Asia Pac Allergy.
2011 Jul;1(2):87-92. 10.5415/apallergy.2011.1.2.87.
The clinical effects of hospitalization in a low pollutant room on atopic dermatitis
- Affiliations
-
- 1Department of Pediatrics, Gwangmyeong Sungae Hospital, Gwangmyeong 423-033, Korea.
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. kmaped@skku.edu
- 3Environmental Health Center for Atopic Disease, Samsung Medical Center, Seoul 135-710, Korea.
- 4Department of Pediatrics, Korea Cancer Center Hospital, Seoul 139-706, Korea.
- 5Seoul Research Institute of Public Health & Environment, gwacheon 427-070, Korea.
- KMID: 2397167
- DOI: http://doi.org/10.5415/apallergy.2011.1.2.87
Abstract
- BACKGROUND
Environmental pollutants are thought to be one of major triggers of atopic dermatitis (AD).
OBJECTIVE
We attempted to evaluate the clinical effects of environment with low indoor pollutant levels on AD management.
METHODS
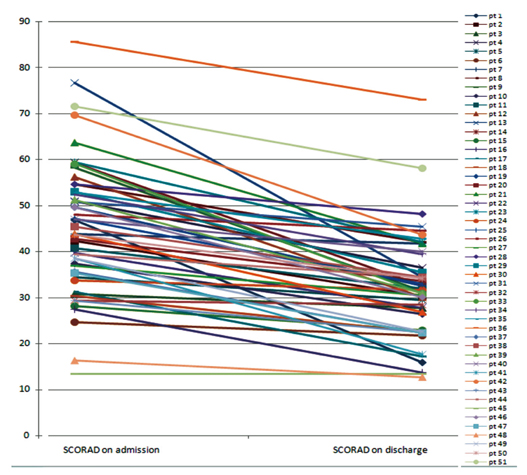
Fifty-one children (mean age 1.7 years) with moderate to severe AD who failed to show improvement with conventional management were recruited. Disease severity was assessed by SCORAD (Scoring of AD) indices. They were admitted in a low pollutant oom for 3-4 days (mean 3.3 days) which was designed to keep low levels of dust, house dust mites, micro-organisms, and indoor air pollutants such as total volatile organic compounds (TVOCs), particulate matter (PM), and so on. Air pollutant levels in the low pollutant room were lower than primary standards defined by the Korean Ministry of Environment. we compared disease severity on admission and after discharge, and the pollutant levels of each patient's home and low pollutant room.
RESULTS
The SCORAD was significantly reduced from 42.0 ± 11 .5 to 29.8 ± 8.9 (p < 0.001) by management in a low pollutant room. PMâ‚‚.â‚…, PMâ‚â‚€, formaldehyde, TVOCs, carbon dioxide, bacterial suspensions, and indoor molds were significantly higher in the patient's home than low pollutant room. Out of 29 patients who deteriorated after discharge to their home, 8 patients were admitted again, and their SCORAD was rapidly decreased from 53.1 ± 16.2 to 39.2 ± 9.8 (p = 0.036).
CONCLUSION
Indoor air pollutants are likely to affect AD in susceptible individuals. Environmental control to lower indoor air pollutant levels might be necessary for better management of AD in some patients.
Keyword
MeSH Terms
-
Air Pollutants
Air Pollution
Carbon Dioxide
Child
Dermatitis, Atopic*
Dust
Environmental Pollutants
Formaldehyde
Fungi
Hospitalization*
Humans
Mites
Particulate Matter
Suspensions
Volatile Organic Compounds
Air Pollutants
Carbon Dioxide
Dust
Environmental Pollutants
Formaldehyde
Particulate Matter
Suspensions
Volatile Organic Compounds
Figure
Cited by 2 articles
-
Early intervention in the management of atopic dermatitis
Donald Y.M. Leung
Asia Pac Allergy. 2011;1(2):51-52. doi: 10.5415/apallergy.2011.1.2.51.Allergic diseases and air pollution
Suh-Young Lee, Yoon-Seok Chang, Sang-Heon Cho
Asia Pac Allergy. 2013;3(3):145-154. doi: 10.5415/apallergy.2013.3.3.145.
Reference
-
1. Williams H, Stewart A, von Mutius E, Cookson W, Anderson HR. International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Groups. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008. 121:947–954.e15.
Article2. Bisgaard H, Halkjaer LB, Hinge R, Giwercman C, Palmer C, Silveira L, Strand M. Risk analysis of early childhood eczema. J Allergy Clin Immunol. 2009. 123:1355–1360.e5.
Article3. Peroni DG, Piacentini GL, Bodini A, Rigotti E, Pigozzi R, Boner AL. Prevalence and risk factors for atopic dermatitis in preschool children. Br J Dermatol. 2008. 158:539–543.
