J Korean Foot Ankle Soc.
2018 Jun;22(2):78-81. 10.14193/jkfas.2018.22.2.78.
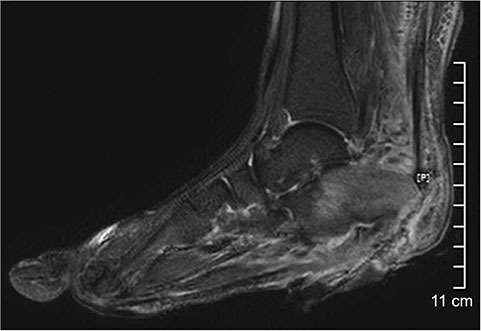
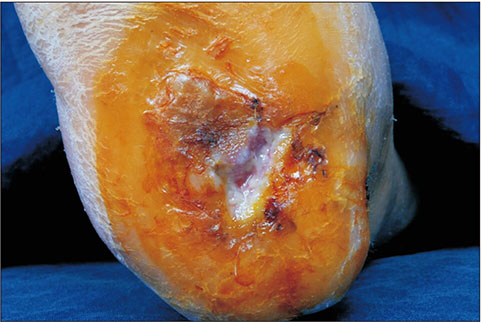
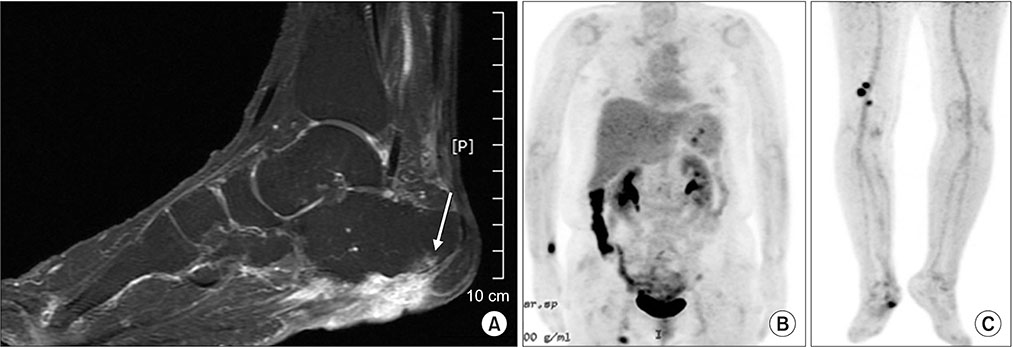
Early Transformed Diabetic Foot Ulcer into a Malignancy: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea. parkyounguk@gmail.com
- 2Department of Orthopedic Surgery, Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- 3Department of Plastic Surgery, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2413717
- DOI: http://doi.org/10.14193/jkfas.2018.22.2.78
Abstract
- This paper presents a case of an early malignant transformation of untreated ulcers in a patient with diabetes. This case shows that Marjolin's ulcer can occur not only after chronic injury, but can also develop in the early stages after the onset. Hence, an early biopsy for diabetic foot ulcers that fail to heal with acute treatment can enable an earlier diagnosis and treatment without amputation, resulting in a better quality of life for the patient.
Keyword
Figure
Reference
-
1. Ozek C, Cankayali R, Bilkay U, Guner U, Gundogan H, Songur E, et al. Marjolin's ulcers arising in burn scars. J Burn Care Rehabil. 2001; 22:384–389.
Article2. Elkins-Williams ST, Marston WA, Hultman CS. Management of the chronic burn wound. Clin Plast Surg. 2017; 44:679–687.
Article3. Spring PM, Myers JN, El-Naggar AK, Langstein HN. Malignant melanoma arising within a burn scar case report and review of the literature. Ann Otol Rhinol Laryngol. 2001; 110:369–376.
Article4. Fleming MD, Hunt JL, Purdue GF, Sandstad J. Marjolin's ulcer: a review and reevaluation of a difficult problem. J Burn Care Rehabil. 1990; 11:460–469.5. Oruç M, Kankaya Y, Sungur N, Özer K, Işık VM, Ulusoy MG, et al. Clinicopathological evaluation of Marjolin ulcers over two decades. Kaohsiung J Med Sci. 2017; 33:327–333.
Article6. Scatena A, Zampa V, Fanelli G, Iacopi E, Piaggesi A. A metastatic squamous cell carcinoma in a diabetic foot: case report. Int J Low Extrem Wounds. 2016; 15:155–157.7. Copcu E. Marjolin's ulcer: a preventable complication of burns? Plast Reconstr Surg. 2009; 124:156e–164e.
Article8. Pekarek B, Buck S, Osher L. A comprehensive review on Marjolin's ulcers: diagnosis and treatment. J Am Col Certif Wound Spec. 2011; 3:60–64.
Article9. Saaiq M, Ashraf B. Marjolin's ulcers in the post-burned lesions and scars. World J Clin Cases. 2014; 2:507–514.
Article10. Horton CE, Crawford HH, Love HG, Loeffler RA. The malignant potential of burn scar. Plast Reconstr Surg Transplant Bull. 1958; 22:348–353.
Article