Korean J Pain.
2022 Jul;35(3):311-318. 10.3344/kjp.2022.35.3.311.
Efficacy and safety of low dose oral ketamine for controlling pain and distress during intravenous cannulation in children: a double-blind, randomized, placebo-controlled trial
- Affiliations
-
- 1Department of Clinical Pharmacy, School of Pharmacy & Pharmaceutical Sciences, Tehran University of Medical Sciences, Tehran, Iran
- 2Pediatrics Center of Excellence, Children’s Medical Center, Tehran University of Medical Sciences, Tehran, Iran
- 3Department of Anesthesiology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
- 4Non-communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran
- 5Research Group in Community Nutrition and Oxidative Stress and Health Research Institute of the Balearic Islands (IdISBa), University of Balearic Islands, Palma de Mallorca, Spain
- 6CIBER Physiopathology of Obesity and Nutrition (CIBEROBN), Instituto de Salud Carlos III (ISCIII), Madrid, Spain
- KMID: 2530986
- DOI: http://doi.org/10.3344/kjp.2022.35.3.311
Abstract
- Background
Ketamine is widely used in infants and young children for procedural sedation and anesthesia. The aim of this study was to evaluate the efficacy and safety of low dose oral ketamine to control pain and distress in children during intravenous (IV) cannulation.
Methods
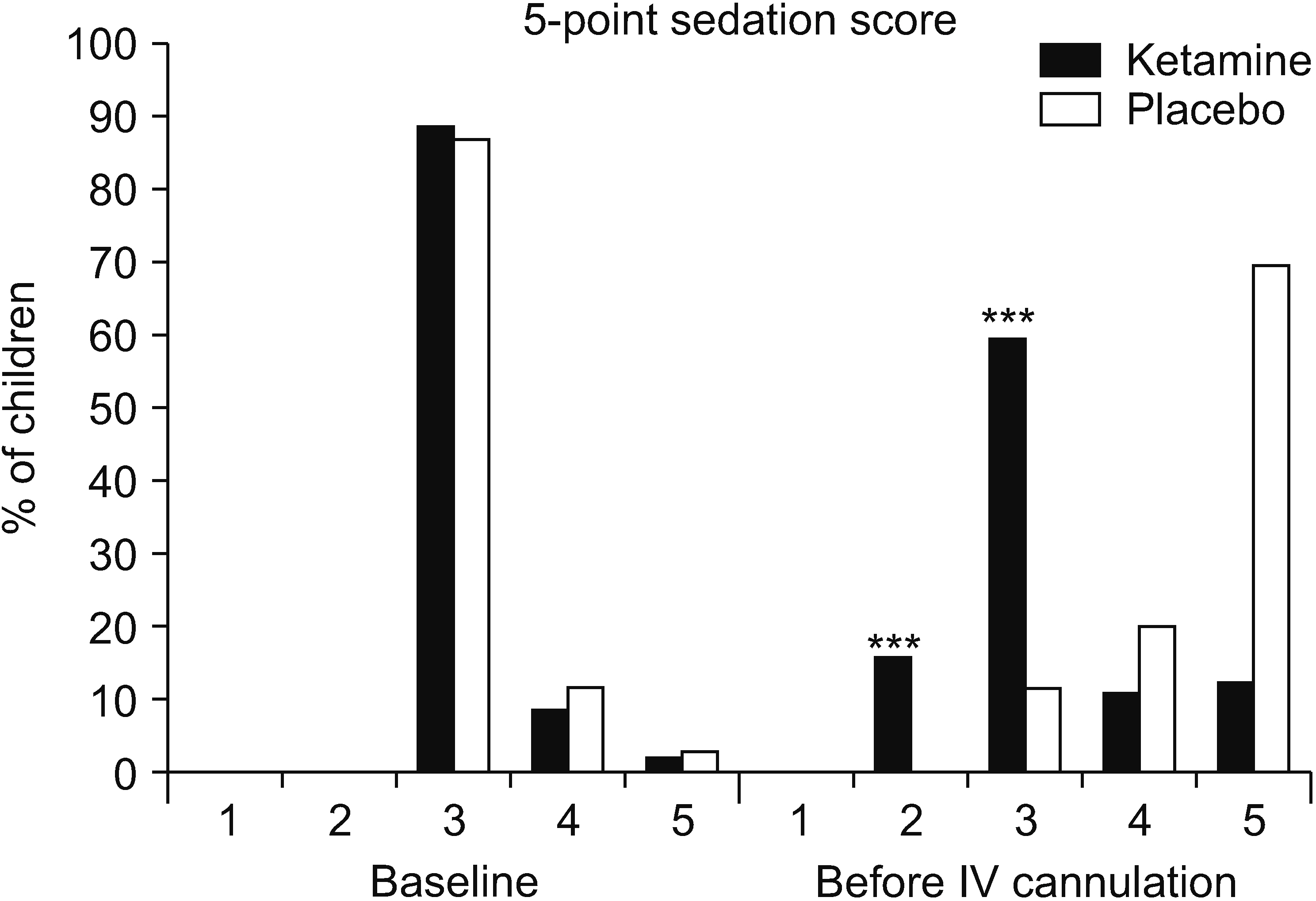
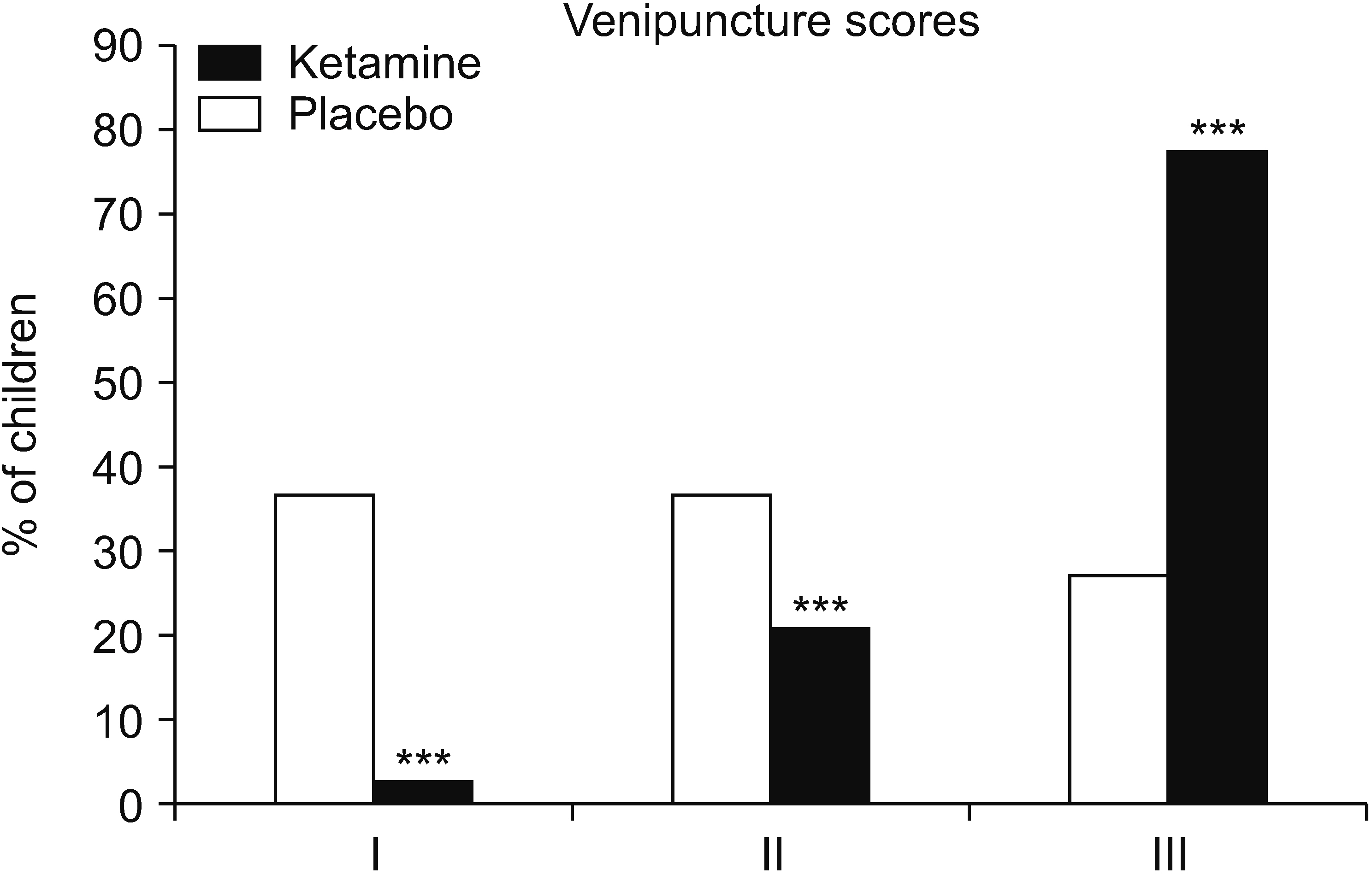
This is a prospective, randomized, double-blind study, including children aged between 3 and 6 years requiring a non-emergent IV-line placement. Children were randomly assigned to two groups, treated either with oral ketamine or a placebo. All patients were monitored for vital signs. Pain was assessed using the Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS) and Wong-Baker Faces Pain Rating Scale (WBFS) scales and sedation using a 5-point sedation score. The facility of IV-line placement was measured by a 3-point scale. Adverse effects were recorded after 1 and 24 hours.
