Yonsei Med J.
2017 May;58(3):668-671. 10.3349/ymj.2017.58.3.668.
Quantitative Computed Tomographic Volumetry after Treatment of a Giant Intracranial Aneurysm with a Pipeline Embolization Device
- Affiliations
-
- 1Department of Radiology, Chung-Ang University Hospital, Seoul, Korea. flightdr61@cau.ac.kr
- 2Department of Neurosurgery, Chung-Ang University Hospital, Seoul, Korea.
- KMID: 2419130
- DOI: http://doi.org/10.3349/ymj.2017.58.3.668
Abstract
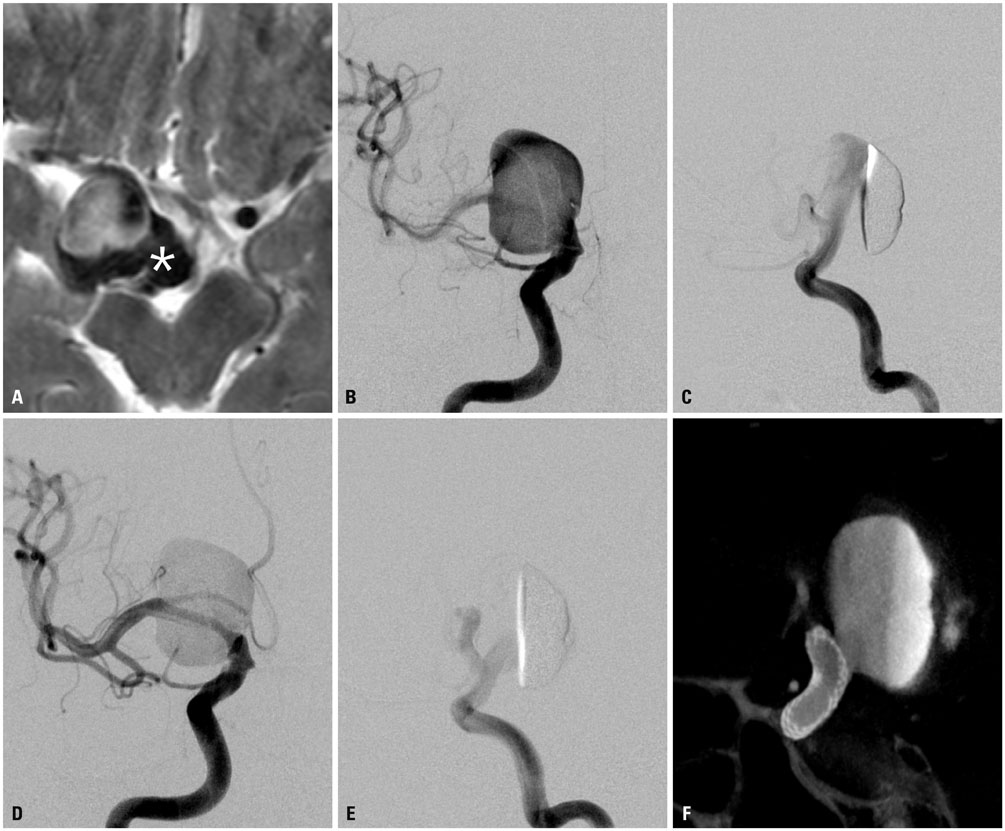
- Recently developed flow diverters, such as the pipeline embolization device (PED), allow for safe and efficacious treatment of giant intracranial aneurysms, with high occlusion rates and a low incidence of complications. However, incomplete obliteration after PED treatment may lead to aneurysm regrowth and delayed rupture. Herein, we report a case of a partially thrombosed giant aneurysm of the cavernous internal carotid artery that showed progressive recanalization at 1-3 months after application of a PED. We monitored inflow volume in the aneurysm by computed tomographic angiography (CTA) and computed tomographic volumetric imaging (CTVI). Based on the imaging results, rather than applying additional PED, we decided to make the switch from a dual antiplatelet medication to low-dose aspirin alone at 3 months after the treatment; complete obliteration of the aneurysm was noted at 21 months. Similar to the findings in this unusual case, CTA and CTVI may be useful follow-up methods for optimal management of patients with giant intracranial aneurysms after PED treatment.
