J Gastric Cancer.
2018 Jun;18(2):189-199. 10.5230/jgc.2018.18.e21.
Long-Term Nutritional Outcomes of Near-Total Gastrectomy in Gastric Cancer Treatment: a Comparison with Total Gastrectomy Using Propensity Score Matching Analysis
- Affiliations
-
- 1Division of Gastrointestinal Surgery, Department of Surgery, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea. painkiller9@catholic.ac.kr
- 2Division of Medical Oncology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
- KMID: 2414539
- DOI: http://doi.org/10.5230/jgc.2018.18.e21
Abstract
- PURPOSE
This study sought to examine whether near total gastrectomy (nTG) confers a long-term nutritional benefit when compared with total gastrectomy (TG) for the treatment of gastric cancer.
MATERIALS AND METHODS
Patients who underwent nTG or TG for gastric cancer were included (n=570). Using the 1:2 matched propensity score, 25 patients from the nTG group and 50 patients from the TG group were compared retrospectively for oncologic outcomes, including long-term survival and nutritional status.
RESULTS
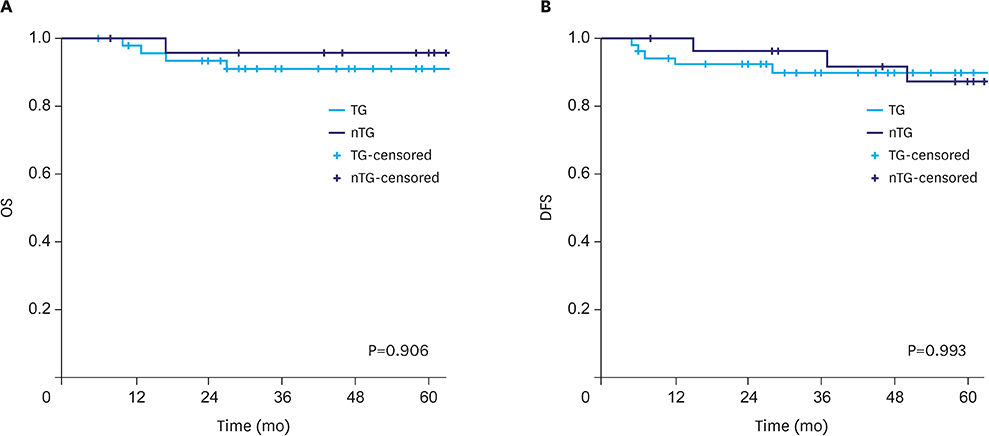
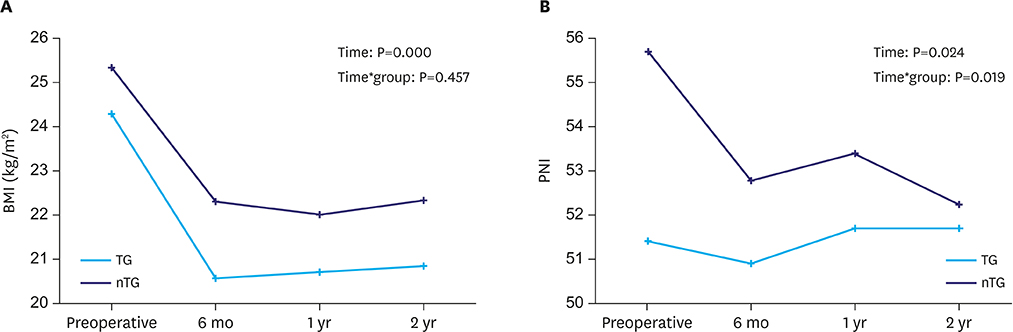
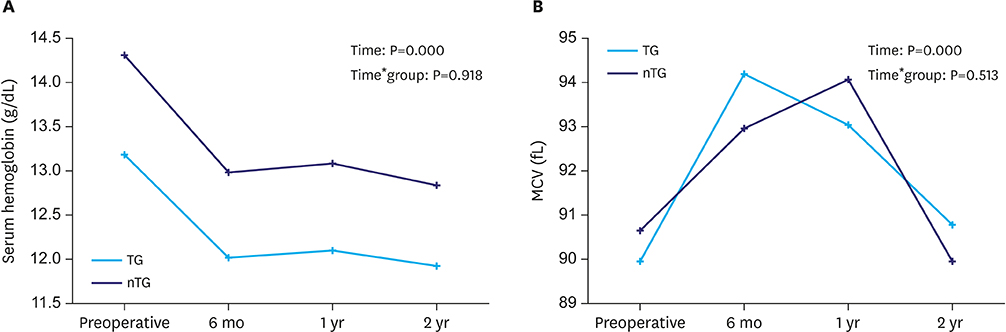
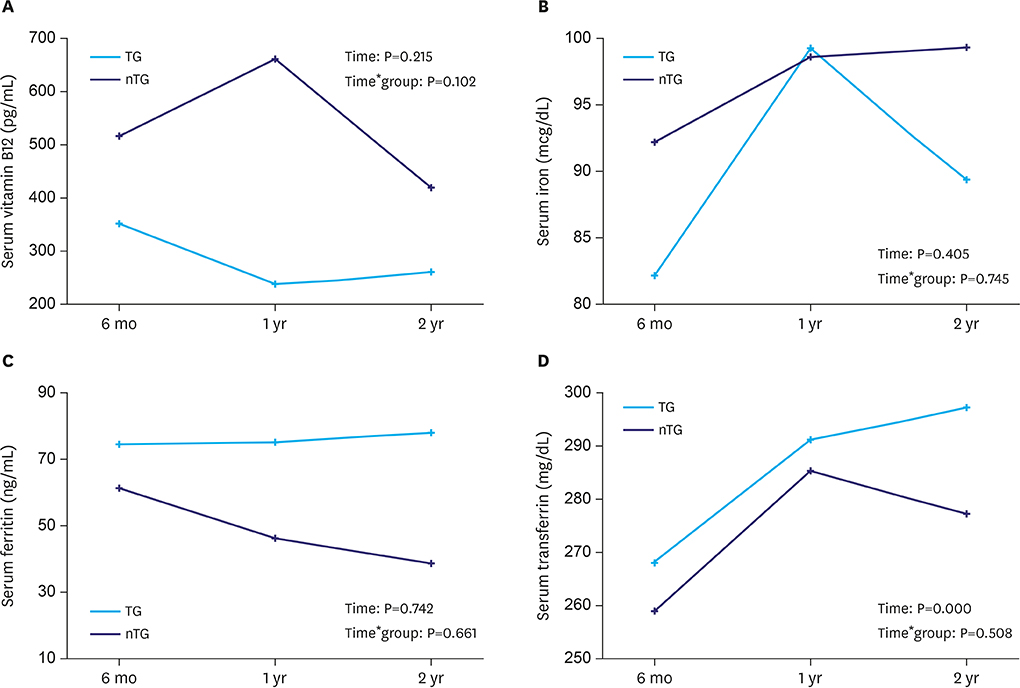
The length of the proximal resection margin, number of retrieved lymph nodes and tumor nodes, metastasis stage, short-term postoperative outcomes, and long-term survival were not significantly different between the groups. The body mass index values, and serum total protein and hemoglobin levels of the patients decreased significantly until postoperative 6 months, and then recovered slightly over time (P < 0.05); however, there was no difference in the levels between the groups. The prognostic nutritional index values and serum albumin levels decreased significantly until postoperative 6 months and then recovered (P < 0.05); the levels decreased more in the nTG group than in the TG group (P < 0.05). The mean corpuscular volumes and serum transferrin levels increased significantly until postoperative 1 year and then recovered slightly over time (P < 0.05); however, there was no difference between the groups. Serum vitamin B12, iron, and ferritin levels of the patients did not change significantly over time, and no difference existed between the groups.
