Neurointervention.
2017 Sep;12(2):83-90. 10.5469/neuroint.2017.12.2.83.
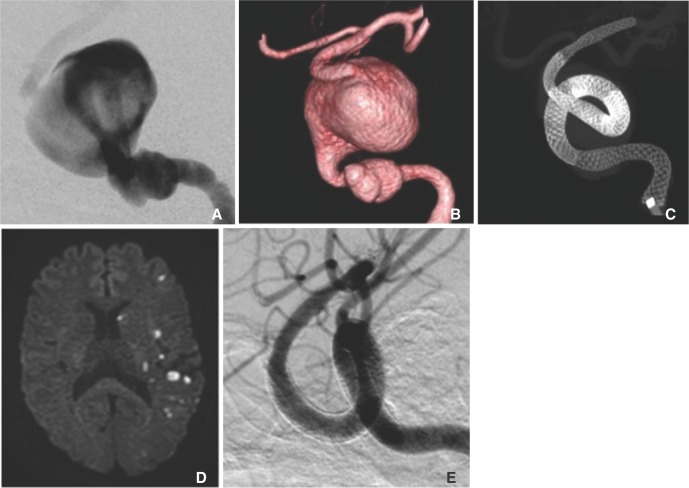
Usefulness of the Pipeline Embolic Device for Large and Giant Carotid Cavernous Aneurysms
- Affiliations
-
- 1Neuroendovascular Therapy Center, Aichi Medical University, Nagakute, Aichi, Japan. miyachi.shigeru.752@mail.aichi-med-u.ac.jp
- 2Department of Neurosurgery and Neuroendovascular Therapy, Osaka Medical College, Takatsuki, Osaka, Japan.
- 3Ohnishi Neurosurgical Hospital, Akashi, Hyogo, Japan.
- KMID: 2389500
- DOI: http://doi.org/10.5469/neuroint.2017.12.2.83
Abstract
- PURPOSE
Conventional coil embolization for large carotid cavernous aneurysms (CCAs) has limited utility due to its inability to prevent recurrences and reduce mass effect. Trapping of the parent artery may have a risk of ischemic complications due to intracranial perfusion disorders. We successfully treated 24 patients with large CCAs using a flow diverter (Pipelineâ„¢ embolic device: PED), and this report discusses the safety and efficacy of this method.
MATERIALS AND METHODS
Twenty four patients (23 females, mean age 71.5 years old) with large CCAs, including 6 giant CCAs, were treated with a PED over three years. Under sufficient dual anti-platelet management, the PED was deployed over the orifice of the aneurysm. Two patients required multiple telescoping stents. Clinical and radiological states were checked with MRI at 1, 3 and 6 months post-surgically. Angiographic follow-up was performed at 6 months.
RESULTS
In all patients, PED was appropriately deployed. Stagnation of contrast with eclipse signs was observed post-angiogram in 21 cases. One patient requiring 5 telescoping stents experienced temporary ischemic symptoms. Fourteen patients experienced improvement of ocular motor impairment deficiency, including 6 patients who recovered. Angiograms at 6 months follow-up showed complete occlusion in 63% (12/19) of patients, and MRI showed reduction of aneurysm volume in 89% (17/19) of patients.
CONCLUSION
Flow diverters for large CCAs showed promising clinical and radiological efficacy. They can shrink the aneurysm and improve symptoms without sacrificing the parent artery. It will be necessary to summarize the cases and to verify the long-term results.
Keyword
MeSH Terms
Figure
Reference
-
1. van Rooij WJ. Endovascular treatment of cavernous sinus aneurysms. AJNR Am J Neuroradiol. 2012; 33:323–326. PMID: 22033713.
Article2. Chalouhi N, Tjoumakaris S, Dumont AS, Gonzalez LF, Randazzo C, Starke RM, et al. Treatment of posterior circulation aneurysms with the pipeline embolization device. Neurosurgery. 2013; 72:883–889. PMID: 23407289.
Article3. Lylyk P, Miranda C, Ceratto R, Ferrario A, Scrivano E, Luna HR, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. 2009; 64:632–642. PMID: 19349825.4. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 32:34–40. PMID: 21148256.
