Intest Res.
2018 Jan;16(1):151-154. 10.5217/ir.2018.16.1.151.
Duodenal amyloidosis secondary to ulcerative colitis
- Affiliations
-
- 1Department of Internal Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. tokimom@nate.com
- KMID: 2402660
- DOI: http://doi.org/10.5217/ir.2018.16.1.151
Abstract
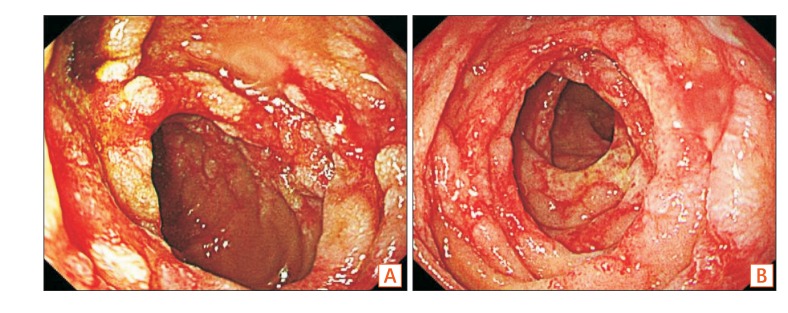
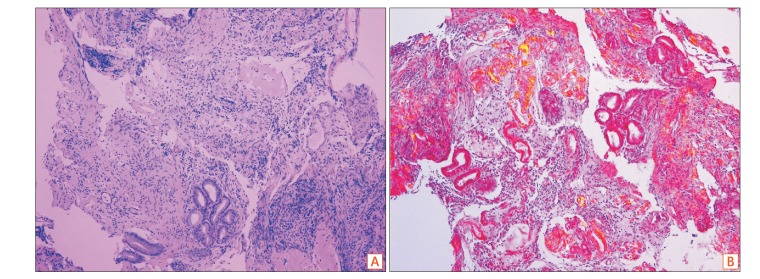
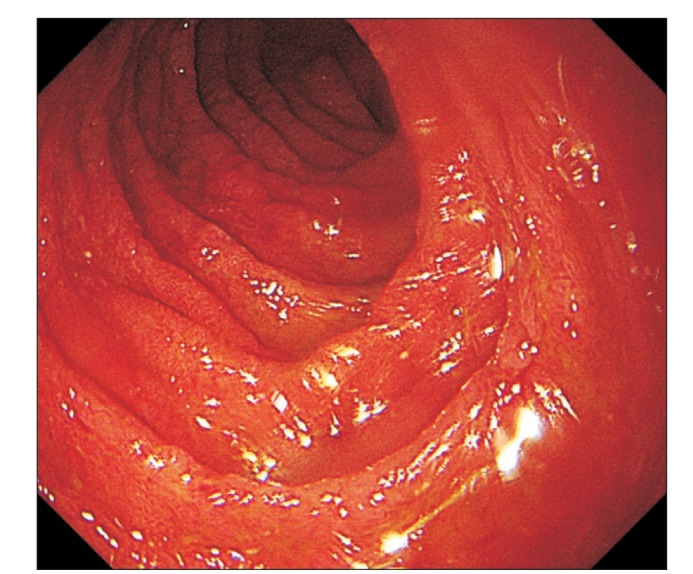
- Amyloidosis is defined as the extracellular deposition of non-branching fibrils composed of a variety of serum-protein precursors. Secondary amyloidosis is associated with several chronic inflammatory conditions, such as rheumatologic or intestinal diseases, familial Mediterranean fever, or chronic infectious diseases, such as tuberculosis. Although the association of amyloidosis with inflammatory bowel disease is known, amyloidosis secondary to ulcerative colitis (UC) is rare. A 36-year-old male patient with a 15-year history of UC presented with nausea, vomiting, and abdominal pain. He had been treated with infliximab for 6 years. At the time of admission, he had been undergoing treatment with mesalazine and adalimumab since the preceding 5 months. Esophagogastroduodenoscopy showed mucosal erythema, edema, and erosions with geographic ulcers at the 2nd and 3rd portions of the duodenum. Duodenal amyloidosis was diagnosed using polarized light microscopy and Congo red stain. Monoclonal gammopathy was not detected in serum and urine tests, while the serum free light chain assay result was not specific. An increase in plasma cells in the bone marrow was not found. Secondary amyloidosis due to UC was suspected. The symptoms were resolved after glucocorticoid therapy.
