Korean J Urol.
2008 Feb;49(2):134-138.
Impact of Laparoscopic Radical Prostatectomy on Urinary Incontinence and Lower Urinary Tract Symptoms
- Affiliations
-
- 1Department of Urology, College of Medicine, The Catholic University of Korea, Seoul, Korea. kjc@catholic.ac.kr
Abstract
- PURPOSE
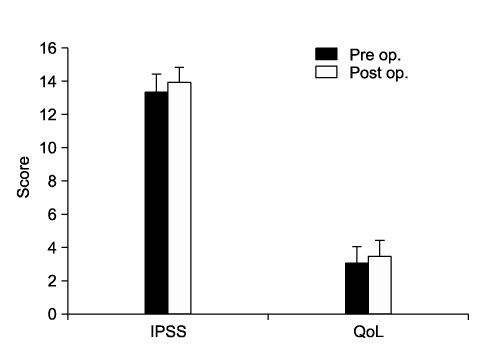
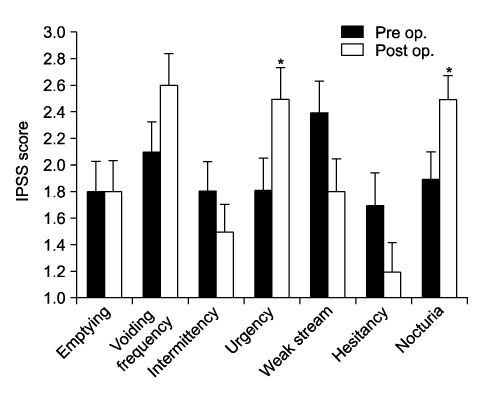
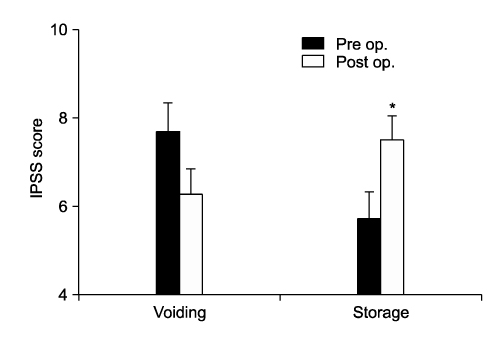
The definition of continence after radical prostatectomy has not been established. We examined the continence rate and changes in voiding and storage symptoms after laparoscopic radical prostatectomy(LRP). MATERIALS AND METHODS: Fifty-seven patients were enrolled and followed for more than 12 months after a LRP. Postoperative evaluation of urinary incontinence was performed by interview, and was classified as completely dry, intermittent(occasional dribbling only), using only 1 pad/day, using more than 1 pad/day, and no control. Pre- and post-operative International Prostate Symptom Scores(IPSS) were compared(Total, each criterion, and quality of life, voiding, and storage symptom subscores). RESULTS: Sixty seven percent of patients were completely dry and 17% of patients were classified as intermittent. Those using 1 pad/day, more than 1 pad/day, or no control accounted for 2%, 9%, and 5%, respectively. Pre- and post-operative total IPSS and quality of life scores were not different, but urgency and nocturia scores increased(p<0.05). The voiding subscore decreased and the storage subscore increased after LRP(p<0.05), suggesting aggravation of storage symptoms after LRP. CONCLUSIONS: We need to determine which definition of continence is most clinically useful. It is important to assess lower urinary tract symptoms, especially storage symptoms, as well as urinary incontinence after LRP.