Results
A total of 79 and 81 children were entered in the ketamine and placebo groups, respectively. The heart and respiratory rates increased significantly in the placebo group. The median CHEOPS 4 (95% confidence interval [CI]: 3, 4, P < 0.001) and WBFS 6 (95% CI: 4, 6, P < 0.001) scores decreased statistically in the ketamine group. IV-line placement was 50% easier in the ketamine group (95% CI: 37%, 63%, P < 0.001). No serious adverse effects were observed in all cases.
Conclusions
Low dose oral ketamine effectively decreased the pain and distress during IV cannulation in children without any significant adverse reactions.
Keyword
Figure
Reference
-
1. Blount RL, Piira T, Cohen LL, Cheng PS. 2006; Pediatric procedural pain. Behav Modif. 30:24–49. DOI: 10.1177/0145445505282438. PMID: 16330518.
Article2. Krauss B, Green SM. 2006; Procedural sedation and analgesia in children. Lancet. 367:766–80. DOI: 10.1016/S0140-6736(06)68230-5. PMID: 16517277.
Article3. Fradet C, McGrath PJ, Kay J, Adams S, Luke B. 1990; A prospective survey of reactions to blood tests by children and adolescents. Pain. 40:53–60. DOI: 10.1016/0304-3959(90)91050-S. PMID: 2339016.
Article4. Green SM, Krauss B. 2004; Clinical practice guideline for emergency department ketamine dissociative sedation in children. Ann Emerg Med. 44:460–71. DOI: 10.1016/j.annemergmed.2004.06.006. PMID: 15520705.
Article5. Green SM, Rothrock SG, Harris T, Hopkins GA, Garrett W, Sherwin T. 1998; Intravenous ketamine for pediatric sedation in the emergency department: safety profile with 156 cases. Acad Emerg Med. 5:971–6. DOI: 10.1111/j.1553-2712.1998.tb02773.x. PMID: 9862587.
Article6. Green SM, Rothrock SG, Lynch EL, Ho M, Harris T, Hestdalen R, et al. 1998; Intramuscular ketamine for pediatric sedation in the emergency department: safety profile in 1,022 cases. Ann Emerg Med. 31:688–97. DOI: 10.1016/S0196-0644(98)70226-4. PMID: 9624307.
Article7. Sherwin TS, Green SM, Khan A, Chapman DS, Dannenberg B. 2000; Does adjunctive midazolam reduce recovery agitation after ketamine sedation for pediatric procedures? A randomized, double-blind, placebo-controlled trial. Ann Emerg Med. 35:229–38. DOI: 10.1016/S0196-0644(00)70073-4. PMID: 10692189.
Article8. Sotoodehnia M, Farmahini-Farahani M, Safaie A, Rasooli F, Baratloo A. 2019; Low-dose intravenous ketamine versus intravenous ketorolac in pain control in patients with acute renal colic in an emergency setting: a double-blind randomized clinical trial. Korean J Pain. 32:97–104. DOI: 10.3344/kjp.2019.32.2.97. PMID: 31091508. PMCID: PMC6549592.
