Hanyang Med Rev.
2011 Nov;31(4):254-260. 10.7599/hmr.2011.31.4.254.
Nutritional Consequences and Management After Gastrectomy
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. Jmoonbae60@yahoo.co.kr
- KMID: 1451838
- DOI: http://doi.org/10.7599/hmr.2011.31.4.254
Abstract
- Gastric cancer is the most common cancer and the third most common cause of cancer deaths in Korea. Gastric resection, especially for the early stages of the disease, results in an excellent survival rate, and has been the mainstay of treatment for gastric cancer patients. Due to increasing use of surveillance endoscopy, the diagnosis of gastric cancer at early stages has increased. The 5-year survival rate for early gastric cancer has now improved to better than 90%, and consequently, the population of long-term survivors after gastrectomy has also increased. Therefore, the quality of life including nutritional support has become an important concern for gastrectomized patients during long-term follow-up. Nutritional capacities after gastrectomy should be evaluated by nutritional assessment and absorption tests. Nutritional deficits are more serious after total gastrectomy than after subtotal gastrectomy. Fat malabsorption has been shown to be a significant concern in patients that have undergone total gastrectomy. Other suggested causes of malnutrition include poor oral intake, relative pancreatic insufficiency, bacterial overgrowth, and shortened intestinal transit time. Food residue and bile reflux are frequently observed in the remnant stomach during surveillance endoscopy after a distal subtotal gastrectomy due to gastric cancer. The bile reflux is often associated with remnant gastritis or esophagitis and has an influence on the quality of life following a distal subtotal gastrectomy. Reconstruction methods have not influenced the food retention phenomenon after a distal gastrectomy over long-term periods. In addition, nutritional status after gastrectomy is significantly associated with postoperative complications. In conclusion, the provision of dietary education and nutritional support is highly recommended in postoperative patients for gastric cancer.
MeSH Terms
-
Absorption
Bile Reflux
Endoscopy
Esophagitis
Exocrine Pancreatic Insufficiency
Follow-Up Studies
Gastrectomy
Gastric Stump
Gastritis
Humans
Korea
Malnutrition
Nutrition Assessment
Nutritional Status
Nutritional Support
Postoperative Complications
Quality of Life
Retention (Psychology)
Stomach Neoplasms
Survival Rate
Survivors
Figure
Cited by 3 articles
-
Effect of Nutrition Education on the Eating Habits and Quality of Life of Gastric Cancer Outpatients Undergoing Gastrectomy
YoonHee Jung, Joomin Lee
Korean J Community Nutr. 2018;23(2):162-173. doi: 10.5720/kjcn.2018.23.2.162.Management of long-term gastric cancer survivors in Korea
Dong Wook Shin, Seung Hyun Yoo, Sung Sunwoo, Moon-Won Yoo
J Korean Med Assoc. 2016;59(4):256-265. doi: 10.5124/jkma.2016.59.4.256.Nutritional Care of Gastric Cancer Patients with Clinical Outcomes and Complications: A Review
Wook Jin Choi, Jeongseon Kim
Clin Nutr Res. 2016;5(2):65-78. doi: 10.7762/cnr.2016.5.2.65.
Reference
-
1. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011. 43:1–11.
Article2. Bae JM, Park JW, Yang HK, Kim JP. Nutritional status of gastric cancer patients after total gastrectomy. World J Surg. 1998. 22:254–260.
Article3. Ryu SW, Kim IH. Comparison of different nutritional assessments in detecting malnutrition among gastric cancer patients. World J Gastroenterol. 2010. 16:3310–3317.
Article4. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000. 894:i–xii. 1–253.5. Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987. 11:8–13.
Article6. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003. 22:415–421.
Article7. Buzby GP, Williford WO, Peterson OL, Crosby LO, Page CP, Reinhardt GF, et al. A randomized clinical trial of total parenteral nutrition in malnourished surgical patients: the rationale and impact of previous clinical trials and pilot study on protocol design. Am J Clin Nutr. 1988. 47:357–365.
Article8. Kuriyan R, Thomas T, Kurpad AV. Total body muscle mass estimation from bioelectrical impedance analysis & simple anthropometric measurements in Indian men. Indian J Med Res. 2008. 127:441–446.9. Park B, Yang JJ, Yang JH, Kim J, Cho LY, Kang D, et al. Reliability and data integration of duplicated test results using two bioelectrical impedence analysis machines in the Korean Genome and Epidemiology Study. J Prev Med Public Health. 2010. 43:479–485.