Keyword
MeSH Terms
-
Abdominal Pain
Adalimumab
Adult
Amyloidosis*
Bone Marrow
Colitis, Ulcerative*
Communicable Diseases
Congo Red
Duodenum
Edema
Endoscopy, Digestive System
Erythema
Familial Mediterranean Fever
Humans
Inflammatory Bowel Diseases
Infliximab
Intestinal Diseases
Male
Mesalamine
Microscopy, Polarization
Nausea
Paraproteinemias
Plasma Cells
Tuberculosis
Ulcer*
Vomiting
Adalimumab
Congo Red
Infliximab
Mesalamine
Figure
Reference
-
1. Lachmann HJ, Goodman HJ, Gilbertson JA, et al. Natural history and outcome in systemic AA amyloidosis. N Engl J Med. 2007; 356:2361–2371. PMID: 17554117.
Article2. Tuglular S, Yalcinkaya F, Paydas S, et al. A retrospective analysis for aetiology and clinical findings of 287 secondary amyloidosis cases in Turkey. Nephrol Dial Transplant. 2002; 17:2003–2005. PMID: 12401861.
Article3. Greenstein AJ, Sachar DB, Panday AK, et al. Amyloidosis and inflammatory bowel disease: a 50-year experience with 25 patients. Medicine (Baltimore). 1992; 71:261–270. PMID: 1522802.
Article4. Serra I, Oller B, Mañosa M, et al. Systemic amyloidosis in inflammatory bowel disease: retrospective study on its prevalence, clinical presentation, and outcome. J Crohns Colitis. 2010; 4:269–274. PMID: 21122515.
Article5. Sattianayagam PT, Hawkins PN, Gillmore JD. Systemic amyloidosis and the gastrointestinal tract. Nat Rev Gastroenterol Hepatol. 2009; 6:608–617. PMID: 19724253.
Article6. Petre S, Shah IA, Gilani N. Review article: gastrointestinal amyloidosis: clinical features, diagnosis and therapy. Aliment Pharmacol Ther. 2008; 27:1006–1016. PMID: 18363891.
Article7. Zemer D, Pras M, Sohar E, Modan M, Cabili S, Gafni J. Colchicine in the prevention and treatment of the amyloidosis of familial Mediterranean fever. N Engl J Med. 1986; 314:1001–1005. PMID: 3515182.
Article8. Gottenberg JE, Merle-Vincent F, Bentaberry F, et al. Anti-tumor necrosis factor alpha therapy in fifteen patients with AA amyloidosis secondary to inflammatory arthritides: a followup report of tolerability and efficacy. Arthritis Rheum. 2003; 48:2019–2024. PMID: 12847696.
Article9. Miyagawa I, Nakayamada S, Saito K, et al. Study on the safety and efficacy of tocilizumab, an anti-IL-6 receptor antibody, in patients with rheumatoid arthritis complicated with AA amyloidosis. Mod Rheumatol. 2014; 24:405–409. PMID: 24252016.
Article10. Dember LM, Hawkins PN, Hazenberg BP, et al. Eprodisate for the treatment of renal disease in AA amyloidosis. N Engl J Med. 2007; 356:2349–2360. PMID: 17554116.
Article11. Jeong YS, Jun JB, Kim TH, et al. Successful treatment of protein-losing enteropathy due to AA amyloidosis with somatostatin analogue and high dose steroid in ankylosing spondylitis. Clin Exp Rheumatol. 2000; 18:619–621. PMID: 11072606.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Secondary Amyloidosis Involving Heart
- Toxic Megacolon Associated with Secondary Amyloidosis: An Unusual Complication of Clostridium difficile Colitis
- A Case of Duodenal Amyloidosis Accompanied with Candidiasis that was Diagnosed by Endoscopy
- A Pediatric Case of Inflammatory Bowel Disease with Renal Amyloidosis
- Ulcerative colitis associated with seropositive rheumatoid arthritis