Tuberc Respir Dis.
2018 Jul;81(3):247-255. 10.4046/trd.2017.0126.
Predicting Mortality in Patients with Tuberculous Destroyed Lung Receiving Mechanical Ventilation
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. jubilate@pusan.ac.kr
- KMID: 2414568
- DOI: http://doi.org/10.4046/trd.2017.0126
Abstract
- BACKGROUND
Patients with acute respiratory failure secondary to tuberculous destroyed lung (TDL) have a poor prognosis. The aim of the present retrospective study was to develop a mortality prediction model for TDL patients who require mechanical ventilation.
METHODS
Data from consecutive TDL patients who had received mechanical ventilation at a single university-affiliated tertiary care hospital in Korea were reviewed. Binary logistic regression was used to identify factors predicting intensive care unit (ICU) mortality. A TDL on mechanical Ventilation (TDL-Vent) score was calculated by assigning points to variables according to β coefficient values.
RESULTS
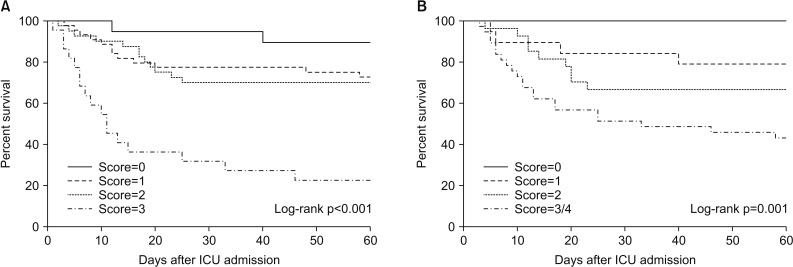
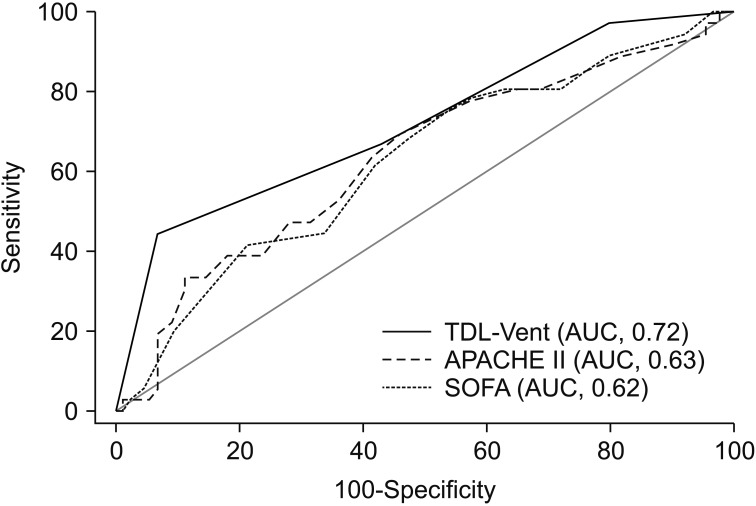
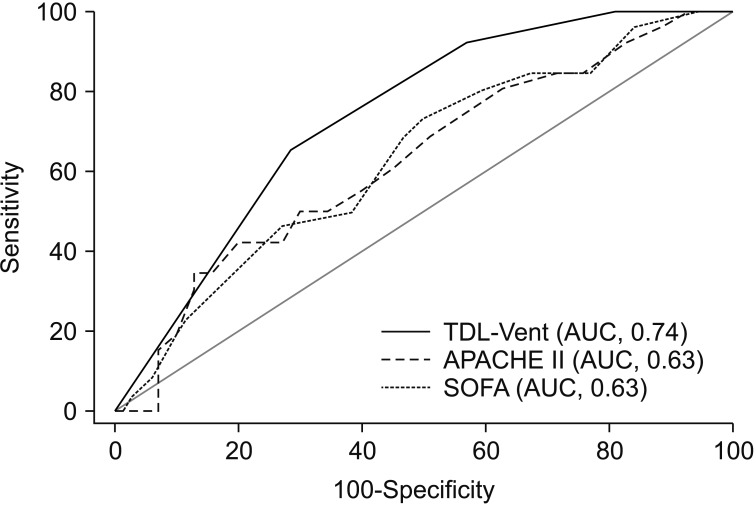
Data from 125 patients were reviewed. A total of 36 patients (29%) died during ICU admission. On the basis of multivariate analysis, the following factors were included in the TDL-Vent score: age ≥65 years, vasopressor use, and arterial partial pressure of oxygen/fraction of inspired oxygen ratio <180. In a second regression model, a modified score was then calculated by adding brain natriuretic peptide. For TDL-Vent scores 0 to 3, the 60-day mortality rates were 11%, 27%, 30%, and 77%, respectively (p<0.001). For modified TDL-Vent scores 0 to ≥3, the 60-day mortality rates were 0%, 21%, 33%, and 57%, respectively (p=0.001). For both the TDL-Vent score and the modified TDL-Vent score, the areas under the receiver operating characteristic curve were larger than that of other illness severity scores.