Article5. Saatci I, Yavuz K, Ozer C, Geyik S, Cekirge HS. Treatment of intra- cranial aneurysms using the pipeline flow-diverter embolization device: a single-center experience with long-term follow-up results. AJNR Am J Neuroradiol. 2012; 33:1436–1446. PMID: 22821921.6. Miyachi S. Tactics, Techniques and Spirits of Neuroendovascular Therapy. - Miyachi's style, Chapter Skill-A Aneurysm -flow diverter-. Osaka: Medica Shuppan;2015. p. 164–169. (in Japanese).7. Roy D, Milot G, Raymond J. Endovascualar treatment of unruptured aneurysms. Stroke. 2001; 32:1998–2004. PMID: 11546888.8. Puffer RC, Piano M, Lanzino G, Valvassori L, Kallmes DF, Quilici L, et al. Treatment of cavernous sinus aneurysms with flow diversion: results in 44 patients. AJNR Am J Neuroradiol. 2014; 35:948–951. PMID: 24356675.
Article9. Zanaty M, Chalouhi N, Starke RM, Barros G, Saigh MP, Schwartz EW, et al. Flow diversion versus conventional treatment for carotid cavernous aneurysms. Stroke. 2014; 45:2656–2661. PMID: 25052318.
Article10. Briganti F, Napoli M, Tortora F, Solari D, Bergui M, Boccardi E, et al. Italian multicenter experience with flow-diverter devices for intracranial unruptured aneurysm treatment with periprocedural complications--a retrospective data analysis. Neuroradiology. 2012; 54:1145–1152. PMID: 22569955.
Article11. O'Kelly CJ, Spears J, Chow M, Wong J, Boulton M, Weill A, et al. Canadian experience with the pipeline embolization device for repair of unruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2013; 34:381–387. PMID: 22859284.12. Lanzino G, Crobeddu E, Cloft HJ, Hanel R, Kallmes DF. Efficacy and safety of flow diversion for paraclinoid aneurysms: a matched-pair analysis compared with standard endovascular approaches. AJNR Am J Neuroradiol. 2012; 33:2158–2161. PMID: 22790243.
Article13. Chalouhi N, Tjoumakaris S, Starke RM, Gonzalez LF, Randazzo C, Hasan D, et al. Comparison of flow diversion and coiling in large unruptured intracranial saccular aneurysms. Stroke. 2013; 44:2150–2154. PMID: 23723311.
Article14. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; 267:858–868. PMID: 23418004.
Article15. Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonafé A, Cekirge S, et al. International retrospective study of the Pipeline embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol. 2015; 36:108–115. PMID: 25355814.
Article16. Raymond J, Darsaut TE, Kotowski M, Makoyeva A, Gevry G, Berthelet F, et al. Thrombosis heralding aneurysmal rupture: an exploration of potential mechanisms in a novel giant swine aneurysm model. AJNR Am J Neuroradiol. 2013; 34:346–353. PMID: 23153870.
Article17. Maruta K, Aoki A, Omoto T, Iizuka H, Kawaura H. The Effect of Steroid Therapy on Postoperative Inflammatory Response after Endovascular Abdominal Aortic Aneurysm Repair. Ann Vasc Dis. 2016; 9:168–172. PMID: 27738457.
Article18. Miyachi S, Ohnishi H, Hiramatsu R, Izumi T, Matsubara N, Kuroiwa T. Innovations in Endovascular Treatment Strategies for Large Carotid Cavernous Aneurysms-The Safety and Efficacy of a Flow Diverter. J Stroke Cerebrovasc Dis. 2017; 26:1071–1080. PMID: 28238529.
Article19. Guédon A, Clarençon F, Di Maria F, Rosso C, Biondi A, Gabrieli J, et al. Very late ischemic complications in flow-diverter stents: a retrospective analysis of single-center series. J Neurosurg. 2016; 125:929–935. PMID: 26824382.20. Miyachi S, Ishii A. Development of a Pipeline-classic Type to Flex: Points of Improvement and Precautions for Use. J Neuroendovascular Ther. 2016; 26:1071–1080.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment for Giant Fusiform Aneurysm Located in the Cavernous Segment of the Internal Carotid Artery Using the Pipeline Embolization Device
- Pipeline Embolization Device for Giant Internal Carotid Artery Aneurysms: 9-Month Follow-Up Results of Two Cases
- Balloon Anchor Technique for Pipeline Embolization Device Deployment Across the Neck of a Giant Intracranial Aneurysm
- Quantitative Computed Tomographic Volumetry after Treatment of a Giant Intracranial Aneurysm with a Pipeline Embolization Device
- Flow diverter stenting for intracranial aneurysms in the pediatric population: Two case reports and literature review