Article9. Svenson JE, Abernathy MK. 2007; Ketamine for prehospital use: new look at an old drug. Am J Emerg Med. 25:977–80. DOI: 10.1016/j.ajem.2007.02.040. PMID: 17920984.
Article10. Pasero C, McCaffery M. 2005; Pain control: ketamine: low doses may provide relief for some painful conditions. Am J Nurs. 105:60–4. DOI: 10.1097/00000446-200504000-00028. PMID: 15791081.11. Oyedepo OO, Nasir AA, Abdur-Rahman LO, Kolawole IK, Bolaji BO, Ige OA. 2016; Efficacy and safety of oral ketamine premedication in children undergoing day case surgery. J West Afr Coll Surg. 6:1–15. PMID: 28344934. PMCID: PMC5342622.12. Gutstein HB, Johnson KL, Heard MB, Gregory GA. 1992; Oral ketamine preanesthetic medication in children. Anesthesiology. 76:28–33. DOI: 10.1097/00000542-199201000-00004. PMID: 1729932.
Article13. Rostaminezhad A, Raeis KF, Zandi GK. 2001; A study on oral ketamine premedication effects on preparation of children for surgery. Armaghane Danesh. 6:1–7. https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=53530.14. Oriby ME. 2019; Comparison of intranasal dexmedetomidine and oral ketamine versus intranasal midazolam premedication for children undergoing dental rehabilitation. Anesth Pain Med. 9:e8522. DOI: 10.5812/aapm.85227. PMID: 30881910. PMCID: PMC6412317.
Article15. Soleimanpour H, Mahmoodpoor A, Eftekhari Milani F, Shahsavari Nia K, Mehdizadeh Esfanjani R, Safari S. 2014; Effectiveness of oral ketamine, midazolam, and atropine cocktail versus oral diphenhydramine for pediatric sedation in the emergency department. Iran Red Crescent Med J. 16:e21366. DOI: 10.5812/ircmj.21366. PMID: 25593736. PMCID: PMC4270670.
Article16. Kamel AAF, Amin OAI. 2020; Analgo-sedative effects of oral or nebulized ketamine in preschoolers undergoing elective surgery: a comparative, randomized, double-blind study. Pain Physician. 23:E195–202. DOI: 10.36076/ppj.2020/23/E195. PMID: 32214298.17. Majidinejad S, Taherian K, Esmailian M, Khazaei M, Samaie V. 2015; Oral midazolam-ketamine versus midazolam alone for procedural sedation of children undergoing computed tomography; a randomized clinical trial. Emerg (Tehran). 3:64–9. PMID: 26495384. PMCID: PMC4614601.18. Şekerci C, Dönmez A, AteŞ Y, Ökten F. 1996; Oral ketamine premedication in children (placebo controlled double-blind study). Eur J Anaesthesiol. 13:606–11. DOI: 10.1097/00003643-199611000-00011. PMID: 8958493.
Article19. Kurdi MS, Theerth KA, Deva RS. 2014; Ketamine: Current applications in anesthesia, pain, and critical care. Anesth Essays Res. 8:283–90. DOI: 10.4103/0259-1162.143110. PMID: 25886322. PMCID: PMC4258981.
Article20. Kimiaei Asadi H, Nikooseresht M, Noori L, Behnoud F. 2016; The effect of administration of ketamine and paracetamol versus paracetamol singly on postoperative pain, nausea and vomiting after pediatric adenotonsillectomy. Anesth Pain Med. 6:e31210. DOI: 10.5812/aapm.31210. PMID: 27110529. PMCID: PMC4834744.
Article21. Barkan S, Breitbart R, Brenner-Zada G, Feldon M, Assa A, Toledano M, et al. 2014; A double-blind, randomised, placebo-controlled trial of oral midazolam plus oral ketamine for sedation of children during laceration repair. Emerg Med J. 31:649–53. DOI: 10.1136/emermed-2012-202189. PMID: 23686730.
Article22. Funk W, Jakob W, Riedl T, Taeger K. 2000; Oral preanaesthetic medication for children: double-blind randomized study of a combination of midazolam and ketamine vs midazolam or ketamine alone. Br J Anaesth. 84:335–40. DOI: 10.1093/oxfordjournals.bja.a013435. PMID: 10793592.
