J Breast Cancer.
2011 Sep;14(3):175-180.
Can CD44+/CD24- Tumor Cells Be Used to Determine the Extent of Breast Cancer Invasion Following Neoadjuvant Chemotherapy?
- Affiliations
-
- 1The Second Bethune Hospital of Jilin University, Changchun, China.
- 2The First Bethune Hospital of Jilin University, Changchun, China. angel-s205@163.com
- 3Jilin Medical College, Changchun, China.
Abstract
- PURPOSE
To investigate the distribution of CD44+/CD24- cells in breast cancers in relation to tumor size before and after the administration of neoadjuvant chemotherapy.
METHODS
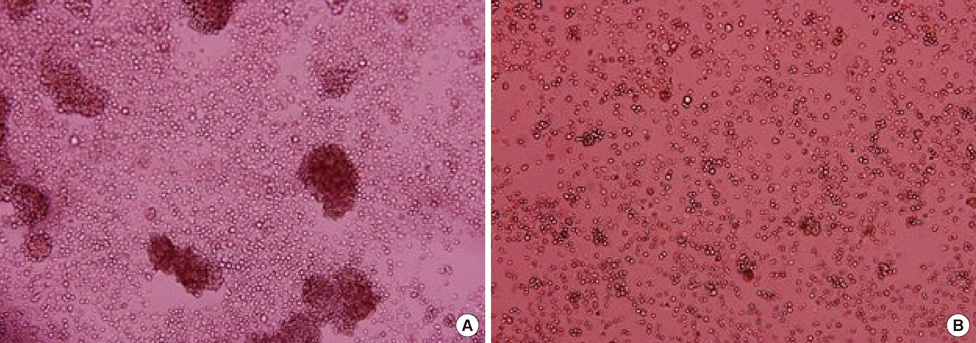
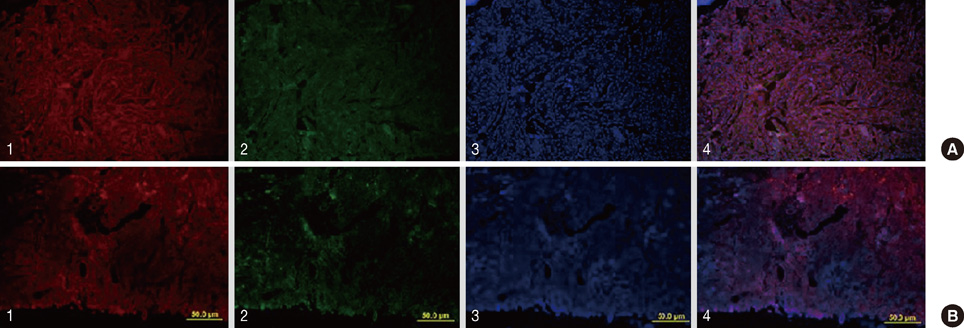
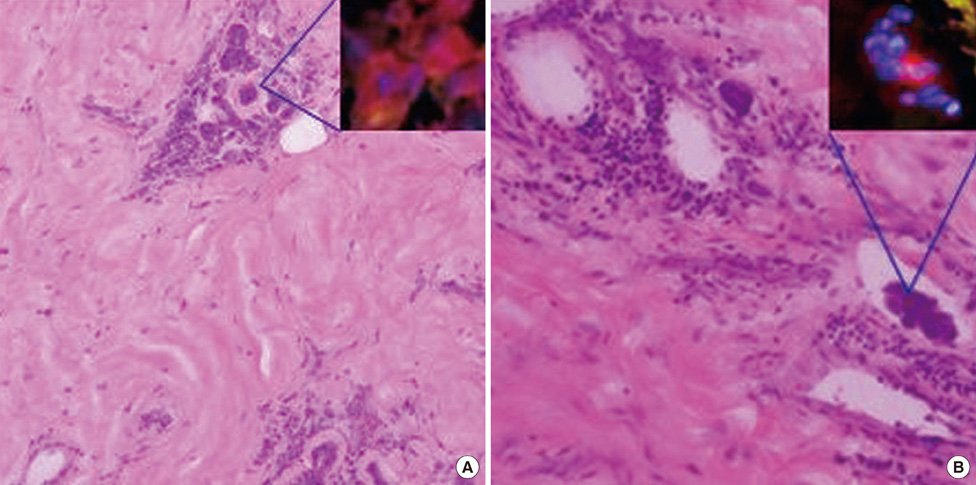
CD44+/CD24- tumor cells obtained from breast cancer specimens were characterized in vivo and in vitro using tumor formation assays and mammosphere generation assays, respectively. The distribution of CD44+/CD24- tumor cells in 78 breast cancer specimens following administration of neoadjuvant chemotherapy was also evaluated using immunofluorescence assays, and this distribution was compared with the extent of tumor invasion predicted by Response Evaluation Criteria in Solid Tumours (RECIST).
