J Adv Prosthodont.
2017 Dec;9(6):423-431. 10.4047/jap.2017.9.6.423.
Load-bearing capacity of various CAD/CAM monolithic molar crowns under recommended occlusal thickness and reduced occlusal thickness conditions
- Affiliations
-
- 1Graduate School of Clinical Dentistry, Ewha Womans University, Seoul, Republic of Korea.
- 2Department of Prosthodontics, School of Dentistry, Seoul National University, Seoul, Republic of Korea. drhiy226@snu.ac.kr
- 3Department of Prosthodontics, School of Medicine, Ewha Womans University, Seoul, Republic of Korea.
- KMID: 2398046
- DOI: http://doi.org/10.4047/jap.2017.9.6.423
Abstract
- PURPOSE
The goal of this study was to evaluate the fracture resistances of various monolithic crowns fabricated by computer-aided design and computer-aided manufacturing (CAD/CAM) with different thickness.
MATERIALS AND METHODS
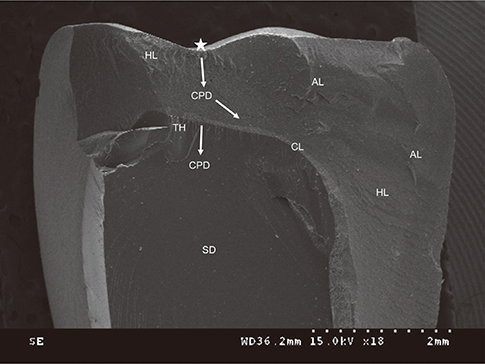
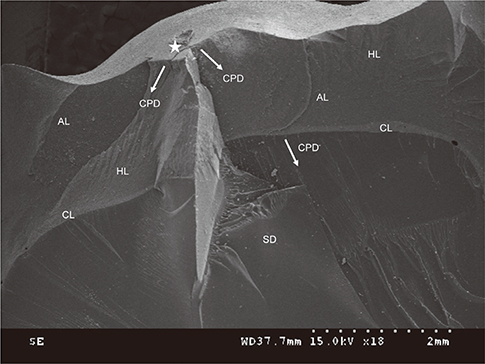
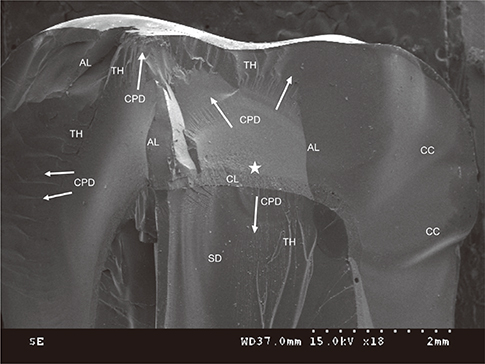
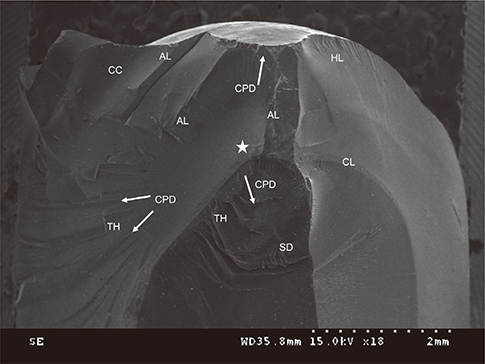
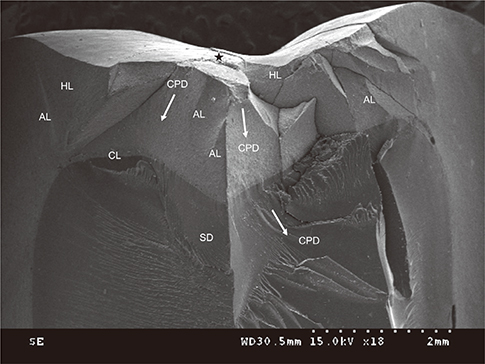
Test dies were fabricated as mandibular molar forms with occlusal reductions using CAD/CAM. With different occlusal thickness (1.0 or 1.5 mm), a polymer-infiltrated ceramic network (Enamic, EN), and zirconia-reinforced lithium silicate (Suprinity, SU and Celtra-Duo, CD) were used to fabricate molar crowns. Lithium disilicate (e.max CAD, EM) crowns (occlusal: 1.5 mm) were fabricated as control. Seventy crowns (n=10 per group) were bonded to abutments and stored in water for 24 hours. A universal testing machine was used to apply load to crown until fracture. The fractured specimens were examined with a scanning electron microscopy.