Article23. Turhanoğlu S, Kararmaz A, Özyilmaz MA, Kaya S, Tok D. 2003; Effects of different doses of oral ketamine for premedication of children. Eur J Anaesthesiol. 20:56–60. DOI: 10.1097/00003643-200301000-00010. PMID: 12553389.
Article24. Horiuchi T, Kawaguchi M, Kurehara K, Kawaraguchi Y, Sasaoka N, Furuya H. 2005; Evaluation of relatively low dose of oral transmucosal ketamine premedication in children: a comparison with oral midazolam. Paediatr Anaesth. 15:643–7. DOI: 10.1111/j.1460-9592.2004.01513.x. PMID: 16029398.
Article25. Javid MJ, Hajijafari M, Hajipour A, Makarem J, Khazaeipour Z. 2012; Evaluation of a low dose ketamine in post tonsillectomy pain relief: a randomized trial comparing intravenous and subcutaneous ketamine in pediatrics. Anesth Pain Med. 2:85–9. DOI: 10.5812/aapm.4399. PMID: 24223344. PMCID: PMC3821120.
Article26. Hatton RC, Patel J, Low MW, Ganesh O. 2013; Use of oral ketamine by academic hospitals in the US. Ann Pharmacother. 47:591–2. DOI: 10.1345/aph.1S019. PMID: 23512665.
Article27. Kalra P. 2010; Miller's anesthesia, volumes 1 and 2, 7th edition. Anesthesiology. 112:260–1. DOI: 10.1097/ALN.0b013e3181c5dc06.
Article28. Kubota R, Komiyama T, Miwa Y, Bun S, Ishii J, Minei S, et al. 2013; Pharmacokinetics of ketamine and norketamine after oral administration of a liquid formulation of ketamine. J Curr Surg. 3:82–6. https://www.currentsurgery.org/index.php/jcs/article/view/213. DOI: 10.4021/jcs196e.
Article29. Soto E, Stewart DR, Mannes AJ, Ruppert SL, Baker K, Zlott D, et al. 2012; Oral ketamine in the palliative care setting: a review of the literature and case report of a patient with neurofibromatosis type 1 and glomus tumor-associated complex regional pain syndrome. Am J Hosp Palliat Care. 29:308–17. DOI: 10.1177/1049909111416345. PMID: 21803784. PMCID: PMC4239997.30. Ozdemir D, Kayserili E, Arslanoglu S, Gulez P, Vergin C. 2004; Ketamine and midazolam for invasive procedures in children with malignancy: a comparison of routes of intravenous, oral, and rectal administration. J Trop Pediatr. 50:224–8. DOI: 10.1093/tropej/50.4.224. PMID: 15357562.
Article31. Ketamine (Rx). 2022. Medscape Reference [Internet]. Medscape. New York (NY);Available at: https://reference.medscape.com/drug/ketalar-ketamine-343099.32. Tobias JD, Phipps S, Smith B, Mulhern RK. 1992; Oral ketamine premedication to alleviate the distress of invasive procedures in pediatric oncology patients. Pediatrics. 90:537–41. DOI: 10.1542/peds.90.4.537. PMID: 1408506.
Article33. Beebe DS, Belani KG, Chang PN, Hesse PS, Schuh JS, Liao JC, et al. 1992; Effectiveness of preoperative sedation with rectal midazolam, ketamine, or their combination in young children. Anesth Analg. 75:880–4. DOI: 10.1213/00000539-199212000-00003. PMID: 1443705.
Article34. Narendra PL, Naphade RW, Nallamilli S, Mohd S. 2015; A comparison of intranasal ketamine and intranasal midazolam for pediatric premedication. Anesth Essays Res. 9:213–8. DOI: 10.4103/0259-1162.154051. PMID: 26417129. PMCID: PMC4563959.
Article35. Motamed F, Aminpour Y, Hashemian H, Soltani AE, Najafi M, Farahmand F. 2012; Midazolam-ketamine combination for moderate sedation in upper GI endoscopy. J Pediatr Gastroenterol Nutr. 54:422–6. DOI: 10.1097/MPG.0b013e3182323c75. PMID: 21857244.
Article36. Norambuena C, Yañez J, Flores V, Puentes P, Carrasco P, Villena R. 2013; Oral ketamine and midazolam for pediatric burn patients: a prospective, randomized, double-blind study. J Pediatr Surg. 48:629–34. DOI: 10.1016/j.jpedsurg.2012.08.018. PMID: 23480923.