CONCLUSIONS
A small remnant stomach after nTG conferred no significant nutritional benefits over TG.
MeSH Terms
Figure
Cited by 1 articles
-
Biomarkers for Evaluating the Inflammation Status in Patients with Cancer
Ali Guner, Hyoung-Il Kim
J Gastric Cancer. 2019;19(3):254-277. doi: 10.5230/jgc.2019.19.e29.
Reference
-
1. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–141.
Article2. Lee SS, Yu W, Chung HY, Kwon OK, Lee WK. Using quality of life scales with nutritional relevance after gastrectomy: a challenge for providing personalized treatment. J Gastric Cancer. 2017; 17:342–353.
Article3. Pyo JH, Lee H, Min BH, Lee JH, Choi MG, Lee JH, et al. Long-term outcome of endoscopic resection vs. surgery for early gastric cancer: a non-inferiority-matched cohort study. Am J Gastroenterol. 2016; 111:240–249.4. Pyo JH, Lee H, Min BH, Lee JH, Choi MG, Lee JH, et al. Early gastric cancer with a mixed-type Lauren classification is more aggressive and exhibits greater lymph node metastasis. J Gastroenterol. 2017; 52:594–601.
Article5. Kosuga T, Ichikawa D, Komatsu S, Okamoto K, Konishi H, Shiozaki A, et al. Feasibility and nutritional benefits of laparoscopic proximal gastrectomy for early gastric cancer in the upper stomach. Ann Surg Oncol. 2015; 22:Suppl 3. S929–S935.
Article6. Sasako M, Sano T, Yamamoto S, Sairenji M, Arai K, Kinoshita T, et al. Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol. 2006; 7:644–651.
Article7. Furukawa H, Kurokawa Y, Takiguchi S, Tanaka K, Miyazaki Y, Makino T, et al. Short-term outcomes and nutritional status after laparoscopic subtotal gastrectomy with a very small remnant stomach for cStage I proximal gastric carcinoma. Gastric Cancer. 2017; 21:500–507.
Article8. Migita K, Takayama T, Matsumoto S, Wakatsuki K, Enomoto K, Tanaka T, et al. Risk factors for esophagojejunal anastomotic leakage after elective gastrectomy for gastric cancer. J Gastrointest Surg. 2012; 16:1659–1665.
Article9. Kim DJ, Lee JH, Kim W. Comparison of the major postoperative complications between laparoscopic distal and total gastrectomies for gastric cancer using Clavien-Dindo classification. Surg Endosc. 2015; 29:3196–3204.
Article10. Fukagawa T, Gotoda T, Oda I, Deguchi Y, Saka M, Morita S, et al. Stenosis of esophago-jejuno anastomosis after gastric surgery. World J Surg. 2010; 34:1859–1863.
Article11. Nozoe T, Ninomiya M, Maeda T, Matsukuma A, Nakashima H, Ezaki T. Prognostic nutritional index: a tool to predict the biological aggressiveness of gastric carcinoma. Surg Today. 2010; 40:440–443.
Article12. Takagi H, Morimoto T. Near-total gastrectomy. J Surg Oncol. 1984; 26:14–16.
Article13. Salo JA, Saario I, Kivilaakso EO, Lempinen M. Near-total gastrectomy for gastric cancer. Am J Surg. 1988; 155:486–489.
Article14. Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010; 17:3077–3079.
Article15. Park KB, Park JY, Lee SS, Kwon OK, Chung HY, Yu W. Impact of body mass index on the quality of life after total gastrectomy for gastric cancer. Cancer Res Treat. 2017; DOI: 10.4143/crt.2017.080. [in press].
Article16. Lee MS, Ahn SH, Lee JH, Park DJ, Lee HJ, Kim HH, et al. What is the best reconstruction method after distal gastrectomy for gastric cancer? Surg Endosc. 2012; 26:1539–1547.
Article17. Lee J, Hur H, Kim W. Improved long-term quality of life in patients with laparoscopy-assisted distal gastrectomy with jejunal pouch interposition for early gastric cancer. Ann Surg Oncol. 2010; 17:2024–2030.
Article18. Lee HH, Song KY, Lee JS, Park SM, Kim JJ. Delta-shaped anastomosis, a good substitute for conventional Billroth I technique with comparable long-term functional outcome in totally laparoscopic distal gastrectomy. Surg Endosc. 2015; 29:2545–2552.
Article19. Lehnert T, Buhl K. Techniques of reconstruction after total gastrectomy for cancer. Br J Surg. 2004; 91:528–539.
Article20. Gertler R, Rosenberg R, Feith M, Schuster T, Friess H. Pouch vs. no pouch following total gastrectomy: meta-analysis and systematic review. Am J Gastroenterol. 2009; 104:2838–2851.
Article21. Scott JM, Molloy AM. The discovery of vitamin B12 . Ann Nutr Metab. 2012; 61:239–245.22. Couderc AL, Camalet J, Schneider S, Turpin JM, Bereder I, Boulahssass R, et al. Cobalamin deficiency in the elderly: aetiology and management: a study of 125 patients in a geriatric hospital. J Nutr Health Aging. 2015; 19:234–239.
Article23. Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T, et al. Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab. 2001; 86:4753–4758.
Article24. Castañeda TR, Tong J, Datta R, Culler M, Tschöp MH. Ghrelin in the regulation of body weight and metabolism. Front Neuroendocrinol. 2010; 31:44–60.
Article25. Stabler SP. Clinical practice. Vitamin B12 deficiency. N Engl J Med. 2013; 368:149–160.26. Lim CH, Kim SW, Kim WC, Kim JS, Cho YK, Park JM, et al. Anemia after gastrectomy for early gastric cancer: long-term follow-up observational study. World J Gastroenterol. 2012; 18:6114–6119.
Article27. Chaiyasate K, Jacobs M, Brooks SE, del Rosario G, Andrus L, Kestenberg W, et al. The uncut Roux-en-Y with jejunal pouch: a new reconstruction technique for total gastrectomy. Surgery. 2007; 142:33–39.
Article28. Nagai E, Ohuchida K, Nakata K, Miyasaka Y, Maeyama R, Toma H, et al. Feasibility and safety of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy: inverted T-shaped anastomosis using linear staplers. Surgery. 2013; 153:732–738.
Article29. Kong L, Yang N, Shi L, Zhao G, Wang M, Zhang Y. Total versus subtotal gastrectomy for distal gastric cancer: meta-analysis of randomized clinical trials. Onco Targets Ther. 2016; 9:6795–6800.
Article30. Lee SS, Chung HY, Kwon OK, Yu W. Long-term quality of life after distal subtotal and total gastrectomy: symptom- and behavior-oriented consequences. Ann Surg. 2016; 263:738–744.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic significance of splenectomy during completion total gastrectomy in patients with remnant gastric cancer: propensity score matching analysis
- Erratum: Clinical Feasibility of Vascular Navigation System During Laparoscopic Gastrectomy for Gastric Cancer: A Retrospective Comparison With Propensity-Score Matching
- Nutritional Consequences and Management After Gastrectomy
- Can Robotic Gastrectomy Surpass Laparoscopic Gastrectomy by Acquiring Long-Term Experience? A Propensity Score Analysis of a 7-Year Experience at a Single Institution
- Clinical Feasibility of Vascular Navigation System During Laparoscopic Gastrectomy for Gastric Cancer: A Retrospective Comparison With Propensity-Score Matching