Keyword
MeSH Terms
Figure
Reference
-
1. Schuessler WW, Schulam PG, Clayman RV, Kavoussi LR. Laparoscopic radical prostatectomy: initial short-term experience. Urology. 1997. 50:854–857.2. Jang J, Cha SH, Kim DB, Kim JC, Hwang TK. Laparoscopic radical prostatectomy. Korean J Urol. 2002. 43:342–345.3. Foote J, Yun S, Leach GE. Postprostatectomy incontinence. Pathophysiology, evaluation, and management. Urol Clin North Am. 1991. 18:229–241.4. Davidson PJ, van den Ouden D, Schroeder FH. Radical prostatectomy: prospective assessment of mortility and morbidity. Eur Urol. 1996. 29:168–173.5. Ficarra V, Novara G, Galfano A, Stringari C, Baldassarre R, Cavalleri S, et al. Twelve-month self-reported quality of life after retropubic radical prostatectomy: a prospective study with Rand 36-Item Health Survey (Short Form-36). BJU Int. 2005. 97:274–278.6. Jacobsen NE, Moore KN, Estey E, Voaklander D. Open versus laparoscopic radical prostatectomy: a prospective comparison of postoperative urinary incontinence rates. J Urol. 2007. 177:615–619.7. Kaye KW, Creed KE, Wilson GJ, D'Antuono M, Dawkins HJ. Urinary continence after radical retropubic prostatectomy. Analysis and synthesis of contributing factors: a unified concept. Br J Urol. 1997. 80:444–501.8. Catalona WJ, Basler JW. Return of erections and urinary continence following nerve sparing radical retropubic prostatectomy. J Urol. 1993. 150:905–907.9. Steiner MS, Morton RA, Walsh PC. Impact of anatomical radical prostatectomy on urinary incontinence. J Urol. 1991. 145:512–515.10. Namiki S, Saito S, Satoh M, Ishidoya S, Kawamura S, Tochigi T, et al. Quality of life after radical prostatectomy in Japanese men: 2 year longitudinal study. Jpn J Clin Oncol. 2005. 35:551–558.11. Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, et al. 5-year urinary and sexual outcoms after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005. 173:1701–1705.12. Matsubara A, Yasumoto H, Mutaguchi K, Mita K, Teishima J, Seki M, et al. Impact of radical perineal prostatectomy on urinary continenece and quality of life: a longitudinal study of Japanese patients. Int J Urol. 2005. 12:953–958.13. Desautel MG, Kapoor R, Badlani GH. Sphincteric incontinence: the primary cause of post-prostatectomy incontinence in patients with prostate ca. Neurourol Urodyn. 1997. 16:153–160.14. Ficazzola MA, Nitti VW. The etiology of post-radical prostatectomy incontinence and correlation of symptoms with urodynamic findings. J Urol. 1998. 160:1317–1320.15. Gacci M, Bartoletti R, Figlioli S, Sarti E, Eisner B, Boddi V, et al. Urinary symptoms, quality of life and sexual function in patients with benign prostatic hypertrophy before and after prostatectomy: a prospective study. BJU Int. 2003. 91:196–200.16. McGuire EJ. The role of urodynamic investigation in the assessment of benign prostatic hypertrophy. J Urol. 1992. 148:1133–1136.17. Gomha MA, Boone TB. Voiding patterns in patients with post-prostatectomy incontinence: urodynamic and demographic analysis. J Urol. 2003. 169:1766–1769.18. Hellstorm P, Lukkarinen O, Kontturi M. Urodynamics in radical retropubic prostatectomy. Scand J Urol Nephrol. 1989. 23:21–24.19. Namiki S, Ishidoya S, Saito S, Satoh M, Tochigi T, Ioritani N, et al. Natural history of voiding function after radical retropubic prostatectomy. Urology. 2006. 68:142–147.20. Homma Y, Yamanoguchi T, Kondo Y. Significance of nocturia in the International Prostate Symptom Score for benign prostatic hyperplasia. J Urol. 2002. 167:172–176.21. Namiki S, Saito S, Ishidoya S, Tochigi T, Ioritani N, Yoshimura K, et al. Adverse effect of radical prostatectomy on nocturia and voiding frequency symptom. Urology. 2005. 66:147–151.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improving Urinary Continence after Radical Prostatectomy: Review of Surgical Modifications
- Case of Fournier’s Gangrene in a Patient with Long-Term Indwelling Catheterization due to Urinary Incontinence after Open Radical Prostatectomy
- Clinical implications of underactive bladder
- Characteristics of Mixed Urinary Incontinence and Stress Urinary Incontinence: Relationship between Lower Urinary Tract Symptoms and Urodynamic Parameters
- The Effects of Lower Urinary Tract Symptoms on Depression and Quality of Life among Women in Urban Areas