RESULTS
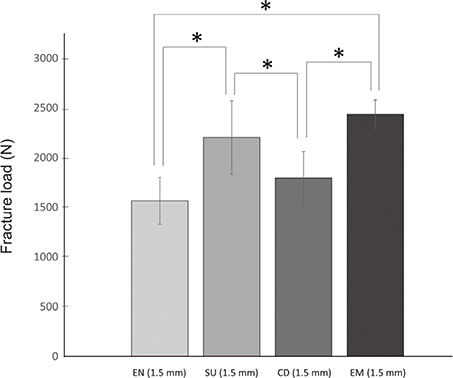
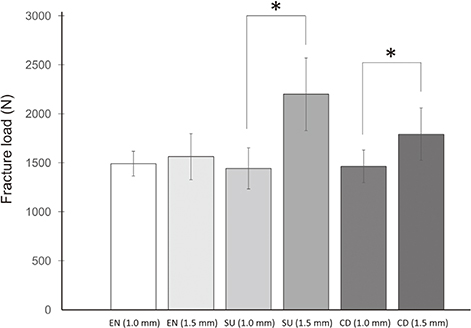
The type of ceramics and the occlusal thickness showed a significant interaction. With a recommended thickness (1.5 mm), the SU revealed the mean load similar to the EM, higher compared with those of the EN and CD. The fracture loads in a reduced thickness (1.0 mm) were similar among the SU, CD, and EN. The mean fracture load of the SU and CD enhanced significantly when the occlusal thickness increased, whereas that of the EN did not.
CONCLUSION
The fracture loads of monolithic crowns were differently influenced by the changes in occlusal thickness, depending on the type of ceramics. Within the limitations of this study, all the tested crowns withstood the physiological masticatory loads both at the recommended and reduced occlusal thickness.
Keyword
MeSH Terms
Figure
Reference
-
1. Wang X, Fan D, Swain MV, Zhao K. A systematic review of all-ceramic crowns: clinical fracture rates in relation to restored tooth type. Int J Prosthodont. 2012; 25:441–450.2. Pjetursson BE, Sailer I, Zwahlen M, Hämmerle CH. A systematic review of the survival and complication rates of allceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: Single crowns. Clin Oral Implants Res. 2007; 18:73–85.3. Raigrodski AJ, Hillstead MB, Meng GK, Chung KH. Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent. 2012; 107:170–177.4. Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater. 2015; 31:603–623.5. Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T. Current status of zirconia restoration. J Prosthodont Res. 2013; 57:236–261.6. Raigrodski AJ, Yu A, Chiche GJ, Hochstedler JL, Mancl LA, Mohamed SE. Clinical efficacy of veneered zirconium dioxide-based posterior partial fixed dental prostheses: five-year results. J Prosthet Dent. 2012; 108:214–222.7. Pieger S, Salman A, Bidra AS. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent. 2014; 112:22–30.8. Agustín-Panadero R, Román-Rodríguez JL, Ferreiroa A, Solá-Ruíz MF, Fons-Font A. Zirconia in fixed prosthesis. A literature review. J Clin Exp Dent. 2014; 6:e66–e73.9. Larsson C, Wennerberg A. The clinical success of zirconiabased crowns: a systematic review. Int J Prosthodont. 2014; 27:33–43.10. Beuer F, Stimmelmayr M, Gueth JF, Edelhoff D, Naumann M. In vitro performance of full-contour zirconia single crowns. Dent Mater. 2012; 28:449–456.11. Denry I, Kelly JR. Emerging ceramic-based materials for dentistry. J Dent Res. 2014; 93:1235–1242.12. Zhao K, Wei YR, Pan Y, Zhang XP, Swain MV, Guess PC. Influence of veneer and cyclic loading on failure behavior of lithium disilicate glass-ceramic molar crowns. Dent Mater. 2014; 30:164–171.13. Guess PC, Zavanelli RA, Silva NR, Bonfante EA, Coelho PG, Thompson VP. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: comparison of failure modes and reliability after fatigue. Int J Prosthodont. 2010; 23:434–442.14. Batson ER, Cooper LF, Duqum I, Mendonça G. Clinical outcomes of three different crown systems with CAD/CAM technology. J Prosthet Dent. 2014; 112:770–777.15. Li RW, Chow TW, Matinlinna JP. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res. 2014; 58:208–216.16. He LH, Swain M. A novel polymer infiltrated ceramic dental material. Dent Mater. 2011; 27:527–534.17. Coldea A, Swain MV, Thiel N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent Mater. 2013; 29:419–426.18. Coldea A, Swain MV, Thiel N. In-vitro strength degradation of dental ceramics and novel PICN material by sharp indentation. J Mech Behav Biomed Mater. 2013; 26:34–42.19. Coldea A, Swain MV, Thiel N. Hertzian contact response and damage tolerance of dental ceramics. J Mech Behav Biomed Mater. 2014; 34:124–133.20. Mörmann WH, Stawarczyk B, Ender A, Sener B, Attin T, Mehl A. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: two-body wear, gloss retention, roughness and Martens hardness. J Mech Behav Biomed Mater. 2013; 20:113–125.21. Coldea A, Fischer J, Swain MV, Thiel N. Damage tolerance of indirect restorative materials (including PICN) after simulated bur adjustments. Dent Mater. 2015; 31:684–694.22. Ankyu S, Nakamura K, Harada A, Hong G, Kanno T, Niwano Y, Örtengren U, Egusa H. Fatigue analysis of computer-aided design/computer-aided manufacturing resinbased composite vs. lithium disilicate glass-ceramic. Eur J Oral Sci. 2016; 124:387–395.23. Zesewitz TF, Knauber AW, Northdurft FP. Fracture resistance of a selection of full-contour all-ceramic crowns: an in vitro study. Int J Prosthodont. 2014; 27:264–266.24. Güncü MB, Cakan U, Muhtarogullari M, Canay S. Zirconiabased crowns up to 5 years in function: a retrospective clinical study and evaluation of prosthetic restorations and failures. Int J Prosthodont. 2015; 28:152–157.25. Kikuchi M, Korioth TW, Hannam AG. The association among occlusal contacts, clenching effort, and bite force distribution in man. J Dent Res. 1997; 76:1316–1325.26. Ferrario VF, Sforza C, Zanotti G, Tartaglia GM. Maximal bite forces in healthy young adults as predicted by surface electromyography. J Dent. 2004; 32:451–457.27. Varga S, Spalj S, Lapter Varga M, Anic Milosevic S, Mestrovic S, Slaj M. Maximum voluntary molar bite force in subjects with normal occlusion. Eur J Orthod. 2011; 33:427–433.28. Wegner LD, Gibson LJ. The fracture toughness behaviour of interpenetrating phase composites. Int J Mech Sci. 2001; 43:1771–1791.29. Thompson VP, Rekow DE. Dental ceramics and the molar crown testing ground. J Appl Oral Sci. 2004; 12:26–36.30. Chen C, Trindade FZ, de Jager N, Kleverlaan CJ, Feilzer AJ. The fracture resistance of a CAD/CAM Resin Nano Ceramic (RNC) and a CAD ceramic at different thicknesses. Dent Mater. 2014; 30:954–962.31. Preis V, Behr M, Hahnel S, Rosentritt M. Influence of cementation on in vitro performance, marginal adaptation and fracture resistance of CAD/CAM-fabricated ZLS molar crowns. Dent Mater. 2015; 31:1363–1369.32. Nordahl N, Vult von, Larsson C. Fracture strength of ceramic monolithic crown systems of different thickness. J Oral Sci. 2015; 57:255–261.33. Schultheis S, Strub JR, Gerds TA, Guess PC. Monolithic and bi-layer CAD/CAM lithium-disilicate versus metal-ceramic fixed dental prostheses: comparison of fracture loads and failure modes after fatigue. Clin Oral Investig. 2013; 17:1407–1413.34. Coelho PG, Bonfante EA, Silva NR, Rekow ED, Thompson VP. Laboratory simulation of Y-TZP all-ceramic crown clinical failures. J Dent Res. 2009; 88:382–386.35. Choi YS, Kim SH, Lee JB, Han JS, Yeo IS. In vitro evaluation of fracture strength of zirconia restoration veneered with various ceramic materials. J Adv Prosthodont. 