Endocrinol Metab.
2017 Dec;32(4):460-465. 10.3803/EnM.2017.32.4.460.
Detection of Polyethylene Glycol Thyrotropin (TSH) Precipitable Percentage (Macro-TSH) in Patients with a History of Thyroid Cancer
- Affiliations
-
- 1Department of Internal Medicine, University of Genoa, Genoa, Italy. magius@unige.it
- 2Endocrine Unit, San Martino University Hospital, Genoa, Italy.
- 3Laboratory Analysis Unit, San Martino University Hospital, Genoa, Italy.
- KMID: 2406190
- DOI: http://doi.org/10.3803/EnM.2017.32.4.460
Abstract
- BACKGROUND
Owing to its large molecular size, polyethylene glycol (PEG)-precipitable thyrotropin (TSH) can accumulate in the circulation, elevating TSH levels. PEG-precipitable TSH can be used to detect macro-TSH (mTSH) in serum. Our aim was to evaluate the prevalence of mTSH in patients who had undergone thyroidectomy for thyroid cancer.
METHODS
Seventy-three thyroid cancer patients and 24 control subjects on levothyroxine (LT4) TSH-suppressive or replacement therapy were evaluated. Screening for mTSH was performed by adding PEG to serum in order to precipitate γ-globulin. A percentage of PEG-precipitable TSH ≥80% was considered suggestive of mTSH.
RESULTS
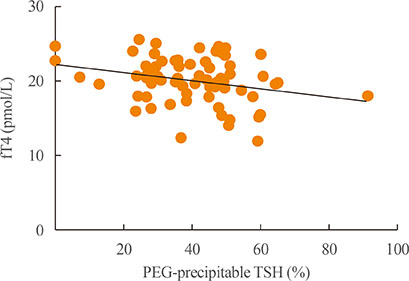
No correlation between free-T4 (fT4) and TSH levels was found. PEG-precipitable TSH was 39.3%±1.9% in thyroid cancer patients and 44.1%±3.9% in controls. Macro-TSH was deemed to be present in one thyroid cancer patient and in two control subjects. Only in the thyroid cancer group was PEG-precipitable TSH found to be negatively correlated with fT4 concentration. No correlation was found between PEG-precipitable TSH and other clinical conditions in any patients.
CONCLUSION
The presence of mTSH seems to be a rare phenomenon in thyroid cancer. In some patients with low PEG-precipitable TSH, a reduction in LT4 dosage could be suggested. LT4 dosage adjusted to body weight is the main factor in maintaining TSH in a semi-suppressed or normal range. Evaluation of mTSH could be necessary in patients in whom a balance is required between adequate TSH suppression and the avoidance of unnecessary exogenous hyperthyroxinemia.
Keyword
MeSH Terms
Figure
Reference
-
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26:1–133.2. Biondi B, Cooper DS. Benefits of thyrotropin suppression versus the risks of adverse effects in differentiated thyroid cancer. Thyroid. 2010; 20:135–146.3. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000; 160:526–534.4. Lam E, Strugnell SS, Bajdik C, Holmes D, Wiseman SM. Limited adequacy of thyroid cancer patient follow-up at a Canadian tertiary care centre. Can J Surg. 2013; 56:385–392.5. Giusti M, Mortara L, Machello N, Monti E, Pera G, Marenzana M. Utility of a liquid formulation of levo-thyroxine in differentiated thyroid cancer patients. Drug Res (Stuttg). 2015; 65:332–336.6. Batrinos ML. The problem of exogenous subclinical hyperthyroidism. Hormones (Athens). 2006; 5:119–125.7. Santini F, Pinchera A, Marsili A, Ceccarini G, Castagna MG, Valeriano R, et al. Lean body mass is a major determinant of levothyroxine dosage in the treatment of thyroid diseases. J Clin Endocrinol Metab. 2005; 90:124–127.8. Skelin M, Lucijanic T, Amidzic Klaric D, Resic A, Bakula M, Liberati-Cizmek AM, et al. Factors affecting gastrointestinal absorption of levothyroxine: a review. Clin Ther. 2017; 39:378–403.9. Padwal R, Brocks D, Sharma AM. A systematic review of drug absorption following bariatric surgery and its theoretical implications. Obes Rev. 2010; 11:41–50.10. Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017; 27:315–389.11. Kricka LJ. Human anti-animal antibody interferences in immunological assays. Clin Chem. 1999; 45:942–956.12. Gurnell M, Halsall DJ, Chatterjee VK. What should be done when thyroid function tests do not make sense? Clin Endocrinol (Oxf). 