Intest Res.
2018 Jul;16(3):489-493. 10.5217/ir.2018.16.3.489.
Enteric infections complicating ulcerative colitis
- Affiliations
-
- 1Section of Gastroenterology, Hepatology and Nutrition, Department of Internal Medicine, University of Chicago, Chicago, IL, USA. dmicic@medicine.bsd.uchicago.edu
- 2Department of Pathology, University of Chicago, Chicago, IL, USA.
- KMID: 2417662
- DOI: http://doi.org/10.5217/ir.2018.16.3.489
Abstract
- Enteric infections have previously been postulated to play a role in the pathogenesis of inflammatory bowel disease (IBD), however, little evidence exists in the etiologic role of specific enteric infections in the development of IBD. When encountered in the setting of IBD, enteric infections pose a clinical challenge in management given the competing treatment strategies for infectious conditions and autoimmune disorders. Here we present the case of a young male with enteric infections complicating a new diagnosis of IBD. Our patient's initial clinical presentation included diagnoses of Klebsiella oxytoca isolation and Clostridium difficile infection. Directed therapies to include withdrawal of antibiotics and fecal microbiota transplantation were performed without resolution of clinical symptoms. Given persistence of symptoms and active colitis, the patient was diagnosed with ulcerative colitis (UC), requiring treatments directed at severe UC to include cyclosporine therapy. The finding of multiple enteric infections in a newly presenting patient with IBD is an unexpected finding that has treatment implications.
MeSH Terms
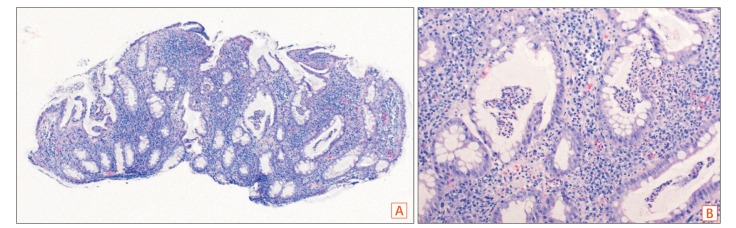
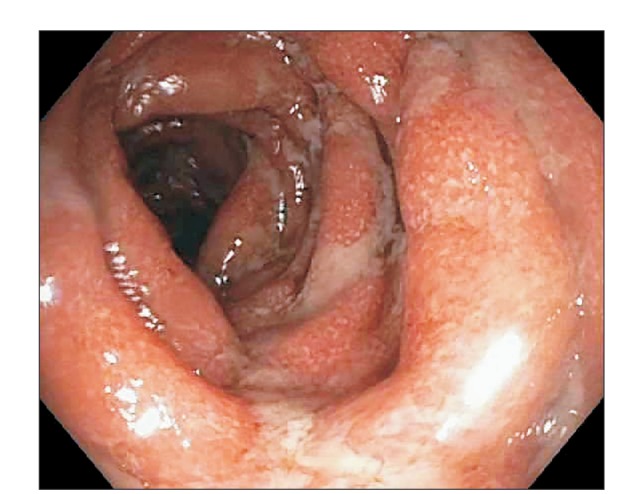
Figure
Cited by 1 articles
-
Usefulness of Stool Multiplex Polymerase Chain Reaction Assays in Patients with Acute Diarrhea
Seo Hyun Kim, You Sun Kim, Seung Hyuk Kim, Won Eui Yoon, Hee Jun Myung, Jeong Seop Moon, Dong Hee Whang
Korean J Gastroenterol. 2022;79(3):118-125. doi: 10.4166/kjg.2022.011.
Reference
-
1. Beaugerie L, Svrcek M, Seksik P, et al. Risk of colorectal high-grade dysplasia and cancer in a prospective observational cohort of patients with inflammatory bowel disease. Gastroenterology. 2013; 145:166–175.e8. PMID: 23541909.
Article2. Meyer AM, Ramzan NN, Loftus EV Jr, Heigh RI, Leighton JA. The diagnostic yield of stool pathogen studies during relapses of inflammatory bowel disease. J Clin Gastroenterol. 2004; 38:772–775. PMID: 15365403.