CONCLUSION
The TDL-Vent model identifies TDL patients on mechanical ventilation with a high risk of mortality. Prospective validation studies in larger cohorts are now warranted.
Keyword
MeSH Terms
-
Cohort Studies
Humans
Intensive Care Units
Korea
Logistic Models
Lung*
Mortality*
Multivariate Analysis
Natriuretic Peptide, Brain
Oxygen
Partial Pressure
Prognosis
Prospective Studies
Respiration, Artificial*
Respiratory Insufficiency
Retrospective Studies
ROC Curve
Tertiary Healthcare
Tuberculosis
Natriuretic Peptide, Brain
Oxygen
Figure
Reference
-
1. Bobrowitz ID, Rodescu D, Marcus H, Abeles H. The destroyed tuberculous lung. Scand J Respir Dis. 1974; 55:82–88. PMID: 4854707.2. Park JH, Na JO, Kim EK, Lim CM, Shim TS, Lee SD, et al. The prognosis of respiratory failure in patients with tuberculous destroyed lung. Int J Tuberc Lung Dis. 2001; 5:963–967. PMID: 11605892.3. Ryu YJ, Koh WJ, Kang EH, Suh GY, Chung MP, Kim H, et al. Prognostic factors in pulmonary tuberculosis requiring mechanical ventilation for acute respiratory failure. Respirology. 2007; 12:406–411. PMID: 17539846.
Article4. Ryu YJ, Lee JH, Chun EM, Chang JH, Shim SS. Clinical outcomes and prognostic factors in patients with tuberculous destroyed lung. Int J Tuberc Lung Dis. 2011; 15:246–250. PMID: 21219689.5. Chakhaia T, Magee MJ, Kempker RR, Gegia M, Goginashvili L, Nanava U, et al. High utility of contact investigation for latent and active tuberculosis case detection among the contacts: a retrospective cohort study in Tbilisi, Georgia, 2010–2011. PLoS One. 2014; 9:e111773. PMID: 25379809.
Article6. Calligaro GL, Theron G, Khalfey H, Peter J, Meldau R, Matinyenya B, et al. Burden of tuberculosis in intensive care units in Cape Town, South Africa, and assessment of the accuracy and effect on patient outcomes of the Xpert MTB/RIF test on tracheal aspirate samples for diagnosis of pulmonary tuberculosis: a prospective burden of disease study with a nested randomised controlled trial. Lancet Respir Med. 2015; 3:621–630. PMID: 26208996.
Article7. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–829. PMID: 3928249.8. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–710. PMID: 8844239.9. Wong KT, Antonio GE, Hui DS, Lee N, Yuen EH, Wu A, et al. Severe acute respiratory syndrome: radiographic appearances and pattern of progression in 138 patients. Radiology. 2003; 228:401–406. PMID: 12759474.
Article10. Muller NL, Ooi GC, Khong PL, Nicolaou S. Severe acute respiratory syndrome: radiographic and CT findings. AJR Am J Roentgenol. 2003; 181:3–8. PMID: 12818821.11. Choi JK, Paek D, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis. 2005; 58:230–242.