2011; 74:673–678.13. Sakai H, Fukuda G, Suzuki N, Watanabe C, Odawara M. Falsely elevated thyroid-stimulating hormone (TSH) level due to macro-TSH. Endocr J. 2009; 56:435–440.14. Rix M, Laurberg P, Porzig C, Kristensen SR. Elevated thyroid-stimulating hormone level in a euthyroid neonate caused by macro thyrotropin-IgG complex. Acta Paediatr. 2011; 100:e135–e137.15. Loh TP, Kao SL, Halsall DJ, Toh SA, Chan E, Ho SC, et al. Macro-thyrotropin: a case report and review of literature. J Clin Endocrinol Metab. 2012; 97:1823–1828.16. Samson SL, Hamrahian AH, Ezzat S. AACE Neuroendocrine and Pituitary Scientific Committee. American College of Endocrinology (ACE). American Association of Clinical Endocrinologists, American College of Endocrinology Disease state clinical review: clinical relevance of macroprolactin in the absence or presence of true hyperprolactinemia. Endocr Pract. 2015; 21:1427–1435.17. Hattori N, Ishihara T, Yamagami K, Shimatsu A. Macro TSH in patients with subclinical hypothyroidism. Clin Endocrinol (Oxf). 2015; 83:923–930.18. Hattori N, Ishihara T, Shimatsu A. Variability in the detection of macro TSH in different immunoassay systems. Eur J Endocrinol. 2016; 174:9–15.19. Hattori N, Ishihara T, Matsuoka N, Saito T, Shimatsu A. Anti-thyrotropin autoantibodies in patients with macro-thyrotropin and long-term changes in macro-thyrotropin and serum thyrotropin levels. Thyroid. 2017; 27:138–146.20. Kadoya M, Koyama S, Morimoto A, Miyoshi A, Kakutani M, Hamamoto K, et al. Serum macro TSH level is associated with sleep quality in patients with cardiovascular risks: HSCAA Study. Sci Rep. 2017; 7:44387.21. Smith TP, Suliman AM, Fahie-Wilson MN, McKenna TJ. Gross variability in the detection of prolactin in sera containing big big prolactin (macroprolactin) by commercial immunoassays. J Clin Endocrinol Metab. 2002; 87:5410–5415.22. Ismail AA, Walker PL, Barth JH, Lewandowski KC, Jones R, Burr WA. Wrong biochemistry results: two case reports and observational study in 5310 patients on potentially misleading thyroid-stimulating hormone and gonadotropin immunoassay results. Clin Chem. 2002; 48:2023–2029.23. Lewis EJ, Lim R, Joseph F, Ewins D, Goenka N, Bowles SA, et al. Recognising macro-TSH: a rare cause of inappropriately high TSH values. Clin Chem Lab Med. 2011; 49:Suppl. S421.24. Mills F, Jeffery J, Mackenzie P, Cranfield A, Ayling RM. An immunoglobulin G complexed form of thyroid-stimulating hormone (macro thyroid-stimulating hormone) is a cause of elevated serum thyroid-stimulating hormone concentration. Ann Clin Biochem. 2013; 50(Pt 5):416–420.25. Sukumar R, Agarwal A, Gupta S, Mishra A, Agarwal G, Verma AK, et al. Prediction of LT4 replacement dose to achieve euthyroidism in subjects undergoing total thyroidectomy for benign thyroid disorders. World J Surg. 2010; 34:527–531.26. Del Duca SC, Santaguida MG, Brusca N, Gatto I, Cellini M, Gargano L, et al. Individually-tailored thyroxine requirement in the same patients before and after thyroidectomy: a longitudinal study. Eur J Endocrinol. 2015; 173:351–357.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of idiopathic thyrotropin (TSH) deficiency
- TSH Suppression after Differentiated Thyroid Cancer Surgery and Osteoporosis
- Clinical Significance of Thyrotropin Measurement as a Screening Test in Ambulatory Patients
- Consideration of Serum Thyrotropin When Interpreting Serum Thyroglobulin Level in Patients with Differentiated Thyroid Cancer
- Preoperative Thyroid-stimulating Hormone Levels as a Predictor of Thyroid Carcinoma