World J Mens Health.
2015 Dec;33(3):194-201. 10.5534/wjmh.2015.33.3.194.
Changes in Nocturia and Lower Urinary Tract Symptoms after Radical Prostatectomy
- Affiliations
-
- 1Department of Urology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. ksw1227@catholic.ac.kr
- 2Catholic Integrative Medicine Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Urology, St. Paul's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2405148
- DOI: http://doi.org/10.5534/wjmh.2015.33.3.194
Abstract
- PURPOSE
The goal of this study was to evaluate changes in nocturia and other lower urinary tract symptoms (LUTS) after laparoscopic radical prostatectomy (LRP) and robot-assisted laparoscopic radical prostatectomy (RALP).
MATERIALS AND METHODS
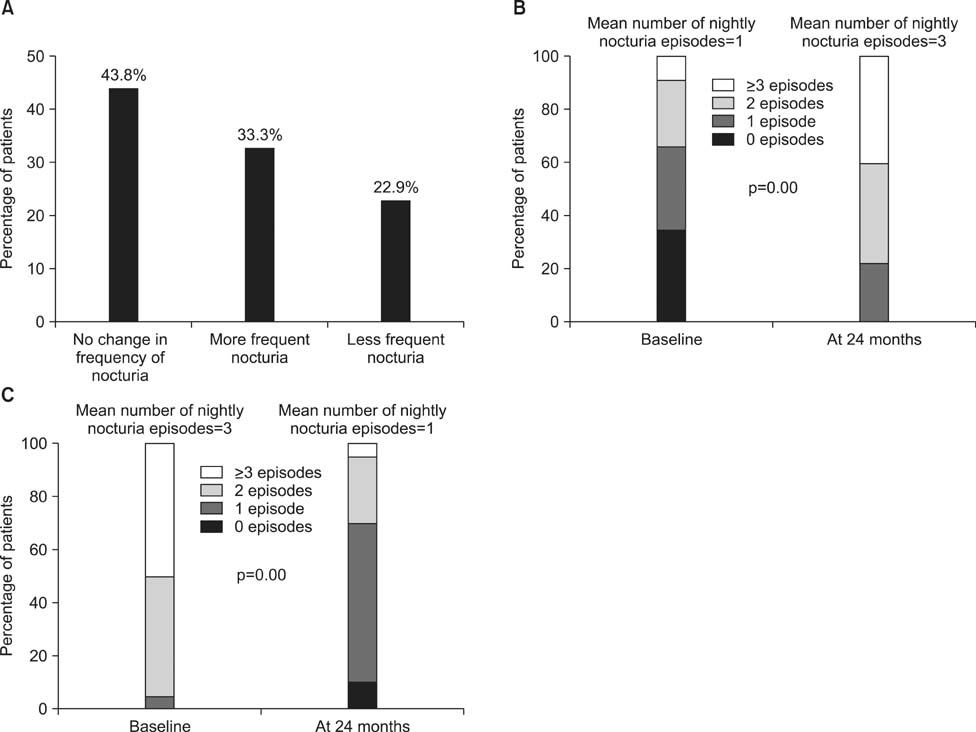
We reviewed the medical records of 96 patients who underwent LRP or RALP for clinically localized prostate cancer and completed the International Prostate Symptom Score (IPSS) questionnaire, which provided a basis for assessing their symptoms. We also evaluated maximal flow rate and post-void residual urine volume over a follow-up period of at least 24 months. We divided the patients into three groups according to postoperative changes in the frequency of nocturia.
RESULTS
Voiding symptoms significantly improved over the course of 24 months in patients who underwent LRP or RALP. However, most patients showed persistent or increased nocturia after LRP or RALP. Moreover, more than one third of the patients (33/96) presented with exacerbated nocturia (1.0+/-0.9 episodes of preoperative nocturia vs. 3.0+/-1.3 episodes of postoperative nocturia). Multiple regression analysis showed that preoperative IPSS storage sub-score had negative association with the nocturia after radical prostatectomy (p=0.005). However, patients' age, body mass index, preoperative prostate specific antigen, Gleason score, T-stage, and prostate volume had no association.
CONCLUSIONS
The present study showed that nocturia was influenced by a range of factors, including other storage LUTS and the relief of bladder outlet obstruction after radical prostatectomy. Moreover, the preoperative storage symptoms are regarded as an important factor which influences the changes of nocturia after radical prostatectomy.
MeSH Terms
Figure
Reference
-
1. Boorjian SA, Eastham JA, Graefen M, Guillonneau B, Karnes RJ, Moul JW, et al. A critical analysis of the long-term impact of radical prostatectomy on cancer control and function outcomes. Eur Urol. 2012; 61:664–675.
Article2. Moran PS, O'Neill M, Teljeur C, Flattery M, Murphy LA, Smyth G, et al. Robot-assisted radical prostatectomy compared with open and laparoscopic approaches: a systematic review and meta-analysis. Int J Urol. 2013; 20:312–321.
