: 24111834.
Article9. Holstein P, Ellitsgaard N, Olsen BB, Ellitsgaard V. Decreasing incidence of major amputations in people with diabetes. Diabetologia. 2000; 43:844–847. PMID: 10952455.
Article10. Krishnan S, Nash F, Baker N, Fowler D, Rayman G. Reduction in diabetic amputations over 11 years in a defined U.K. population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care. 2008; 31:99–101. PMID: 17934144.11. Feng Y, Schlosser FJ, Sumpio BE. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg. 2009; 50:675–682. PMID: 19595541.
Article12. Moghtaderi A, Bakhshipour A, Rashidi H. Validation of Michigan neuropathy screening instrument for diabetic peripheral neuropathy. Clin Neurol Neurosurg. 2006; 108:477–481. PMID: 16150538.
Article13. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002; 39(2 Suppl 1):S1–S266. PMID: 11904577.14. Oyibo SO, Jude EB, Tarawneh I, Nguyen HC, Harkless LB, Boulton AJ. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems. Diabetes Care. 2001; 24:84–88. PMID: 11194247.15. Kennon B, Leese GP, Cochrane L, Colhoun H, Wild S, Stang D, Sattar N, Pearson D, Lindsay RS, Morris AD, Livingstone S, Young M, McKnight J, Cunningham S. Reduced incidence of lower-extremity amputations in people with diabetes in Scotland: a nationwide study. Diabetes Care. 2012; 35:2588–2590. PMID: 23011727.16. Sorensen BM, Houben AJ, Berendschot TT, Schouten JS, Kroon AA, van der Kallen CJ, Henry RM, Koster A, Sep SJ, Dagnelie PC, Schaper NC, Schram MT, Stehouwer CD. Prediabetes and type 2 diabetes are associated with generalized microvascular dysfunction: the Maastricht Study. Circulation. 2016; 134:1339–1352. PMID: 27678264.17. Keymel S, Heinen Y, Balzer J, Rassaf T, Kelm M, Lauer T, Heiss C. Characterization of macro-and microvascular function and structure in patients with type 2 diabetes mellitus. Am J Cardiovasc Dis. 2011; 1:68–75. PMID: 22254187.18. Nather A, Wong KL. Distal amputations for the diabetic foot. Diabet Foot Ankle. 2013; 4.
Article19. Quigley M, Dillon MP, Duke EJ. Comparison of quality of life in people with partial foot and transtibial amputation: a pilot study. Prosthet Orthot Int. 2016; 40:467–474. PMID: 25716956.20. Gauthier-Gagnon C, Grise MC, Potvin D. Enabling factors related to prosthetic use by people with transtibial and transfemoral amputation. Arch Phys Med Rehabil. 1999; 80:706–713. PMID: 10378500.
Article21. Gurlek A, Bayraktar M, Savas C, Gedik O. Amputation rate in 147 Turkish patients with diabetic foot: the Hacettepe University Hospital experience. Exp Clin Endocrinol Diabetes. 1998; 106:404–409. PMID: 9831306.22. Svensson H, Apelqvist J, Larsson J, Lindholm E, Eneroth M. Minor amputation in patients with diabetes mellitus and severe foot ulcers achieves good outcomes. J Wound Care. 2011; 20:261–262. PMID: 21727875.
Article23. Evans KK, Attinger CE, Al-Attar A, Salgado C, Chu CK, Mardini S, Neville R. The importance of limb preservation in the diabetic population. J Diabetes Complications. 2011; 25:227–231. PMID: 21447444.
Article24. Park IB, Baik SH. Epidemiologic characteristics of diabetes mellitus in Korea: current status of diabetic patients using Korean Health Insurance Database. Korean Diabetes J. 2009; 33:357–362.
Article25. Park SA, Ko SH, Lee SH, Cho JH, Moon SD, Jang SA, Son HS, Song KH, Cha BY, Son HY, Ahn YB. Incidence of diabetic foot and associated risk factors in type 2 diabetic patients: a five-year observational study. Korean Diabetes J. 2009; 33:315–323.
Article26. Kim JY, Lee KT, Young KW, Hwang SK. A clinical study on the diabetic foot wound. J Korean Diabetes Assoc. 2007; 31:89–95.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Management of Diabetic Foot
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Diabetic Foot Ulcer Recording Form Incorporating the Concepts of Wound Care and Treatment Plan
- Amputation in Diabetic Foot Ulcer and Infection
- Prevention and Education for Diabetic Foot