RESULTS
In 27/78 cases, complete remission (CR) was identified using RECIST. However, 18 of these CR cases were associated with a scattered distribution of tumor stem cells in the outline of the original tumor prior to neoadjuvant chemotherapy. After neoadjuvant chemotherapy, 24 cases involved cancer cells that were confined to the tumor outline, and 21 cases had tumor cells or tumor stem cells overlapping the tumor outline. In addition, there were 6 patients who were insensitive to chemotherapy, and in these cases, both cancer cells and stem cells were detected outside the contours of the tumor volume imaged prior to chemotherapy.
CONCLUSION
CD44+/CD24- tumor cells may be an additional parameter to evaluate when determining the extent of breast cancer invasion.
MeSH Terms
Figure
Reference
-
1. Lyall D, Schwartz M, Herter FP, Hudson PB, Wright JC, Findlay CW, et al. Treatment of cancer by the method of Revici. JAMA. 1965. 194:279–280.
Article2. Chong HY, Taib NA, Rampal S, Saad M, Bustam AZ, Yip CH. Treatment options for locally advanced breast cancer--experience in an Asian tertiary hospital. Asian Pac J Cancer Prev. 2010. 11:913–917.3. Siponen ET, Vaalavirta L, Joensuu H, Vironen J, Heikkilä P, Leidenius MH. Ipsilateral breast recurrence after breast conserving surgery in patients with small (≤ 2 cm) breast cancer treated with modern adjuvant therapies. Eur J Surg Oncol. 2011. 37:25–31.
Article4. Smith BD, Buchholz TA, Kuerer HM. Intraoperative radiotherapy for early breast cancer. Lancet. 2010. 376:1141.
Article5. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009. 45:228–247.
Article6. Linton KM, Taylor MB, Radford JA. Response evaluation in gastrointestinal stromal tumours treated with imatinib: misdiagnosis of disease progression on CT due to cystic change in liver metastases. Br J Radiol. 2006. 79:e40–e44.
Article7. Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A. 2003. 100:3983–3988.
Article8. Pece S, Tosoni D, Confalonieri S, Mazzarol G, Vecchi M, Ronzoni S, et al. Biological and molecular heterogeneity of breast cancers correlates with their cancer stem cell content. Cell. 2010. 140:62–73.
Article9. Tanei T, Morimoto K, Shimazu K, Kim SJ, Tanji Y, Taguchi T, et al. Association of breast cancer stem cells identified by aldehyde dehydrogenase 1 expression with resistance to sequential paclitaxel and epirubicin-based chemotherapy for breast cancers. Clin Cancer Res. 2009. 15:4234–4241.
Article10. Liu S, Wicha MS. Targeting breast cancer stem cells. J Clin Oncol. 2010. 28:4006–4012.
Article11. Yi M, Buchholz TA, Meric-Bernstam F, Bedrosian I, Hwang RF, Ross MI, et al. Classification of ipsilateral breast tumor recurrences after breast conservation therapy can predict patient prognosis and facilitate treatment planning. Ann Surg. 2011. 253:572–579.
Article12. Shin HJ, Kim HH, Ahn JH, Kim SB, Jung KH, Gong G, et al. Comparison of mammography, sonography, MRI and clinical examination in patients with locally advanced or inflammatory breast cancer who underwent neoadjuvant chemotherapy. Br J Radiol. 2011. 84:612–620.
Article13. Nakshatri H. Radiation resistance in breast cancer: are CD44+/CD24-/proteosome low/PKH26+ cells to blame? Breast Cancer Res. 2010. 12:105.14. Oliveira LR, Jeffrey SS, Ribeiro-Silva A. Stem cells in human breast cancer. Histol Histopathol. 2010. 25:371–385.15. Kakarala M, Wicha MS. Implications of the cancer stem-cell hypothesis for breast cancer prevention and therapy. J Clin Oncol. 2008. 26:2813–2820.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Invited Commentary on: Can CD44+/CD24- Tumor Stem Cells Be Used to Determine the Extent of Breast Cancer Invasion Following Neoadjuvant Chemotherapy?
- Clinicopathological Significance of Invasive Ductal Carcinoma with High Prevalence of CD44(+)/CD24(-/low) Tumor Cells in Breast Cancer
- Effect of bFGF on the MCF-7 Cell Cycle with CD44+/CD24-: Promoting the G0/G1-->G2/S Transition
- New Findings on Breast Cancer Stem Cells: A Review
- Changes of Tumor-infiltrating Lymphocytes in Breast Cancer after Neoadjuvant Chemotherapy