Ann Pediatr Endocrinol Metab.
2017 Sep;22(3):176-182. 10.6065/apem.2017.22.3.176.
Insulin resistance and bone age advancement in girls with central precocious puberty
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea. hopechae@yuhs.ac
- 2Sowha Children’s Hospital, Seoul, Korea.
- KMID: 2396137
- DOI: http://doi.org/10.6065/apem.2017.22.3.176
Abstract
- PURPOSE
Precocious puberty has significantly increased recently. While obesity is associated with puberty timing, the relationship between obesity and central precocious puberty (CPP) remains controversial. The purpose of this study was to determine whether insulin resistance is associated with bone age (BA) advancement in girls with CPP.
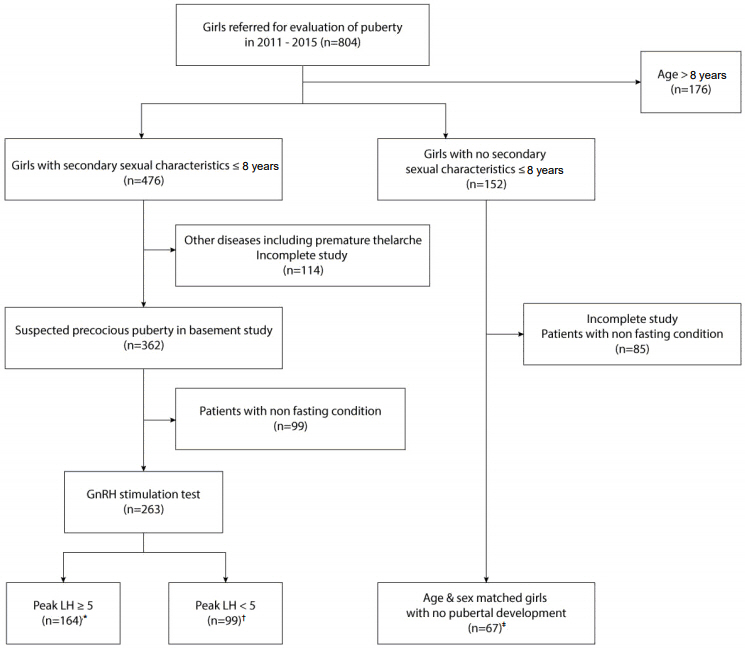
METHODS
We retrospectively analyzed the records of 804 girls referred for puberty evaluation. Anthropometric measurements, BA, sex hormone, sex hormone binding globulin (SHBG), and insulin levels, lipid profiles, and gonadotropin releasing hormone stimulation tests were assessed. Insulin resistance parameters were calculated using the homeostasis model assessment-insulin resistance (HOMA-IR) and quantitative insulin sensitivity check index (QUICKI) models.
RESULTS
BA, BA advancement, free estradiol index, insulin, and HOMA-IR increased significantly in girls with high body mass index (BMI) compared with that of girls with low BMI in cases of CPP. HOMA-IR was positively correlated with BA advancement and BMI but negatively correlated with SHBG. QUICKI was negatively correlated with BA advancement and BMI and positively correlated with SHBG. When HOMA-IR increased by 1, the odds for BA advancement increased 120% after adjusting for age and BMI (P=0.033).
CONCLUSION
Insulin resistance could be associated with BA advancement in girls with CPP.
MeSH Terms
-
Adolescent
Body Mass Index
Estradiol
Female*
Gonadotropin-Releasing Hormone
Homeostasis
Humans
Insulin Resistance*
Insulin*
Luteinizing Hormone
Obesity
Puberty
Puberty, Precocious*
Retrospective Studies
Sex Hormone-Binding Globulin
Estradiol
Gonadotropin-Releasing Hormone
Insulin
Luteinizing Hormone
Sex Hormone-Binding Globulin
Figure
Reference
-
References
1. Sørensen K, Mouritsen A, Aksglaede L, Hagen CP, Mogensen SS, Juul A. Recent secular trends in pubertal timing: implications for evaluation and diagnosis of precocious puberty. Horm Res Paediatr. 2012; 77:137–45.
Article2. Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev. 2003; 24:668–93.
Article3. Park MJ, Lee IS, Shin EK, Joung H, Cho SI. The timing of sexual maturation and secular trends of menarchial age in Korean adolescents. Korean J Pediatr. 2006; 49:610–6.
Article4. Kim SH, Huh K, Won S, Lee KW, Park MJ. A significant increase in the incidence of central precocious puberty among Korean girls from 2004 to 2010. PLoS One. 2015; 10:e0141844.
Article5. Dunger DB, Ahmed ML, Ong KK. Effects of obesity on growth and puberty. Best Pract Res Clin Endocrinol Metab. 2005; 19:375–90.
Article6. Byun SH, Seo WH, Choi BM, Lee KH. The fasting serum glucose, insulin and C-peptide levels in children with obesity. J Korean Soc Pediatr Endocrinol. 2003; 8:73–80.7. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991; 14:173–94.
Article8. Lakshman R, Forouhi NG, Sharp SJ, Luben R, Bingham SA, Khaw KT, et al. Early age at menarche associated with cardiovascular disease and mortality. J Clin Endocrinol Metab. 2009; 94:4953–60.
Article9. Bordini B, Littlejohn E, Rosenfield RL. Blunted sleeprelated luteinizing hormone rise in healthy premenarcheal pubertal girls with elevated body mass index. J Clin Endocrinol Metab. 2009; 94:1168–75.
Article10. Jasik CB, Lustig RH. Adolescent obesity and puberty: the "perfect storm". Ann N Y Acad Sci. 2008; 1135:265–79.11. Sørensen K, Mouritsen A, Mogensen SS, Aksglaede L, Juul A. Insulin sensitivity and lipid profiles in girls with central precocious puberty before and during gonadal suppression. J Clin Endocrinol Metab. 2010; 95:3736–44.
Article12. Hillman JB, Huang B, Pinney SM, Biro FM. Early pubertal development and insulin sensitivity among school-aged girls: mediation via adiposity. J Pediatr Adolesc Gynecol. 2013; 26:47–50.
Article13. Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969; 44:291–303.
Article14. Korea Centers for Disease Control and Prevention. 2005 Korean children and adolescents growth standard: commentary for the development of 2005 growth chart. Cheongju: Korea Centers for Disease Control and Prevention;2005.15. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–9.
Article16. Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000; 85:2402–10.
Article17. Biro FM, Khoury P, Morrison JA. Influence of obesity on timing of puberty. Int J Androl. 2006; 29:272–7.
Article18. Zimmerman PA, Francis GL, Poth M. Hormone-containing cosmetics may cause signs of early sexual development. Mil Med. 1995; 160:628–30.
Article19. Gladen BC, Ragan NB, Rogan WJ. Pubertal growth and development and prenatal and lactational exposure to polychlorinated biphenyls and dichlorodiphenyl dichloroethene. J Pediatr. 2000; 136:490–6.
Article20. He Q, Karlberg J. BMI in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001; 49:244–51.
Article21. Kliegman RM, Stanton BF, St. Geme JW III, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia (PA): Elsevier Saunders;2011.22. Møller N, Jørgensen JO. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr Rev. 2009; 30:152–77.
Article23. Sørensen K, Aksglaede L, Petersen JH, Andersson AM, Juul A. Serum IGF1 and insulin levels in girls with normal and precocious puberty. Eur J Endocrinol. 2012; 166:903–10.
Article24. Friedrich N, Thuesen B, Jørgensen T, Juul A, Spielhagen C, Wallaschofksi H, et al. The association between IGF-I and insulin resistance: a general population study in Danish adults. Diabetes Care. 2012; 35:768–73.25. Södergård R, Bäckström T, Shanbhag V, Carstensen H. Calculation of free and bound fractions of testosterone and estradiol-17 beta to human plasma proteins at body temperature. J Steroid Biochem. 1982; 16:801–10.26. Chae HW, Kwon AR, Kim DH, Kim HS. Sex hormone binding globulin, free estradiol index, and lipid profiles in girls with precocious puberty. Ann Pediatr Endocrinol Metab. 2013; 18:81–4.
Article27. Ahmed ML, Ong KK, Dunger DB. Childhood obesity and the timing of puberty. Trends Endocrinol Metab. 2009; 20:237–42.
Article28. Kaplowitz PB. Link between body fat and the timing of puberty. Pediatrics. 2008; 121 Suppl 3:S208–17.
Article29. Kolaczynski JW, Nyce MR, Considine RV, Boden G, Nolan JJ, Henry R, et al. Acute and chronic effects of insulin on leptin production in humans: Studies in vivo and in vitro. Diabetes. 1996; 45:699–701.
Article30. Flor-Cisneros A, Roemmich JN, Rogol AD, Baron J. Bone age and onset of puberty in normal boys. Mol Cell Endocrinol. 2006; 254-255:202–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Biochemical Factors Associated with GnRH Stimulation test in the Idiopathic Central Precocious Puberty and Early Puberty Girls
- Etiology and Age Incidence of Precocious Puberty
- Serum IGF-1 and IGFBP-3 Levels in Central Precocious Puberty Girls Treated with Gonadotropin Releasing Hormone Agonist (GnRHa)
- Slower progression of central puberty in overweight girls presenting with precocious breast development
- The difference in serum alkaline phosphatase levels between girls with precocious puberty and those with normal puberty