Article13. Arcasoy SM, Christie JD, Ferrari VA, Sutton MS, Zisman DA, Blumenthal NP, et al. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Respir Crit Care Med. 2003; 167:735–740. PMID: 12480614.
Article14. Cleveland WS, Grosse E, Shyu WM. Local regression models. In : Chambers JM, Hastie TJ, editors. Statistical models in S. Pacific Grove: Wadsworth & Brooks/Cole;1992. p. 309–376.15. Perkins NJ, Schisterman EF. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol. 2006; 163:670–675. PMID: 16410346.
Article16. Bishop JM, Cross KW. Physiological variables and mortality in patients with various categories of chronic respiratory disease. Bull Eur Physiopathol Respir. 1984; 20:495–500. PMID: 6440605.17. Lee JH, Chang JH. Lung function in patients with chronic airflow obstruction due to tuberculous destroyed lung. Respir Med. 2003; 97:1237–1242. PMID: 14635980.
Article18. Chaouat A, Naeije R, Weitzenblum E. Pulmonary hypertension in COPD. Eur Respir J. 2008; 32:1371–1385. PMID: 18978137.
Article19. Benza RL, Miller DP, Gomberg-Maitland M, Frantz RP, Foreman AJ, Coffey CS, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation. 2010; 122:164–172. PMID: 20585012.20. Lee PL, Jerng JS, Chang YL, Chen CF, Hsueh PR, Yu CJ, et al. Patient mortality of active pulmonary tuberculosis requiring mechanical ventilation. Eur Respir J. 2003; 22:141–147. PMID: 12882464.
Article21. Erbes R, Oettel K, Raffenberg M, Mauch H, Schmidt-Ioanas M, Lode H. Characteristics and outcome of patients with active pulmonary tuberculosis requiring intensive care. Eur Respir J. 2006; 27:1223–1228. PMID: 16481385.
Article22. Kim S, Kim H, Kim WJ, Lee SJ, Hong Y, Lee HY, et al. Mortality and predictors in pulmonary tuberculosis with respiratory failure requiring mechanical ventilation. Int J Tuberc Lung Dis. 2016; 20:524–529. PMID: 26970163.
Article23. Zahar JR, Azoulay E, Klement E, De Lassence A, Lucet JC, Regnier B, et al. Delayed treatment contributes to mortality in ICU patients with severe active pulmonary tuberculosis and acute respiratory failure. Intensive Care Med. 2001; 27:513–520. PMID: 11355119.
Article24. Jo YS, Park JH, Lee JK, Heo EY, Chung HS, Kim DK. Risk factors for pulmonary arterial hypertension in patients with tuberculosis-destroyed lungs and their clinical characteristics compared with patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017; 12:2433–2443. PMID: 28860738.
Article25. Song JW, Song JK, Kim DS. Echocardiography and brain natriuretic peptide as prognostic indicators in idiopathic pulmonary fibrosis. Respir Med. 2009; 103:180–186. PMID: 19097877.
Article26. Park SY, Lee CY, Kim C, Jang SH, Park YB, Park S, et al. One-year prognosis and the role of brain natriuretic peptide levels in patients with chronic cor pulmonale. J Korean Med Sci. 2015; 30:442–449. PMID: 25829812.
Article27. Rhee CK, Yoo KH, Lee JH, Park MJ, Kim WJ, Park YB, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis. 2013; 17:67–75. PMID: 23232006.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Factors Affecting Postoperative Morbidity and Mortality in Destroyed Lung
- Clinical Evaluation of Risk Factors Affection Postoperative Morbidity and Mortality in the Surgical Treatment of Tuberculous Destroyed Lung
- Treatment of acute respiratory failure: invasive mechanical ventilation
- Mechanical ventilation in patients with idiopathic pulmonary fibrosis in Korea: a nationwide cohort study
- Characteristics of Mechanical Ventilation Employed in Intensive Care Units: A Multicenter Survey of Hospitals