Clin Endosc.
2017 Nov;50(6):609-613. 10.5946/ce.2017.021.
Tranexamic Acid-Induced Acute Renal Cortical Necrosis in Post-Endoscopic Papillectomy Bleeding
- Affiliations
-
- 1Department of Internal Medicine, SAM Anyang Hospital, Anyang, Korea. permi@naver.com
- KMID: 2398315
- DOI: http://doi.org/10.5946/ce.2017.021
Abstract
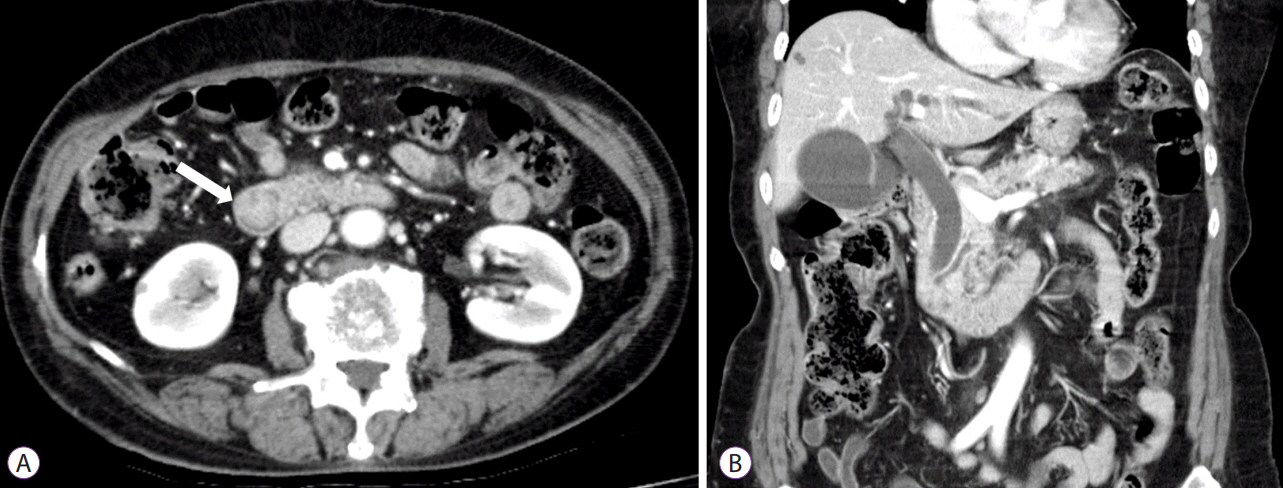
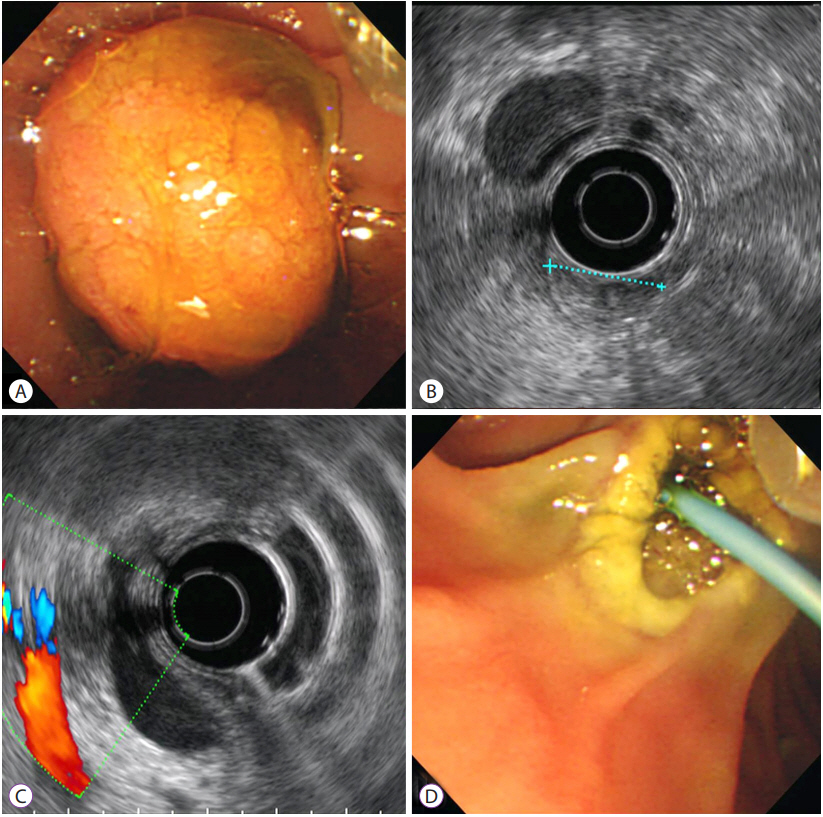
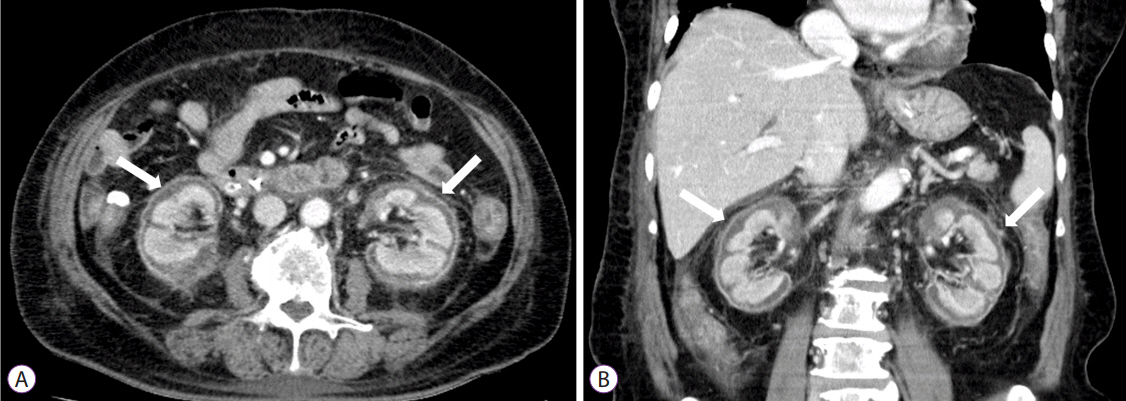
- Acute renal failure can be the result of acute renal cortical necrosis (RCN), which commonly occurs from complications occurring during pregnancy. RCN is rarely caused by medications, although tranexamic acid, which is used in patients with acute bleeding for its antifibrinolytic effects, reportedly causes acute RCN in rare cases. An 82-year-old woman experienced gastrointestinal bleeding after endoscopic papillectomy of an ampullary adenoma. The bleeding was controlled with tranexamic acid administration; however, 4 days later, her urine volume decreased and she developed pulmonary edema and dyspnea. Serum creatinine levels increased from 0.8 to 3.9 mg/dL and dialysis was performed. Abdominal pelvic computed tomography with contrast enhancement revealed bilateral RCN with no renal cortex enhancement. Renal dysfunction and oliguria persisted and hemodialysis was continued. Clinicians must be aware that acute RCN can occur after tranexamic acid administration to control bleeding.
MeSH Terms
Figure
Reference
-
1. Prakash J, Singh VP. Changing picture of renal cortical necrosis in acute kidney injury in developing country. World J Nephrol. 2015; 4:480–486.
Article2. Sahay M, Swain M, Padua M. Renal cortical necrosis in tropics. Saudi J Kidney Dis Transpl. 2013; 24:725–730.
Article3. Kim HJ. Bilateral renal cortical necrosis with the changes in clinical features over the past 15 years (1980-1995). J Korean Med Sci. 1995; 10:132–141.
Article4. Aksoy S, Hocaoglu E, Karahasanoglu A, Igus B, Acay MB, Inci E. Bisphosphonate- induced bilateral acute renal cortical necrosis. Radiol Case Rep. 2015; 10:992.5. British Society of Gastroenterology Endoscopy Committee. Non-variceal upper gastrointestinal haemorrhage: guidelines. Gut. 2002; 51 Suppl 4:iv1–iv6.6. Gluud LL, Klingenberg SL, Langholz E. Tranexamic acid for upper gastrointestinal bleeding. Cochrane Database Syst Rev. 2012; 1:CD006640.