Keyword
MeSH Terms
-
Adult
Aged
Anticoagulants/therapeutic use
Aspirin/therapeutic use
Carotid Artery, Internal/diagnostic imaging
Embolization, Therapeutic/adverse effects/*instrumentation/*methods
Female
Humans
Intracranial Aneurysm/diagnostic imaging/*therapy
Male
Middle Aged
Platelet Aggregation Inhibitors/therapeutic use
Stents
Thrombosis/*diagnostic imaging/drug therapy/etiology
Tomography, X-Ray Computed/*methods
Treatment Outcome
Anticoagulants
Platelet Aggregation Inhibitors
Aspirin
Figure
Reference
-
1. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; 267:858–868.
Article2. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke. 2013; 44:442–447.
Article3. Kallmes DF, Ding YH, Dai D, Kadirvel R, Lewis DA, Cloft HJ. A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke. 2007; 38:2346–2352.
Article4. Lieber BB, Stancampiano AP, Wakhloo AK. Alteration of hemodynamics in aneurysm models by stenting: influence of stent porosity. Ann Biomed Eng. 1997; 25:460–469.
Article5. Makkar RR, Eigler NL, Kaul S, Frimerman A, Nakamura M, Shah PK, et al. Effects of clopidogrel, aspirin and combined therapy in a porcine ex vivo model of high-shear induced stent thrombosis. Eur Heart J. 1998; 19:1538–1546.
Article6. Krings T, Alvarez H, Reinacher P, Ozanne A, Baccin CE, Gandolfo C, et al. Growth and rupture mechanism of partially thrombosed aneurysms. Interv Neuroradiol. 2007; 13:117–126.
Article7. Martin AJ, Hetts SW, Dillon WP, Higashida RT, Halbach V, Dowd CF, et al. MR imaging of partially thrombosed cerebral aneurysms: characteristics and evolution. AJNR Am J Neuroradiol. 2011; 32:346–351.
Article8. Rouchaud A, Brinjikji W, Lanzino G, Cloft HJ, Kadirvel R, Kallmes DF. Delayed hemorrhagic complications after flow diversion for intracranial aneurysms: a literature overview. Neuroradiology. 2016; 58:171–177.
Article9. Hampton T, Walsh D, Tolias C, Fiorella D. Mural destabilization after aneurysm treatment with a flow-diverting device: a report of two cases. J Neurointerv Surg. 2011; 3:167–171.
Article10. Ikeda H, Ishii A, Kikuchi T, Ando M, Chihara H, Arai D, et al. Delayed aneurysm rupture due to residual blood flow at the inflow zone of the intracranial paraclinoid internal carotid aneurysm treated with the Pipeline embolization device: histopathological investigation. Interv Neuroradiol. 2015; 21:674–683.
Article11. Siddiqui AH, Kan P, Abla AA, Hopkins LN, Levy EI. Complications after treatment with pipeline embolization for giant distal intracranial aneurysms with or without coil embolization. Neurosurgery. 2012; 71:E509–E513.
Article12. Carneiro A, Rane N, Küker W, Cellerini M, Corkill R, Byrne JV. Volume changes of extremely large and giant intracranial aneurysms after treatment with flow diverter stents. Neuroradiology. 2014; 56:51–58.
Article13. National Research Council, Division on Earth and Life Studies, Board on Radiation Effects Research, Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Washington, DC: National Academies Press;2006.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pipeline Embolization Device for Giant Internal Carotid Artery Aneurysms: 9-Month Follow-Up Results of Two Cases
- A Case of Migration of Pipeline Embolization Device Causing Rupture during Treatment of an Unruptured Vertebral Artery Dissecting Aneurysm
- Treatment for Giant Fusiform Aneurysm Located in the Cavernous Segment of the Internal Carotid Artery Using the Pipeline Embolization Device
- Balloon Anchor Technique for Pipeline Embolization Device Deployment Across the Neck of a Giant Intracranial Aneurysm
- Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm