Clin Exp Otorhinolaryngol.
2017 Sep;10(3):241-247. 10.21053/ceo.2016.01732.
A Study of Single Nucleotide Polymorphisms of Tumour Necrosis Factor α-1031 And Tumour Necrosis Factor β+ 252 in Chronic Rhinosinusitis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head & Neck Surgery, School of Medical Sciences, Universiti Sains Malaysia Health Campus, Kelantan, Malaysia.
- 2Basic Science and Oral Biology Unit, School of Dental Sciences, Universiti Sains Malaysia Health Campus, Kelantan, Malaysia.
- KMID: 2395738
- DOI: http://doi.org/10.21053/ceo.2016.01732
Abstract
OBJECTIVES
This case-controlled study aimed to identify the association of tumor necrosis factor (TNF)α-1031 and TNFβ+ 252 gene polymorphisms between chronic rhinosinusitis (CRS) and healthy controls. Another purpose of this study was to investigate the associations of these gene polymorphisms with factors related to CRS.
METHODS
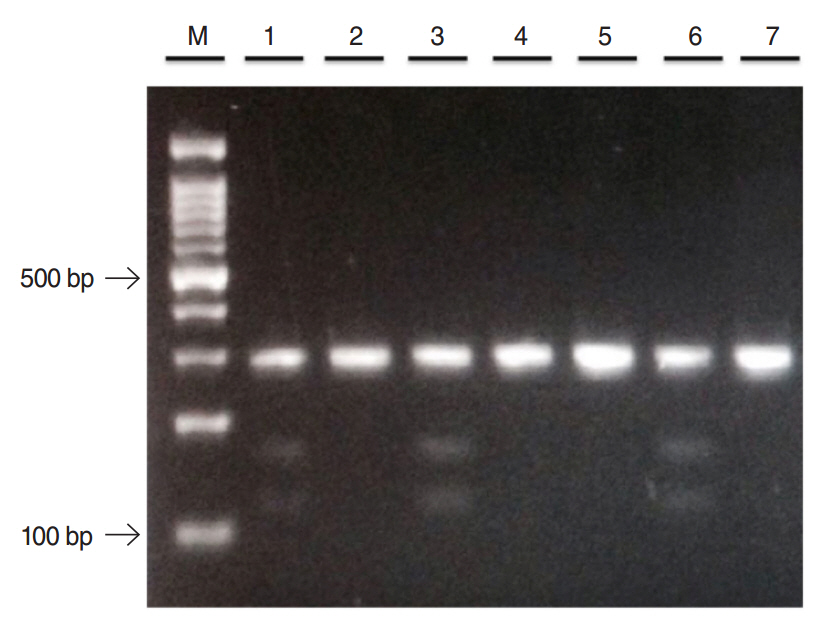
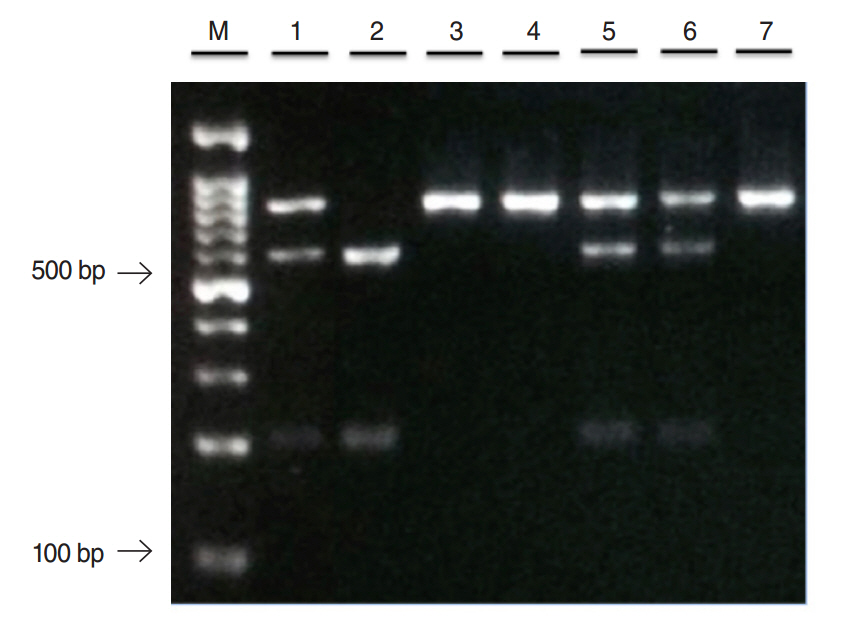
All deoxyribonucleic acid (DNA) samples were genotyped for TNFα-1031 and TNFβ+252 genes by mean of polymerase chain reaction (PCR) and restriction fragment length polymorphisms (RFLP). The statistical analysis were carried out using chi-square test or Fisher exact test to determine the associations of these gene polymorphisms in CRS. Multiple logistic regression was performed to evaluate the associations of these gene polymorphisms in CRS and its related risk factors.
RESULTS
The genotype and allele frequencies of TNFα-1031 and TNFβ+252 gene did not show any significant associations between CRS and healthy controls. However, a significantly statistical difference of TNFα-1031 was observed in CRS participants with atopy (P-value, 0.045; odds ratio, 3.66) but not in CRS with asthma or aspirin intolerance.
CONCLUSION
Although the presence of TNFα-1031 and TNFβ+252 gene polymorphisms did not render any significant associations between CRS and healthy control, this study suggests that TNFα-1031 gene polymorphisms in CRS patients with atopy may be associated with increase susceptibility towards CRS.
MeSH Terms
Figure
Cited by 2 articles
-
Association of
IL-1 gene polymorphisms with chronic rhinosinusitis with and without nasal polyp
Sakinah Mohamad, Suzina Sheikh Ab Hamid, Ahmad Azlina, Norasnieda Md Shukri
Asia Pac Allergy. 2019;9(3):e22. doi: 10.5415/apallergy.2019.9.e22.Association of
IL-1 gene polymorphisms with chronic rhinosinusitis with and without nasal polyp
Sakinah Mohamad, Suzina Sheikh Ab Hamid, Ahmad Azlina, Norasnieda Md Shukri
Asia Pac Allergy. 2019;9(3):. doi: 10.5415/apallergy.2019.9.e22.
Reference
-
1. Hastan D, Fokkens WJ, Bachert C, Newson RB, Bislimovska J, Bockelbrink A, et al. Chronic rhinosinusitis in Europe: an underestimated disease: a GA²LEN study. Allergy. 2011; Sep. 66(9):1216–23.2. Pearlman AN, Chandra RK, Chang D, Conley DB, Tripathi-Peters A, Grammer LC, et al. Relationships between severity of chronic rhinosinusitis and nasal polyposis, asthma, and atopy. Am J Rhinol Allergy. 2009; Mar-Apr. 23(2):145–8.
Article3. Chen Y, Dales R, Lin M. The epidemiology of chronic rhinosinusitis in Canadians. Laryngoscope. 2003; Jul. 113(7):1199–205.
Article4. Johansson L, Akerlund A, Holmberg K, Melen I, Bende M. Prevalence of nasal polyps in adults: the Skovde population-based study. Ann Otol Rhinol Laryngol. 2003; Jul. 112(7):625–9.
Article5. Settipane GA. Epidemiology of nasal polyps. Allergy Asthma Proc. 1996; Sep-Oct. 17(5):231–6.
Article6. Aggarwal BB, Gupta SC, Kim JH. Historical perspectives on tumor necrosis factor and its superfamily: 25 years later, a golden journey. Blood. 2012; Jan. 119(3):651–65.
Article7. Aggarwal BB. SNPs: why do we care?. In : Kwok PY, editor. Single nucleotide polymorphisms: methods and protocols. Totowa (NJ): Humana Press;2003. p. 1–14.8. Qidwai T, Khan F. Tumour necrosis factor gene polymorphism and disease prevalence. Scand J Immunol. 2011; Dec. 74(6):522–47.
Article9. Sashio H, Tamura K, Ito R, Yamamoto Y, Bamba H, Kosaka T, et al. Polymorphisms of the TNF gene and the TNF receptor superfamily member 1B gene are associated with susceptibility to ulcerative colitis and Crohn’s disease, respectively. Immunogenetics. 2002; Mar. 53(12):1020–7.10. Li HQ, Li Z, Liu Y, Li JH, Dong JQ, Gao JR, et al. Association of-238G/A and -857C/T polymorphisms of tumor necrosis factor-alpha gene promoter region with outcomes of hepatitis B virus infection. Biomed Environ Sci. 2006; Apr. 19(2):133–6.11. Oregon-Romero E, Vazquez-Del Mercado M, Ruiz-Quezada SL, Navarro-Hernandez RE, Rangel-Villalobos H, Martinez-Bonilla G, et al. Tumor necrosis factor alpha-308 and -238 polymorphisms in rheumatoid arthritis: association with messenger RNA expression and sTNF-alpha. J Investig Med. 2008; Oct. 56(7):937–43.12. Seymour HE, Worsley A, Smith JM, Thomas SH. Anti-TNF agents for rheumatoid arthritis. Br J Clin Pharmacol. 2001; Mar. 51(3):201–8.
Article13. Takeuchi K, Majima Y, Sakakura Y. Tumor necrosis factor gene polymorphism in chronic sinusitis. Laryngoscope. 2000; Oct. 110(10 Pt 1):1711–4.