Article4. Purvis DJ, Thompson JM, Clark PM, Robinson E, Black PN, Wild CJ, Mitchell EA. Risk factors for atopic dermatitis in New Zealand children at 3.5 years of age. Br J Dermatol. 2005. 152:742–749.
Article5. Wang IJ, Guo YL, Weng HJ, Hsieh WS, Chuang YL, Lin SJ, Chen PC. Environmental risk factors for early infantile atopic dermatitis. Pediatr Allergy Immunol. 2007. 18:441–447.
Article6. Miyake Y, Ohya Y, Tanaka K, Yokoyama T, Sasaki S, Fukushima W, Ohfuji S, Saito K, Kiyohara C, Hirota Y. Osaka Maternal and Child Health Study Group. Home environment and suspected atopic eczema in Japanese infants: the Osaka Maternal and Child Health Study. Pediatr Allergy Immunol. 2007. 18:425–432.
Article7. Sebök B, Schneider I, Harangi F. Primary Care Paediatricians in Baranya County. Familiar and environmental factors influencing atopic dermatitis in the childhood. J Eur Acad Dermatol Venereol. 2006. 20:418–422.8. McNally NJ, Williams HC, Phillips DR. Atopic eczema and the home environment. Br J Dermatol. 2001. 145:730–736.
Article9. Herbarth O, Fritz GJ, Rehwagen M, Richter m, Röder S, Schlink U. Association between indoor renovation activities and eczema in early childhood. Int J Hyg Environ Health. 2006. 209:241–247.
Article10. Huss-Marp J, Eberlein-König B, Breuer K, Mair S, Ansel A, Darsow U, Krämer U, Mayer E, Ring J, Behrendt H. Influence of short-term exposure to airborne Der p 1 and volatile organic compounds on skin barrier function and dermal blood flow in patients with atopic eczema and healthy individuals. Clin Exp Allergy. 2006. 36:338–345.
Article11. Eberlein-König B, Przybilla B, Kühnl P, Pechak J, Gebefügi I, Kleinschmidt J, Ring J. Influence of airborne nitrogen dioxide or formaldehyde on parameters of skin function and cellular activation in patients with atopic eczema and control subjects. J Allergy Clin Immunol. 1998. 101:141–143.
Article12. Peden DB. The epidemiology and genetics of asthma risk associated with air pollution. J Allergy Clin Immunol. 2005. 115:213–219. quiz 20.
Article13. Leung AD, Schiltz AM, Hall CF, Liu AH. Severe atopic dermatitis is associated with a high burden of environmental Staphylococcus aureus. Clin Exp Allergy. 2008. 38:789–793.
Article14. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh). 1980. 92:44–47.15. Staldera JF, Taïebb A. Consensus Report of the European Task Force on Atopic Dermatitis. Severity scoring of atopic dermatitis: the SCORAD index. Dermatology. 1993. 186:23–31.
Article19. Herberth G, Gubelt R, Röder S, Krämer U, Schins RP, Diez U, Borte M, Heinrich J, Wichmann HE, Herbarth O, Lehmann I. LISAplus study group. Increase of inflammatory markers after indoor renovation activities: the LISA birth cohort study. Pediatr Allergy Immunol. 2009. 20:563–570.
Article20. Lehmann I, Rehwagen M, Diez U, Seiffart A, Rolle-Kampczyk U, Richter M, Wetzig H, Borte M, Herbarth O. Leipzig Allergy Risk Children Study. Enhanced in vivo IgE production and T cell polarization toward the type 2 phenotype in association with indoor exposure to VOC: results of the LARS study. Int J Hyg Environ Health. 2001. 204:211–221.
Article21. Pénard-Morand C, Charpin D, Raherison C, Kopferschmitt C, Caillaud D, Lavaud F, Annesi-Maesano I. Long-term exposure to background air pollution related to respiratory and allergic health in schoolchildren. Clin Exp Allergy. 2005. 35:1279–1287.
Article22. Vocks E, Busch R, Frohlich C, Borelli S, Mayer H, Ring J. Influence of weather and climate on subjective symptom intensity in atopic eczema. Int J Biometeorol. 2001. 45:27–33.
Article23. Yang CY, Cheng MF, Hsieh YL. Effects of indoor environmental factors on risk for atopic eczema in a subtropical area. J Toxicol Environ Health A. 2000. 61:245–253.24. Sator PG, Schmidt JB, Hönigsmann H. Comparison of epidermal hydration and skin surface lipids in healthy individuals and in patients with atopic dermatitis. J Am Acad Dermatol. 2003. 48:352–358.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Measurement of Atopic Dermatitis Disability
- Serum IgE Level in Patients of Atopic Dermatitis and Atopic Dermatitis with Molluscum Contagiosum
- Nipple Involvement in Atopic Dermatitis: Report of 3 cases
- Therapeutic approach to atopic dermatitis in children
- A Clinical Investigation of Patients with Atopic Dermatitis