Article10. Yu W, Chung HY. Nutritional status after curative surgery in patients with gastric cancer: comparison of total versus subtotal gastrectomy. J Korean Surg Soc. 2001. 60:297–301.11. Tanaka S, Matsuo K, Matsumoto H, Maki T, Nakano M, Sasaki T, et al. Clinical outcomes of Roux-en-Y and Billroth I reconstruction after a distal gastrectomy for gastric cancer: What is the optimal reconstructive procedure? Hepatogastroenterology. 2011. 58:257–262.12. Pellegrini CA, Deveney CW, Patti MG, Lewin M, Way LW. Intestinal transit of food after total gastrectomy and Roux-Y esophagojejunostomy. Am J Surg. 1986. 151:117–125.
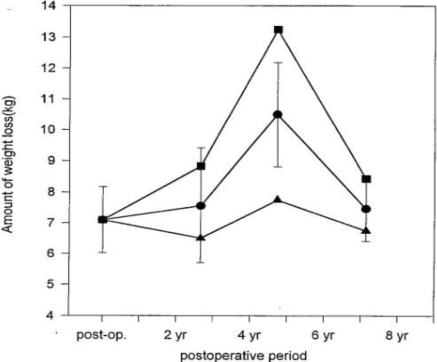
Article13. Jung HJ, Lee JH, Ryu KW, Lee JY, Kim CG, Choi IJ, et al. The influence of reconstruction methods on food retention phenomenon in the remnant stomach after a subtotal gastrectomy. J Surg Oncol. 2008. 98:11–14.
Article14. Bae JM. Kim JP, editor. Nutritional problems in gastrectomy. Gastric cancer. 1999. Seoul: Medrang;283–295.15. Zittel TT, Glatzle J, Muller M, Kreis ME, Raybould HE, Becker HD, et al. Total gastrectomy severely alters the central regulation of food intake in rats. Ann Surg. 2002. 236:166–176.
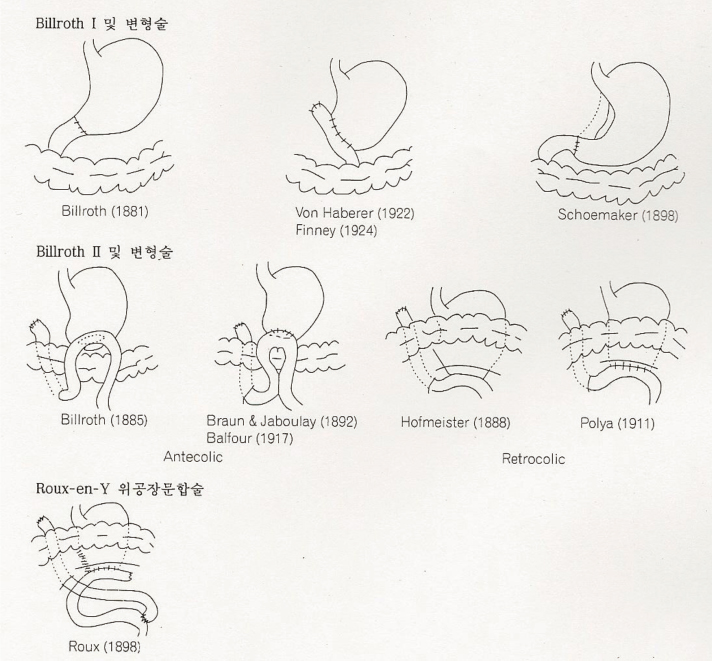
Article16. Kim JP, Yoo HJ. Kim JP, editor. Reconstructive surgery after gastrectomy in the stomach cancer patient. Gastric cancer. 1999. Seoul: Medrang;176–183.17. Copland L, Liedman B, Rothenberg E, Bosaeus I. Effects of nutritional support long time after total gastrectomy. Clin Nutr. 2007. 26:605–613.
Article18. Adachi S, Takiguchi S, Okada K, Yamamoto K, Yamasaki M, Miyata H, et al. Effects of ghrelin administration after total gastrectomy: a prospective, randomized, placebocontrolled phase II study. Gastroenterology. 2010. 138:1312–1320.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Post-Operative Nutritional Status according to the Extent of Gastrectomy and the Reconstruction Method in Patients with Gastric Cancer
- Factors Associated with Early Nutritional Status after Radical Gastrectomy in Patients with Gastric Cancer
- Nutritional treatment after gastrectomy
- Nutritional Intervention for a Patient with Laparoscopic Sleeve Gastrectomy for Morbid Obesity: a Case Report
- Nutritional Status after Curative Surgery in Patients with Gastric Cancer: Comparison of Total Versus Subtotal Gastrectomy