Article7. Mannucci PM. Hemostatic drugs. N Engl J Med. 1998; 339:245–253.
Article8. Koo JR, Lee YK, Kim YS, Cho WY, Kim HK, Won NH. Acute renal cortical necrosis caused by an antifibrinolytic drug (tranexamic acid). Nephrol Dial Transplant. 1999; 14:750–752.
Article9. Levin MD, Betjes MG, V d Kwast TH, Wenberg BL, Leebeek FW. Acute renal cortex necrosis caused by arterial thrombosis during treatment for acute promyelocytic leukemia. Haematologica. 2003; 88:ECR21.10. Odabaş AR, Cetinkaya R, Selçuk Y, Kaya H, Coşkun U. Tranexamic-acid-induced acute renal cortical necrosis in a patient with haemophilia A. Nephrol Dial Transplant. 2001; 16:189–190.
Article11. Park JH, Kang MK, Na WT, et al. A case of bilateral acute renal cortical necrosis complicated by tranexamic acid administration. Korean J Med. 2011; 80:723–728.12. De Palma GD. Endoscopic papillectomy: indications, techniques, and results. World J Gastroenterol. 2014; 20:1537–1543.13. Wang T, Wang DN, Liu WT, et al. Hemostatic effect of topical hemocoagulase spray in digestive endoscopy. World J Gastroenterol. 2016; 22:5831–5836.
Article14. Kim HJ, Cho OK. CT scan as an important diagnostic tool in the initial phase of diffuse bilateral renal cortical necrosis. Clin Nephrol. 1996; 45:125–130.15. Lantsberg S, Rachinsky I, Lupu L, Tovbin D, Hertzanu Y. Unilateral acute renal cortical necrosis: correlative imaging. Clin Nucl Med. 2000; 25:184–186.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Bilateral Acute Renal Cortical Necrosis Complicated by Tranexamic Acid Administration
- A Case of Acute Kidney Cortex Necrosis Caused by Tranexamic-Acid
- Endoscopic Duodenal Snare Papillectomy Induced Complication: Prevention and Management
- The Diagnostic Value of Contrast-Enhanced CT in Acute Bilateral Renal Cortical Necrosis: A Case Report
- Obscure gastrointestinal bleeding in a patient with factor VII deficiency: a case controlled with tranexamic acid