Korean J Pain.
2018 Jan;31(1):39-42. 10.3344/kjp.2018.31.1.39.
Double blind randomized control trial to evaluate the efficacy of ketoprofen patch to attenuate pain during venous cannulation
- Affiliations
-
- 1Department of Anesthesiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India. drsanjaygupta9@gmail.com
- KMID: 2400906
- DOI: http://doi.org/10.3344/kjp.2018.31.1.39
Abstract
- BACKGROUND
Venipuncture pain is an uncomfortable suffering to the patient. It creates anxiety, fear and dissatisfaction. The ketoprofen transdermal patch is a proven treatment for musculoskeletal and arthritic pain. We planned this study to evaluate the efficacy of the ketoprofen patch to reduce venipuncture pain.
METHODS
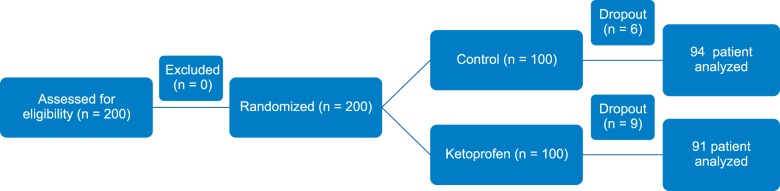
Two hundred adult patients, aged 18-60 years, of either sex, ASA grade I or II, were enrolled. Presuming that therapy would decrease venipuncture pain by 30%, a power calculation with α = 0.05 and β = 0.80 required enrollment of at least 24 patients into each group. However, 100 patients in each group were recruited. Group I (Control) received a placebo patch; Group II (Ketoprofen) received a 20 mg ketoprofen patch. A selected vein on the dorsum of the patient's non-dominant hand was cannulated with 18 g intravenous cannula 1 h after the application of the respective patch. Assessment of pain was done by a 10 cm visual analogue scale (VAS) of 0-10, where 0 depicts "no pain" and 10 is "the worst imaginable pain". The venipuncture site was assessed for the presence of skin erythema, swelling and rashes at 12 h, 24 h and at the time of decannulation.
RESULTS
Incidence of pain was 100% (94/94) in the control group as compared to 93% (85/91) in the ketoprofen group. The severity of the venipuncture pain was 6 (2) and 2 (2) for control and ketoprofen groups respectively (P < 0.05).
CONCLUSIONS
Application of a ketoprofen patch at the proposed site of venipuncture one hour before the attempt is effective and safe for attenuating venipuncture pain.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Topical agents: a thoughtful choice for multimodal analgesia
Eunjoo Choi, Francis Sahngun Nahm, Woong Ki Han, Pyung-Bok Lee, Jihun Jo
Korean J Anesthesiol. 2020;73(5):384-393. doi: 10.4097/kja.20357.
Reference
-
1. Keane TK, Hennis PJ, Bink-Boelkens MT. Non-drug related asystole associated with anaesthetic induction. Anaesthesia. 1991; 46:38–39. PMID: 1996753.
Article2. Hart PS, Yanny W. Needle phobia and malignant vasovagal syndrome. Anaesthesia. 1998; 53:1002–1004. PMID: 9893544.
Article3. Lal MK, McClelland J, Phillips J, Taub NA, Beattie RM. Comparison of EMLA cream versus placebo in children receiving distraction therapy for venepuncture. Acta Paediatr. 2001; 90:154–159. PMID: 11236044.
Article4. Agarwal A, Gautam S, Gupta D, Singh U. Transdermal diclofenac patch vs eutectic mixture of local anesthetics for venous cannulation pain. Can J Anaesth. 2007; 54:196–200. PMID: 17331931.
Article5. Smith AJ, Eggers KA, Stacey MR, Power I. Topical ibuprofen for skin analgesia prior to venepuncture. Anaesthesia. 1996; 51:495–497. PMID: 8694169.
Article6. Agarwal A, Yadav G, Gupta D, Tandon M, Dhiraaj S, Singh PK. Comparative evaluation of myolaxin and EMLA cream for attenuation of venous cannulation pain: a prospective, randomised, double blind study. Anaesth Intensive Care. 2007; 35:726–729. PMID: 17933159.
Article7. Usichenko TI, Pavlovic D, Foellner S, Wendt M. Reducing venipuncture pain by a cough trick: a randomized crossover volunteer study. Anesth Analg. 2004; 98:343–345. PMID: 14742367.
Article8. Agarwal A, Sinha PK, Tandon M, Dhiraaj S, Singh U. Evaluating the efficacy of the valsalva maneuver on venous cannulation pain: a prospective, randomized study. Anesth Analg. 2005; 101:1230–1232. PMID: 16192551.
Article9. Park HJ, Moon DE. Pharmacologic management of chronic pain. Korean J Pain. 2010; 23:99–108. PMID: 20556211.
Article10. Tripathi KD. Essentials of medical pharmacology. 6th ed. New Delhi: Jaypee Brothers;2008. p. 192–193.11. Massey T, Derry S, Moore RA, McQuay HJ. Topical NSAIDs for acute pain in adults. Cochrane Database Syst Rev. 2010; CD007402. PMID: 20556778.
Article12. Komatsu T, Sakurada T. Comparison of the efficacy and skin permeability of topical NSAID preparations used in Europe. Eur J Pharm Sci. 2012; 47:890–895. PMID: 22985876.
Article13. Adachi H, Ioppolo F, Paoloni M, Santilli V. Physical characteristics, pharmacological properties and clinical efficacy of the ketoprofen patch: a new patch formulation. Eur Rev Med Pharmacol Sci. 2011; 15:823–830. PMID: 21780552.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Knee Osteoarthritis with Ketoprofen(Ketotop): A Double-blind Placebo-controlled Randomized Trial
- Contact Dermatitis due to Ketoprofen Patch(Ketotop(R))
- Pretreatmet with 5% lidocaine patch reduces cannula-induced and propofol-induced pain: a randomized, double-blind, placebo-controlled study
- Correspondence to editorial on “Safety and efficacy of HK-660S in patients with primary sclerosing cholangitis: A randomized double-blind phase 2a trial”
- Efficacy and safety of low dose oral ketamine for controlling pain and distress during intravenous cannulation in children: a double-blind, randomized, placebo-controlled trial