2012; 4:162–169.36. Harada A, Nakamura K, Kanno T, Inagaki R, Örtengren U, Niwano Y, Sasaki K, Egusa H. Fracture resistance of computer-aided design/computer-aided manufacturing-generated composite resin-based molar crowns. Eur J Oral Sci. 2015; 123:122–129.37. Yucel MT, Yondem I, Aykent F, Eraslan O. Influence of the supporting die structures on the fracture strength of all-ceramic materials. Clin Oral Investig. 2012; 16:1105–1110.38. Dittmer MP, Kohorst P, Borchers L, Stiesch M. Influence of the supporting structure on stress distribution in all-ceramic FPDs. Int J Prosthodont. 2010; 23:63–68.39. Scherrer SS, de Rijk WG. The fracture resistance of all-ceramic crowns on supporting structures with different elastic moduli. Int J Prosthodont. 1993; 6:462–467.40. Chun K, Choi H, Lee J. Comparison of mechanical property and role between enamel and dentin in the human teeth. J Dent Biomech. 2014; 5:1758736014520809.41. Stanford WJ, Paffenbarger GC, Kumpula JW, Sweeney WT. Determination of some compressive properties of human enamel and dentin. J Am Dent Assoc. 1958; 57:487–495.42. Arcís RW, López-Macipe A, Toledano M, Osorio E, Rodríguez-Clemente R, Murtra J, Fanovich MA, Pascual CD. Mechanical properties of visible light-cured resins reinforced with hydroxyapatite for dental restoration. Dent Mater. 2002; 18:49–57.43. Øilo M, Kvam K, Tibballs JE, Gjerdet NR. Clinically relevant fracture testing of all-ceramic crowns. Dent Mater. 2013; 29:815–823.44. Nakamura K, Harada A, Inagaki R, Kanno T, Niwano Y, Milleding P, Ortengren U. Fracture resistance of monolithic zirconia molar crowns with reduced thickness. Acta Odontol Scand. 2015; 73:602–608.45. Johansson C, Kmet G, Rivera J, Larsson C, Vult Von. Fracture strength of monolithic all-ceramic crowns made of high translucent yttrium oxide-stabilized zirconium dioxide compared to porcelain-veneered crowns and lithium disilicate crowns. Acta Odontol Scand. 2014; 72:145–153.46. Sun T, Zhou S, Lai R, Liu R, Ma S, Zhou Z, Longquan S. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J Mech Behav Biomed Mater. 2014; 35:93–101.47. de Kok P, Kleverlaan CJ, de Jager N, Kuijs R, Feilzer AJ. Mechanical performance of implant-supported posterior crowns. J Prosthet Dent. 2015; 114:59–66.48. Seydler B, Rues S, Müller D, Schmitter M. In vitro fracture load of monolithic lithium disilicate ceramic molar crowns with different wall thicknesses. Clin Oral Investig. 2014; 18:1165–1171.49. Campos RE, Soares PV, Versluis A, de O, Ambrosano GM, Nunes IF. Crown fracture: Failure load, stress distribution, and fractographic analysis. J Prosthet Dent. 2015; 114:447–455.50. Harada A, Nakamura K, Kanno T, Inagaki R, Örtengren U, Niwano Y, Sasaki K, Egusa H. Fracture resistance of computer-aided design/computer-aided manufacturing-generated composite resin-based molar crowns. Eur J Oral Sci. 2015; 123:122–129.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of reduced thickness in different regions on the fracture resistance of monolithic zirconia crowns
- Comparison of occusal aspects in monolithic zirconia crown before and after occlusal adjustment during intraoral try-in: a case report
- Fracture strength of zirconia monolithic crowns
- Superimposition: a simple method to minimize occlusal adjustment of monolithic restoration
- Fracture resistance of CAD-CAM all-ceramic surveyed crowns with different occlusal rest seat designs