Article37. Qureshi FA, Mellis PT, McFadden MA. 1995; Efficacy of oral ketamine for providing sedation and analgesia to children requiring laceration repair. Pediatr Emerg Care. 11:93–7. DOI: 10.1097/00006565-199504000-00009. PMID: 7596886.
Article38. Jain K, Ghai B, Saxena AK, Saini D, Khandelwal N. 2010; Efficacy of two oral premedicants: midazolam or a low-dose combination of midazolam-ketamine for reducing stress during intravenous cannulation in children undergoing CT imaging. Paediatr Anaesth. 20:330–7. DOI: 10.1111/j.1460-9592.2010.03279.x. PMID: 20470336.
Article39. Green SM, Johnson NE. 1990; Ketamine sedation for pediatric procedures: part 2, review and implications. Ann Emerg Med. 19:1033–46. DOI: 10.1016/S0196-0644(05)82569-7. PMID: 2203290.
Article40. Petrack EM. 2000; Ketamine. Clin Pediatr Emerg Med. 1:281–4. https://doi.org/10.1016/S1522-8401(00)90041-7. DOI: 10.1016/S1522-8401(00)90041-7. PMID: 29532791. PMCID: PMC5999402.
Article41. Visintainer MA, Wolfer JA. 1975; Psychological preparation for surgery pediatric patients: the effects on children's and parents' stress responses and adjustment. Pediatrics. 56:187–202. DOI: 10.1542/peds.56.2.187.
Article42. Schechter NL, Weisman SJ, Rosenblum M, Bernstein B, Conard PL. 1995; The use of oral transmucosal fentanyl citrate for painful procedures in children. Pediatrics. 95:335–9. DOI: 10.1016/0278-2391(95)90146-9. PMID: 7862469.43. Saarnivaara L, Lindgren L, Klemola UM. 1988; Comparison of chloral hydrate and midazolam by mouth as premedicants in children undergoing otolaryngological surgery. Br J Anaesth. 61:390–6. DOI: 10.1093/bja/61.4.390. PMID: 3190970.
Article44. Kil HK, Kim WO, Han SW, Kwon Y, Lee A, Hong JY. 2012; Psychological and behavioral effects of chloral hydrate in day-case pediatric surgery: a randomized, observer-blinded study. J Pediatr Surg. 47:1592–9. DOI: 10.1016/j.jpedsurg.2011.12.025. PMID: 22901923.
Article45. Hamid M, Khan MA, Khatri A, Akhtar I. 2012; Effectiveness of premedication at the time of separation from parent and mask induction in paediatric patients coming for congenital heart disease surgery. J Coll Physicians Surg Pak. 22:280–4. PMID: 22538030.46. Sajid B, Mohamed T, Jumaila M. 2019; A comparison of oral dexmedetomidine and oral midazolam as premedicants in children. J Anaesthesiol Clin Pharmacol. 35:36–40. DOI: 10.4103/joacp.JOACP_20_18. PMID: 31057237. PMCID: PMC6495609.
Article47. Kim KH. 2014; Safe sedation and hypnosis using dexmedetomidine for minimally invasive spine surgery in a prone position. Korean J Pain. 27:313–20. DOI: 10.3344/kjp.2014.27.4.313. PMID: 25317279. PMCID: PMC4196495.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Low-dose intravenous ketamine versus intravenous ketorolac in pain control in patients with acute renal colic in an emergency setting: a double-blind randomized clinical trial
- Effect of low dose ketamine to prevent remifentanil-induced cough: a randomized, double-blind, placebo controlled trial
- Efficacy and Safety of Low-Dose Gamma-Aminobutyric Acid From Unpolished Rice Germ as a Health Functional Food for Promoting Sleep: A Randomized, Double-Blind, Placebo-Controlled Trial
- The Effects of Different Doses of Remifentanil on Propofol Injection Pain: A Placebo Controlled Comparison of Ketamine
- Does Intravenous Ketamine Enhance Analgesia after Arthroscopic Shoulder Surgery with Ultrasound Guided Single-Injection Interscalene Block?: A Randomized, Prospective, Double-Blind Trial