J Pathol Transl Med.
2018 Mar;52(2):121-125. 10.4132/jptm.2017.08.20.
Combined Adenosquamous and Large Cell Neuroendocrine Carcinoma of the Gallbladder
- Affiliations
-
- 1Department of Pathology, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea. lepetit80@hanmail.net
- 2Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- KMID: 2408513
- DOI: http://doi.org/10.4132/jptm.2017.08.20
Abstract
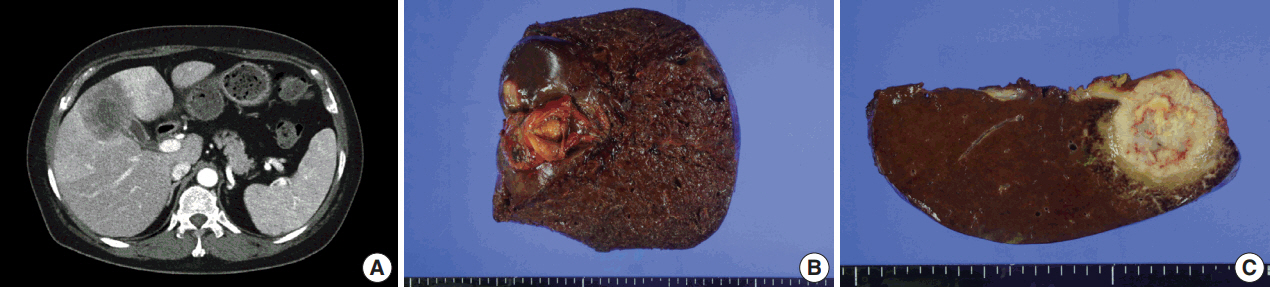
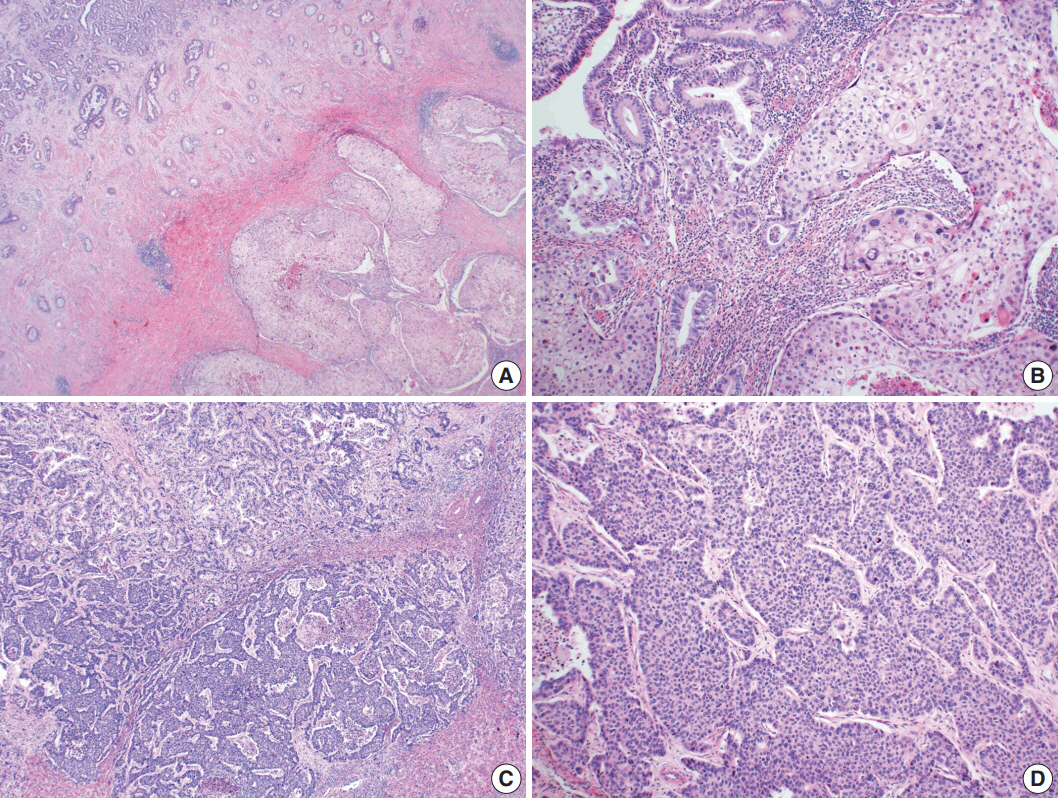
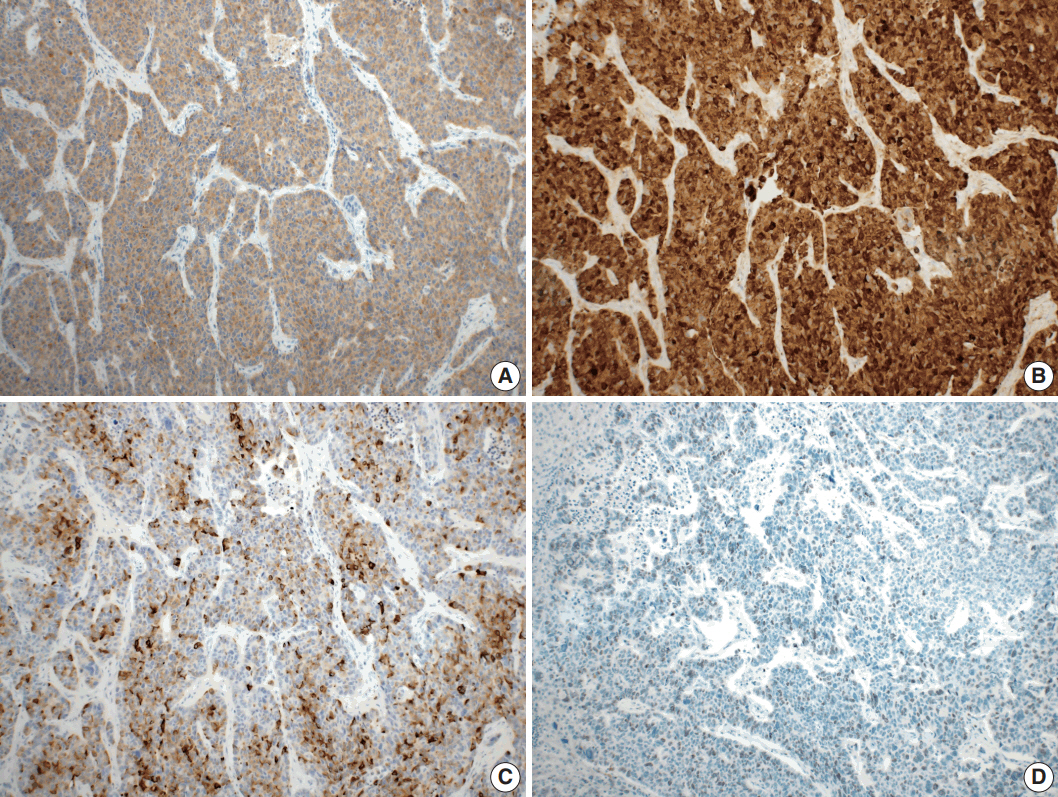
- Large cell neuroendocrine carcinoma (LCNEC) of the gallbladder is extremely rare and usually combined with other type of malignancy, mostly adenocarcinoma. We report an unusual case of combined adenosquamous carcinoma and LCNEC of the gallbladder in a 54-year-old woman. A radical cholecystectomy specimen revealed a 4.3×4.0 cm polypoid mass in the fundus with infiltration of adjacent liver parenchyma. Microscopically, the tumor consisted of two distinct components. Adenosquamous carcinoma was predominant and abrupt transition from adenocarcinoma to squamous cell carcinoma was observed. LCNEC showed round cells with large, vesicular nuclei, abundant mitotic figures, and occasional pseudorosette formation. The patient received adjuvant chemotherapy. However, multiple liver metastases were identified at 3-month follow-up. Metastatic nodules were composed of LCNEC and squamous cell carcinoma components. Detecting LCNEC component is important in gallbladder cancer, because the tumor may require a different chemotherapy regimen and show early metastasis and poor prognosis.