Article3. Kim TH, Han DH, Lee KS. The prevalence of lower urinary tract symptoms in Korean men aged 40 years or older: a population-based survey. Int Neurourol J. 2014; 18:126–132.
Article4. Resnick MJ, Barocas DA, Morgans AK, Phillips SE, Chen VW, Cooperberg MR, et al. Contemporary prevalence of pretreatment urinary, sexual, hormonal, and bowel dysfunction: Defining the population at risk for harms of prostate cancer treatment. Cancer. 2014; 120:1263–1271.
Article5. Masters JG, Rice ML. Improvement in urinary symptoms after radical prostatectomy: a prospective evaluation of flow rates and symptom scores. BJU Int. 2003; 91:795–797.
Article6. Lepor H, Kaci L. The impact of open radical retropubic prostatectomy on continence and lower urinary tract symptoms: a prospective assessment using validated self-administered outcome instruments. J Urol. 2004; 171:1216–1219.
Article7. Slova D, Lepor H. The short-term and long-term effects of radical prostatectomy on lower urinary tract symptoms. J Urol. 2007; 178:2397–2400.
Article8. Giannantoni A, Mearini E, Zucchi A, Costantini E, Mearini L, Bini V, et al. Bladder and urethral sphincter function after radical retropubic prostatectomy: a prospective long-term study. Eur Urol. 2008; 54:657–664.
Article9. Van Kerrebroeck P, Andersson KE. Terminology, epidemiology, etiology, and pathophysiology of nocturia. Neurourol Urodyn. 2014; 33:Suppl 1. S2–S5.
Article10. Schneider T, de la Rosette JJ, Michel MC. Nocturia: a nonspecific but important symptom of urological disease. Int J Urol. 2009; 16:249–256.
Article11. Marshall SD, Raskolnikov D, Blanker MH, Hashim H, Kupelian V, Tikkinen KA, et al. International Consultations on Urological Diseases. Nocturia: current levels of evidence and recommendations from the international consultation on male lower urinary tract symptoms. Urology. 2015; 85:1291–1299.12. Matsubara A, Yoneda T, Yasumoto H, Teishima J, Shiina H, Igawa M, et al. Lower urinary tract symptoms after radical perineal prostatectomy. Jpn J Clin Oncol. 2007; 37:534–539.
Article13. Namiki S, Saito S, Ishidoya S, Tochigi T, Ioritani N, Yoshimura K, et al. Adverse effect of radical prostatectomy on nocturia and voiding frequency symptoms. Urology. 2005; 66:147–151.
Article14. Homma Y, Kawabe K, Tsukamoto T, Yamaguchi O, Okada K, Aso Y, et al. Estimate criteria for diagnosis and severity in benign prostatic hyperplasia. Int J Urol. 1996; 3:261–266.
Article15. Prabhu V, Taksler GB, Sivarajan G, Laze J, Makarov DV, Lepor H. Radical prostatectomy improves and prevents age dependent progression of lower urinary tract symptoms. J Urol. 2014; 191:412–417.
Article16. Choi WS, Ku JH, Oh SJ, Kim SW, Paick JS. Change of nocturnal polyuria after holmium laser enucleation of the prostate in patients with benign prostatic hyperplasia. Urology. 2014; 84:650–656.
Article17. Gordon A, Skarecky DW, Ahlering T. Long-term outcomes in severe lower urinary tract symptoms in men undergoing robotic-assisted radical prostatectomy. Urology. 2014; 84:826–831.
Article18. Tikkinen KA, Auvinen A, Johnson TM 2nd, Weiss JP, Keränen T, Tiitinen A, et al. A systematic evaluation of factors associated with nocturia: the population-based FINNO study. Am J Epidemiol. 2009; 170:361–368.19. De Ridder D, Roumeguère T, Kaufman L. Urgency and other lower urinary tract symptoms in men aged ≥ 40 years: a Belgian epidemiological survey using the ICIQ-MLUTS questionnaire. Int J Clin Pract. 2015; 69:358–365.20. Kayali M, Balci M, Aslan Y, Bilgin O, Guzel O, Tuncel A, et al. The relationship between prostate cancer and presence of metabolic syndrome and late-onset hypogonadism. Urology. 2014; 84:1448–1452.
Article21. Hutchinson RC, Thiel DD, Tavlarides AM, Diehl NN, Parker AS. The effect of robot-assisted laparoscopic prostatectomy on nocturia. J Endourol. 2012; 26:861–865.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Laparoscopic Radical Prostatectomy on Urinary Incontinence and Lower Urinary Tract Symptoms
- Nocturia
- Factors Affecting Quality of Life in Patients with Radical Prostatectomy
- Nocturia is the Lower Urinary Tract Symptom With Greatest Impact on Quality of Life of Men From a Community Setting
- Practical Tip for Management of Nocturia