Article3. Jess T, Simonsen J, Nielsen NM, et al. Enteric Salmonella or Campylobacter infections and the risk of inflammatory bowel disease. Gut. 2011; 60:318–324. PMID: 21193449.
Article4. Pola S, Patel D, Ramamoorthy S, et al. Strategies for the care of adults hospitalized for active ulcerative colitis. Clin Gastroenterol Hepatol. 2012; 10:1315–1325.e4. PMID: 22835577.
Article5. Sartor RB. Microbial influences in inflammatory bowel diseases. Gastroenterology. 2008; 134:577–594. PMID: 18242222.
Article6. Schulfer AF, Battaglia T, Alvarez Y, et al. Intergenerational transfer of antibiotic-perturbed microbiota enhances colitis in susceptible mice. Nat Microbiol. 2018; 3:234–242. PMID: 29180726.
Article7. Ungaro R, Bernstein CN, Gearry R, et al. Antibiotics associated with increased risk of new-onset Crohn's disease but not ulcerative colitis: a meta-analysis. Am J Gastroenterol. 2014; 109:1728–1738. PMID: 25223575.
Article8. Högenauer C, Langner C, Beubler E, et al. Klebsiella oxytoca as a causative organism of antibiotic-associated hemorrhagic colitis. N Engl J Med. 2006; 355:2418–2426. PMID: 17151365.
Article9. Zollner-Schwetz I, Högenauer C, Joainig M, et al. Role of Klebsiella oxytoca in antibiotic-associated diarrhea. Clin Infect Dis. 2008; 47:e74–e78. DOI: 10.1086/592074. PMID: 18808355.10. Sweetser S, Schroeder KW, Pardi DS. Pseudomembranous colitis secondary to Klebsiella oxytoca. Am J Gastroenterol. 2009; 104:2366–2368. PMID: 19727105.
Article11. Plessier A, Cosnes J, Gendre JP, Beaugerie L. Intercurrent Klebsiella oxytoca colitis in a patient with Crohn's disease. Gastroenterol Clin Biol. 2002; 26:799–800. PMID: 12434087.12. Zollner-Schwetz I, Herzog KA, Feierl G, et al. The toxin-producing pathobiont Klebsiella oxytoca is not associated with flares of inflammatory bowel diseases. Dig Dis Sci. 2015; 60:3393–3398. PMID: 26091802.
Article13. Aroniadis OC, Brandt LJ, Greenberg A, et al. Long-term follow-up study of fecal microbiota transplantation for severe and/or complicated Clostridium difficile infection: a multicenter experience. J Clin Gastroenterol. 2016; 50:398–402. PMID: 26125460.
Article14. Jodorkovsky D, Young Y, Abreu MT. Clinical outcomes of patients with ulcerative colitis and co-existing Clostridium difficile infection. Dig Dis Sci. 2010; 55:415–420. PMID: 19255850.
Article15. Trnka YM, LaMont JT. Association of Clostridium difficile toxin with symptomatic relapse of chronic inflammatory bowel disease. Gastroenterology. 1981; 80:693–696. PMID: 7202941.
Article16. Meyers S, Mayer L, Bottone E, Desmond E, Janowitz HD. Occurrence of Clostridium difficile toxin during the course of inflammatory bowel disease. Gastroenterology. 1981; 80:697–670. PMID: 7202942.
Article17. Clayton EM, Rea MC, Shanahan F, et al. The vexed relationship between Clostridium difficile and inflammatory bowel disease: an assessment of carriage in an outpatient setting among patients in remission. Am J Gastroenterol. 2009; 104:1162–1169. PMID: 19319128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Appendiceal Orifice Inflammation in an 8-Year-Old Girl with Ulcerative Colitis Complicating Wilson's Disease
- A Case of Non-Hodgkin's Lymphoma in Ulcerative Colitis
- A case of ulcerative colitis
- Cytomegalovirus Colitis with Ulcerative Colitis in the Steroid Naive Immunocompetent Patient
- A Case of Cytomegalvirus Colitis Developed during the Treatment of Ulcerative Colitis