Lab Med Online.
2017 Oct;7(4):163-169. 10.3343/lmo.2017.7.4.163.
Evaluation of the Automated Immunohematology Analyzer DAYMATE M
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul St. Mary's Hospital, Seoul, Korea. yonggoo@catholic.ac.kr
- 2Department of Laboratory Medicine, Incheon St. Mary's Hospital, Incheon, Korea. bonokarl@catholic.ac.kr
- 3Laboratory for Development and Evaluation Center, The Catholic University of Korea, Seoul, Korea.
- KMID: 2389655
- DOI: http://doi.org/10.3343/lmo.2017.7.4.163
Abstract
- BACKGROUND
An automated immunohematology analyzer, DAYMATE M (DAY Medical, Switzerland), has been recently developed. The potential of this analyzer to improve test results has been evaluated.
METHODS
A total of 300 blood samples from Seoul St. Mary's hospital and Incheon St. Mary's hospital were tested for ABO and RhD typing. In addition, 336 antibody screening test (AST) samples and 82 patients treated with hematopoietic stem cell transplantation (HSCT) were included. AST results by DAYMATE M were compared with those obtained by a manual method using DS-Screening II (Bio-Rad Laboratories, Switzerland) and red blood cells from Selectogen (Ortho-Clinical diagnostics Inc., USA).
RESULTS
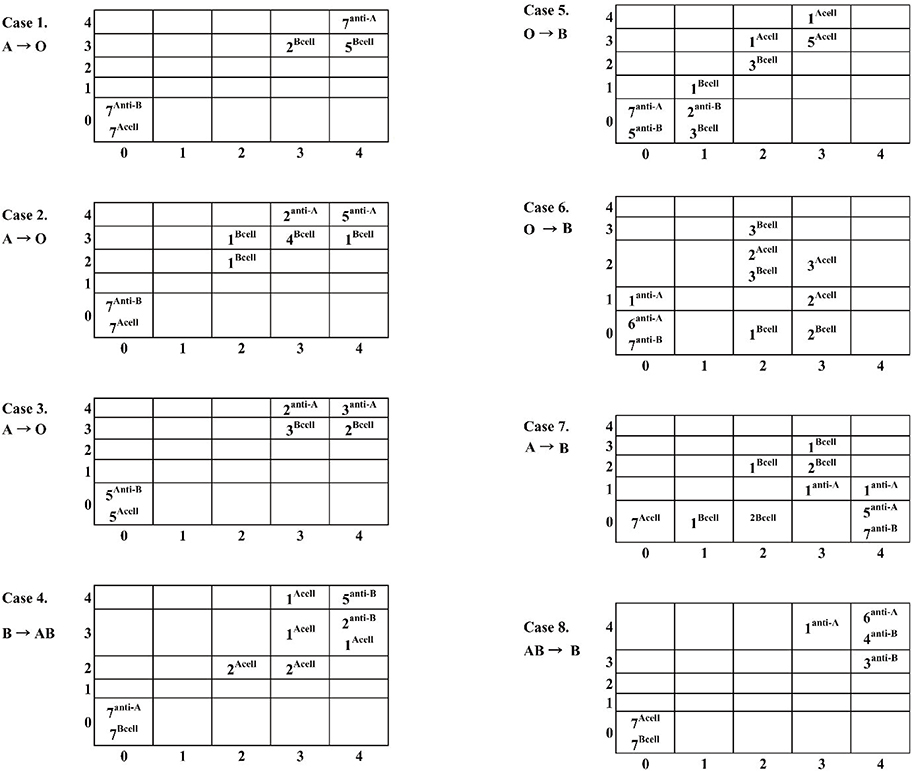
Of the 300 patients enrolled, 87, 73, 79, and 61 had type A, B, O, and AB blood, respectively. The concordance rate was 99.9% for cell typing and 97.0% for serum typing. One discordant case was classified as type B instead of AB, and six discordant serum-typing cases were type A, but classified as type AB. Among the 336 AST samples, the concordance rate was 93.2%. From 136 positive cases, six were discordant. Within the 82 HSCT-treated patients, the concordance rate for ABO blood typing was 92.2%. Among the six discordant cases, DAYMATE M typed four cases as donor type where the standard method typed them as the recipient blood type.
CONCLUSIONS
The DAYMATE M automated immunohematology analyzer performs reliably for ABO and RhD typing, as well as for ASTs and on samples from patients treated with HSCT.
MeSH Terms
Figure
Reference
-
1. Roback JD, Barclay S, Hillyer CD. An automatable format for accurate immunohematology testing by flow cytometry. Transfusion. 2003; 43:918–927.
Article2. Bajpai M, Kaur R, Gupta E. Automation in Immunohematology. Asian J Transfus Sci. 2012; 6:140–144.
Article3. Shin SY, Kwon KC, Koo SH, Park JW, Ko CS, Song JH, et al. Evaluation of two automated instruments for pre-transfusion testing: AutoVue Innova and Techno TwinStation. Korean J Lab Med. 2008; 28:214–220.
Article4. Sturgeon P, Cedergren B, McQuiston D. Automation of routine bloodtyping procedures. Vox Sang. 1963; 8:438–451.5. Lapierre Y, Rigal D, Adam J, Josef D, Meyer F, Greber S, et al. The gel test: a new way to detect red cell antigen-antibody reactions. Transfusion. 1990; 30:109–113.
Article6. Sinor LT. Advances in solid-phase red cell adherence methods and transfusion serology. Transfus Med Rev. 1992; 6:26–31.
Article7. Voak D. The status of new methods for the detection of red cell agglutination. Transfusion. 1999; 39:1037–1040.
Article8. Duguid JK, Bromilow IM. New technology in hospital blood banking. J Clin Pathol. 1993; 46:585–588.
Article9. Casina TS. In search of the Holy Grail: comparison of antibody screening methods. Immunohematology. 2006; 22:196–202.
Article10. Malomgré W, Neumeister B. Recent and future trends in blood group typing. Anal Bioanal Chem. 2009; 393:1443–1451.
Article11. Tanabe K. Interinstitutional variation in the measurement of anti-A/B antibodies: the Japanese ABO-Incompatible Transplantation Committee survey. Transplantation. 2007; 84:S13–S16.
Article12. Validation Task Force of the International Society of Blood Transfusion Working Party on Information Technology. ISBT Guidelines for validation of automated systems in blood establishments. Vox Sang. 2010; 98:1–19.13. Clinical and Laboratory Standards Institute. Validation of automated systems for immunohematological testing before implementation; approved guidelines. I/LA33-A. Wayne, PA: Clinical and Laboratory Standards Institute;2010.14. Fung MK, Grossman BJ, editors. Technical manual. 18th ed. Bethesda: American Association of Blood Banks;2014. p. 371–378.15. Jang MA, Oh JW, Lee ST, Seo JY, Kim DW. Evaluation of the automated blood bank systems Galileo NEO and QWALYS-3 for ABO-RhD typing and antibody screening. Korean J Blood Transfus. 2014; 25:235–242.16. Park Y, Lim J, Ko Y, Kwon K, Koo S, Kim J. Evaluation of IH-1000 for automated ABO-Rh typing and irregular antibody screening. Korean J Blood Transfus. 2012; 23:127–135.17. Jo SY, Lee JM, Kim HL, Sin KH, Lee HJ, Chang CL, et al. Comparative analysis of clinical samples showing weak serum reaction on AutoVue System causing ABO blood typing discrepancies. Ann Lab Med. 2017; 37:117–123.
Article18. Morelati F, Revelli N, Maffei LM, Poretti M, Santoro C, Parravicini A, et al. Evaluation of a new automated instrument for pretransfusion testing. Transfusion. 1998; 38:959–965.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimum Specimen Volume Analysis of ABO/RhD Typing and Unexpected Antibody Screening Using an Automated Immunohematology System DAYmate S
- Advances in Pre-transfusion Testing and Immunohematology
- A Case of Myeloperoxidase Deficiency: its detection on the automated hematology analyzer Technicon H*2
- Comparison of ABO Blood Group Typing between Automated Blood Bank Analyzer IH-500 and Manual Method
- Evaluation of ACL-300 automated coagulation analyzer for the plasmafibrinogen assay