Article14. Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012: a summary for otorhinolaryngologists. Rhinology. 2012; Mar. 50(1):1–12.
Article15. Bonyadi M, Abdolmohammadi R, Jahanafrooz Z, Somy MH, Khoshbaten M. TNF-alpha gene polymorphisms in Iranian Azari Turkish patients with inflammatory bowel diseases. Saudi J Gastroenterol. 2014; Mar-Apr. 20(2):108–12.
Article16. Daly AK, Day CP. Candidate gene case-control association studies: advantages and potential pitfalls. Br J Clin Pharmacol. 2001; Nov. 52(5):489–99.
Article17. Huvenne W, van Bruaene N, Zhang N, van Zele T, Patou J, Gevaert P, et al. Chronic rhinosinusitis with and without nasal polyps: what is the difference. Curr Allergy Asthma Rep. 2009; May. 9(3):213–20.
Article18. Shkoukani MA, Krouse JH. The role of atopy and asthma status in chronic rhinosinusitis in adults. J Otol Rhinol. 2013; 2(3):https://doi.org/10.4172/2324-8785.1000122.
Article19. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011; Oct. 128(4):693–707.
Article20. Oakley GM, Curtin K, Orb Q, Schaefer C, Orlandi RR, Alt JA. Familial risk of chronic rhinosinusitis with and without nasal polyposis: genetics or environment. Int Forum Allergy Rhinol. 2015; Apr. 5(4):276–82.
Article21. Erbek SS, Yurtcu E, Erbek S, Atac FB, Sahin FI, Cakmak O. Proinflammatory cytokine single nucleotide polymorphisms in nasal polyposis. Arch Otolaryngol Head Neck Surg. 2007; 133(7):705–9.
Article22. Bernstein JM, Anon JB, Rontal M, Conroy J, Wang C, Sucheston L. Genetic polymorphisms in chronic hyperplastic sinusitis with nasal polyposis. Laryngoscope. 2009; Jul. 119(7):1258–64.
Article23. Batikhan H, Gokcan MK, Beder E, Akar N, Ozturk A, Gerceker M. Association of the tumor necrosis factor-alpha -308 G/A polymorphism with nasal polyposis. Eur Arch Otorhinolaryngol. 2010; Jun. 267(6):903–8.
Article24. Fajardo-Dolci G, Solorio-Abreu J, Romero-Alvarez JC, Zavaleta-Villa B, Cerezo-Camacho O, Jimenez-Lucio R, et al. DQA1 and DQB1 association and nasal polyposis. Otolaryngol Head Neck Surg. 2006; Aug. 135(2):243–7.
Article25. Mfuna Endam L, Cormier C, Bosse Y, Filali-Mouhim A, Desrosiers M. Association of IL1A, IL1B, and TNF gene polymorphisms with chronic rhinosinusitis with and without nasal polyposis: a replication study. Arch Otolaryngol Head Neck Surg. 2010; Feb. 136(2):187–92.26. Szabo K, Kiricsi A, Revesz M, Vona I, Szabo Z, Bella Z, et al. The -308 G>A SNP of TNFA is a factor predisposing to chronic rhinosinusitis associated with nasal polyposis in aspirin-sensitive Hungarian individuals: conclusions of a genetic study with multiple stratifications. Int Immunol. 2013; Jun. 25(6):383–8.27. Berghea EC, Popa OM, Meirosu M, Popa LO, Bara C, Bumbacea RS. Association of TNF-alpha gene polymorphism with nasal polyposis in Romanian asthmatic patients. Rom J Rhinol. 2014; Sep. 4(15):149–55.28. Bohonak AJ. Genetic drift in human populations. In: Encyclopedia of life sciences. Chichester, UK: John Wiley & Son. 2008. http://doi.org/10.1002/9780470015902.a0005440.pub2.
Article29. Pawankar R, Nonaka M. Inflammatory mechanisms and remodeling in chronic rhinosinusitis and nasal polyps. Curr Allergy Asthma Rep. 2007; Jun. 7(3):202–8.
Article30. Jiffri EH, Elhawary NA. Association between β+252 tumour necrosis factor polymorphism and asthma in western Saudi children. Saudi J Biol Sci. 2011; Jan. 18(1):107–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tumour Regression via Integrative Regulation of Neurological, Inflammatory, and Hypoxic Tumour Microenvironment
- Interleukin-10 and Tumor Necrosis Factor-alpha Polymorphisms in Vascular Access Failure in Patients on Hemodialysis: Preliminary Data in Korea
- No Association between Tumor Necrosis Factor-alpha Gene Polymorphisms and Lung Cancer Risk
- Association of TNFA Promoter Region Haplotype in Behcet's Disease
- Polymorphisms of the 5'-Flanking Region of the Human Tumor Necrosis Factor-alpha Gene in Korean Patients with Crohn's Disease