MeSH Terms
Figure
Reference
-
1. National Cancer Institute. SEER data, 1973-2005 [Internet]. Rockville: National Cancer Institute;2008. [cited 2017 Sep 1]. Available from: http://seer.cancer.gov/.2. Henson DE, Albores-Saavedra J, Corle D. Carcinoma of the gallbladder: histologic types, stage of disease, grade, and survival rates. Cancer. 1992; 70:1493–7.
Article3. Liu W, Wang L, He XD, Feng C, Chang XY, Lu ZH. Mixed large cell neuroendocrine carcinoma and adenocarcinoma of the gallbladder: a case report and brief review of the literature. World J Surg Oncol. 2015; 13:114.
Article4. Buscemi S, Orlando E, Damiano G, et al. "Pure" large cell neuroendocrine carcinoma of the gallbladder: report of a case and review of the literature. Int J Surg. 2016; 28 Suppl 1:S128–32.
Article5. Eltawil KM, Gustafsson BI, Kidd M, Modlin IM. Neuroendocrine tumors of the gallbladder: an evaluation and reassessment of management strategy. J Clin Gastroenterol. 2010; 44:687–95.6. Alpuerto AC, Mora ME, Robitsek RJ, Schubl SD. Primary pure squamous cell carcinoma of the gallbladder locally invading the liver, duodenum, and stomach: a case report and literature review. Case Rep Surg. 2017; 2017:2534029.
Article7. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC Press;2010. p. 274–6.8. Noske A, Pahl S. Combined adenosquamous and large-cell neuroendocrine carcinoma of the gallbladder. Virchows Arch. 2006; 449:135–6.
Article9. Kanthan R, Senger JL, Ahmed S, Kanthan SC. Gallbladder cancer in the 21st century. J Oncol. 2015; 2015:967472.
Article10. Albores-Saavedra J, Nadji M, Henson DE, Angeles-Angeles A. Enteroendocrine cell differentiation in carcinomas of the gallbladder and mucinous cystadenocarcinomas of the pancreas. Pathol Res Pract. 1988; 183:169–75.
Article11. Christie AC. Three cases illustrating the presence of argentaffin (kultschitzky) cells in the human gall-bladder. J Clin Pathol. 1954; 7:318–21.
Article12. Hart IR, Fidler IJ. The implications of tumor heterogeneity for studies on the biology of cancer metastasis. Biochim Biophys Acta. 1981; 651:37–50.13. Hoshimoto S, Hoshi S, Hishinuma S, et al. Adenosquamous carcinoma in the biliary tract: association of the proliferative ability of the squamous component with its proportion and tumor progression. Scand J Gastroenterol. 2017; 52:425–30.
Article14. Chen C, Wang L, Liu X, Zhang G, Zhao Y, Geng Z. Gallbladder neuroendocrine carcinoma: report of 10 cases and comparision of clinicopathologic features with gallbladder adenocarcinoma. Int J Clin Exp Pathol. 2015; 8:8218–26.15. Acosta AM, Wiley EL. Primary biliary mixed adenoneuroendocrine carcinoma (MANEC): a short review. Arch Pathol Lab Med. 2016; 140:1157–62.
Article16. Verlicchi L, Blons H, Hannoun L, Bachet JB. Squamous-cell gallbladder carcinoma: how to treat? J Cell Sci Ther. 2015; 6:212.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Large Cell Neuroendocrine Carcinoma of the Maxillary Sinus
- Small Cell Carcinoma of the Gallbladder: A Case Report
- A Case of Primary Neuroendocrine Carcinoma of the Gallbladder Associated with Anomalous Union of the Pancreaticobiliary Duct
- Adenosquamous Cell Carcinoma of the Gallbladder: A case report
- Combined Large Cell Neuroendocrine Carcinoma with Component of Adenocarcinoma: A case report